A
A pattern See pattern, A.
abathic distance See plane, apparent frontoparallel.
Abbé’s condenser See condenser, Abbé’s.
Abbé’s condition See sin condition.
Abbé’s number See constringence.
Abbé’s refractometer See refractometer.
abducens muscle See muscle, lateral rectus.
abducens nerve See nerve, abducens.
abducens nerve palsy See paralysis of the sixth nerve.
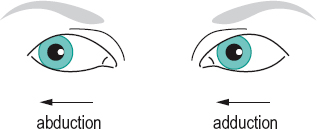
abduct To turn away from the midline, as when the eye rotates outward.
abduction Outward rotation of an eye, that is away from the midline.
See duction; syndrome, Duane’s.
abductors Extraocular muscles that move the eye outward, such as the lateral rectus, the inferior oblique and the superior oblique.
aberrant regeneration An abnormal regeneration process following paralysis or paresis of the fibres of the third cranial nerve (oculomotor) in which the upper lid fails to follow the eye on downward gaze or even retracts on downward gaze or adduction, with occasional contraction of the pupil. Syn. pseudo-von Graefe sign.
aberration An optical defect in which the rays from a point object do not form a perfect point after passing through an optical system.
See astigmatism, oblique; coma; curvature of field; distortion.
axial chromatic a. See aberration, longitudinal chromatic.
lateral chromatic a. Defect of an optical system (eye, lens, prism, etc.) in which the size of the image of a point object is extended by a coloured fringe, due to the unequal refraction of different wavelengths (dispersion). Syn. chromatic difference of magnification; transverse chromatic aberration (TCA).
See dispersion; doublet.
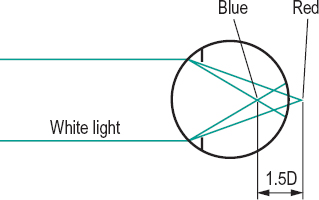
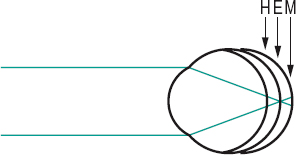
longitudinal chromatic a. (LCA) Defect of an optical system (eye, lens, prism, etc.) due to the unequal refraction of different wavelengths (dispersion) which results in an extended image along the optical axis. In the eye, blue rays are focused in front of the retina (by about 1 D) and red rays slightly behind the retina (0.25–0.5 D) when relaxed. When the eye is accommodated for a near target, blue rays tend to be focused near the retina and red rays are focused behind the retina (1 D), because of a lag of accommodation usually occurring when viewing near targets (Fig. A1). Syn. axial chromatic aberration.
See chromoretinoscopy; chromostereopsis; constringence; dispersion; doublet; lens, achromatizing; pigment, macular; test, duochrome.
monochromatic a. Defect of an optical system (eye, lens, prism, etc.) occurring for a single wavelength of light. There are five such aberrations: spherical aberration, coma, curvature of field, oblique astigmatism and distortion. Syn. Seidel aberration.
negative a. See aberration, spherical.
oblique a . Aberration induced by a point object off the optical axis of the system. These comprise coma, curvature of field, distortion and oblique astigmatism.
positive a. See aberration, spherical.
prism a . Additional effects of a prism on light, in addition to the expected change in direction of light. These effects include different magnifications, curvature of field and chromatic aberration.
Seidel a. See aberration, monochromatic.
spherical a . Defect of an optical system due to a variation in the focusing between peripheral and paraxial rays. The larger the pupil size, the greater the difference in focusing between the two rays. In the gaussian theory, the focus of the optical system is attributed to the paraxial rays. The distance, in dioptres, between the focus of the paraxial rays and the peripheral rays represents the amount of longitudinal spherical aberration of the system. When the peripheral rays are refracted more than the paraxial rays, the aberration is said to be positive or undercorrected. When the peripheral rays are refracted less than the paraxial rays the aberration is said to be negative or overcorrected. The relaxed human eye has a small amount of positive spherical aberration (up to 1 D for a pupil of 8 mm diameter) (Fig. A2).
See caustic; lens, aplanatic; theory, gaussian.
transverse chromatic a. See aberration, lateral chromatic.
wavefront a . The amount of deviation between an output wavefront emanating from an optical system and a conceptualized ideal (reference) wavefront. The specification of the deviation (or error) is usually fitted with a normalized Zernike expansion. The measurement of this aberration can be done subjectively or objectively (e.g. with an aberrometer based on the Hartmann–Shack principle). The method (called aberrometry) has been applied clinically to measure the aberrations displayed by optical systems, such as the eye, the eye with a correction, contact lenses (in vitro or in situ), intraocular lenses (in vitro or in situ), in corneal refractive surgery, cataract, etc. (Fig. A3). Syn. wavefront error.
aberrometry See aberration, wavefront.
aberroscope Instrument for observing aberration. Such an instrument was designed by Tscherning to measure his own spherical aberration. It consists of a planoconvex lens with a grid made up of squares ruled on its plane surface.
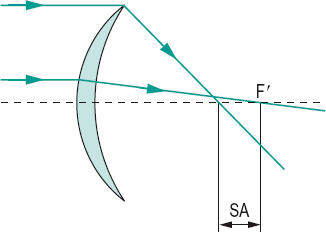
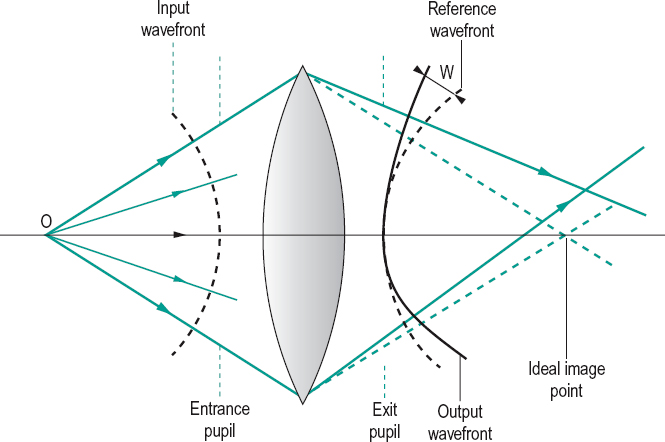
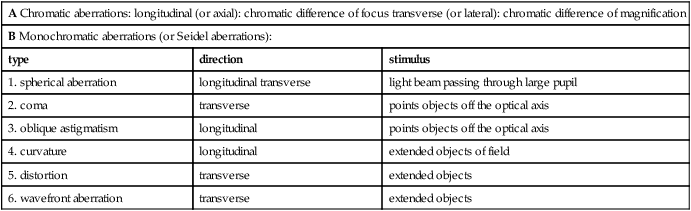
Table A1
Aberrations of the eye
| A Chromatic aberrations: longitudinal (or axial): chromatic difference of focus transverse (or lateral): chromatic difference of magnification | ||
| B Monochromatic aberrations (or Seidel aberrations): | ||
| type | direction | stimulus |
| 1. spherical aberration | longitudinal transverse | light beam passing through large pupil |
| 2. coma | transverse | points objects off the optical axis |
| 3. oblique astigmatism | longitudinal | points objects off the optical axis |
| 4. curvature | longitudinal | extended objects of field |
| 5. distortion | transverse | extended objects |
| 6. wavefront aberration | transverse | extended objects |
abetalipoproteinaemia See syndrome, Bassen–Kornzweig.
ablatio retinae See retinal detachment.
ablation A procedure in which a tissue or body part is removed or destroyed by surgery, radiation or photocoagulation. Example: LASIK.
ablepharon See ablephary.
ablephary Congenital absence, complete or partial, of the eyelids. Syn. ablepharon.
ablepsia See blindness.
ablepsy See blindness.
Abney’s law; phenomenon See under the nouns.
abnormal (anomalous) retinal correspondence See retinal correspondence, abnormal.
abrasion, corneal See corneal abrasion.
abrasive Granular substance used in lens grinding, such as corundum (aluminium oxide), carborundum, etc.
See roughing; smoothing; surfacing.
abscess An accumulation of pus located in infected tissue.
absorbance A measure of absorption equal to the logarithm to the base 10 of the reciprocal of the transmittance T, for a specified wavelength and expressed as A = –log10 T. Syn. optical density.
See density, optical; transmittance.
absorption Transformation of radiant energy into a different form of energy, usually heat, as it passes through a medium. Light that is absorbed is neither transmitted nor reflected. It may, however, be re-emitted as light of another wavelength as, for example, ultraviolet radiation is converted into visible radiation on absorption by a luminescent material. A substance that absorbs all radiations is called a black body.
See absorbance; density, optical; fluorescence.
absorptive lens See lens, absorptive.
AC/A ratio Ratio of the accommodative convergence AC (in prism dioptres) to the stimulus to accommodation A (in dioptres). The most common method of determining this ratio is by the gradient method (or gradient test) in which the phoria at near is measured after changing the accommodation with a spherical lens (usually +1.00 D or –1.00 D) placed in front of the two eyes. It is expressed as
< ?xml:namespace prefix = "mml" />
where α is the phoria at near, and α’ is the phoria at the same distance but through a lens of power F. The deviation is measured in prism dioptres, with + for esodeviation and – for exodeviation. Example: if the initial phoria is 4 Δ exo and 8 Δ exo when a lens of +1.00 D is placed in front of the eyes, the AC/A ratio is equal to
The average AC/A ratio is about 4 in young adults and tends to decline slightly with age. The gradient is not affected by proximal convergence, as the target distance and size are relatively constant. Syn. gradient. Another method of determining the AC/A ratio (often called the heterophoria method) compares the phoria measured at distance and at near. It is expressed as
where PD is the interpupillary distance in cm, N the deviation at near, D the deviation at distance and K the near fixation distance in dioptres. Example: A patient has a PD of 70 mm, a distance phoria of 4 Δ eso and a near phoria of 8 Δ exo at 33.3 cm from the eyes, the AC/A ratio is equal to
See convergence, accommodative; convergence, proximal; dioptre, prism.
acanthamoeba keratitis See keratitis, acanthamoeba.
acanthocytosis See syndrome, Bassen–Kornzweig.
acanthosis nigricans A rare skin disorder presenting numerous superficial, pigmented papillomatous growths on various parts of the body. Ocular manifestations are primarily papillomatous lesions of the lid margins, which may be so extensive as to cause punctal occlusion, as well as papillary conjunctivitis. Syn. keratosis nigricans.
accessory lacrimal glands See glands, accessory lacrimal; glands of Krause; glands of Wolfring.
accommodation Adjustment of the dioptric power of the eye. It is generally involuntary and made to see objects clearly at any distance. In man (and primates), this adjustment is brought about by a change in the shape of the crystalline lens. In some animals this adjustment occurs either as a result of an anteroposterior movement of the crystalline lens, or of an alteration in the curvature of the cornea.
See aniso-accommodation; muscle, ciliary; reflex, accommodative; theory, Fincham’s; theory, Helmholtz’s of accommodation.
amplitude of a. The maximum amount of accommodation A that the eye can exert. It is expressed in dioptres, as the difference between the far point and the near point measured with respect either to the spectacle plane or the corneal apex or some other reference point. Thus,

where B is the near point vergence and K is the far point vergence. A is always positive. In the emmetropic eye, A = – B, because the far point is at infinity and K = 0. So, if the near point of an emmetrope is at 25 cm from the spectacle plane, the amplitude of accommodation is equal to – [–1/(25 × 10–2)] = 4 D. The amplitude of accommodation declines from about 14 D at age 10 to about 0.5 D at age 60 (although the measured value is usually higher due to the depth of focus of the eye).
See method, minus lens; method, push-up.
astigmatic a. Postulated unequal accommodation along different meridians of the eye attributed to a differential action of the ciliary muscle which would lead to a difference in the curvature of the surfaces of the crystalline lens along different meridians. Syn. meridional accommodation.
Table A2
Mean amplitude of accommodation as a function of age, in Caucasians (the plane of reference is the spectacle plane)
| age (years) | Duane (N = 2000 subjects, push-up method) | Turner (Nh = 500 subjects, push-out method) |
| 10 | 13.5 | 13.0 |
| 15 | 12.5 | 10.6 |
| 20 | 11.5 | 9.5 |
| 25 | 10.5 | 7.9 |
| 30 | 8.9 | 6.6 |
| 35 | 7.3 | 5.75 |
| 40 | 5.9 | 4.4 |
| 45 | 3.7 | 2.5 |
| 50 | 2.0 | 1.6 |
| 55 | 1.3 | 1.1 |
| 60 | 1.2 | 0.7 |
| 65 | 1.1 | 0.6 |
| 70 | 1.0 | 0.6 |
closed-loop a. Accommodation response to visual stimuli in normal viewing conditions.
See accommodation, open-loop.
components of a . The process of accommodation is assumed to involve four components: reflex, vergence (convergence), proximal and tonic accommodation (also called resting state of accommodation).
See accommodation, convergence; accommodation, proximal; accommodation, reflex; accommodation, resting state of.
consensual a. Accommodation occurring in one eye when the other eye has received the dioptric stimulus.
convergence a. 1. Accommodation induced directly by a change in convergence. 2. That component of accommodation induced by the binocular disparity of the retinal images. Syn. vergence accommodation.
correction induced a. Ocular accommodation induced when changing from spectacles to contact lenses in near vision. Spectacles induce less accommodation in myopes and more accommodation in hyperopes than that exerted by an emmetrope fixating at a given distance. Contact lenses do not induce any different accommodation than that required for a given distance. Consequently, myopes require more accommodation and hyperopes less accommodation when they transfer from spectacles to contact lenses. However, this change in accommodative demand is accompanied by a similar change in convergence, so that a myope transferring to contact lenses accommodates and converges more than with spectacles and the reverse applies for a hyperope.
See convergence, correction induced.
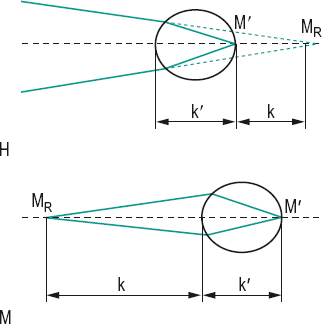
far point of a. A point in space conjugate with the retina (more specifically the foveola) when the accommodation is relaxed. In emmetropia, the far point is at infinity; in myopia, it is at a finite distance in front of the eye; in hyperopia, it is a virtual point behind the eye (Fig. A4). Syn. far point of the eye; punctum remotum.
ill-sustained a. See accommodative insufficiency.
inert a. See accommodative infacility.
insufficiency of a. See accommodative insufficiency.
lag of a. 1. The amount by which the accommodative response of the eye is less than the dioptric stimulus to accommodation, as usually occurs when fixating an object at near. It could be due to uncorrected hyperopia or indicate accommodative insufficiency. Absence of an accommodative lag may indicate latent hyperopia. Syn. lazy lag of accommodation. 2. The condition occurring in dynamic retinoscopy in which the neutral point is situated further from the eyes than is the retinoscopic target.
lead of a. The amount by which the accommodative response of the eye is greater than the dioptric stimulus to accommodation, as occurs when fixating at distance, in a few individuals. It can also occur as a result of a spasm of accommodation.
mechanism of a . Process by which the eye focuses onto an object. It does so by contracting the ciliary muscle which releases the tension on the zonular fibres, allowing the elastic lens capsule to increase its curvature, especially that of the front surface. Along with these changes are an increase in the thickness of the lens, a decrease in its equatorial diameter and a reduction in pupil size. The ciliary muscle is controlled by the parasympathetic system, which is triggered by an out of focus retinal image.
See accommodation, convergence; accommodation, proximal; accommodative response; muscle, ciliary; reflex, near.
meridional a. See accommodation, astigmatic.
microfluctuations of a. Involuntary variations in the contraction of the intraocular muscles responsible for accommodation and resulting in changes of about 0.1–0.5 D with a frequency of 0.5–2.5 Hz.
near point of a. The nearest point in space that is conjugate with the foveola when exerting the maximum accommodative effort. Syn. punctum proximum.
See method, push-up; rule, near point; sphere, near point; test, Scheiner’s.
negative a. 1. A relaxation of accommodation below the apparent zero level or when shifting from near to distance vision. 2. See accommodation, relative amplitude of.
objective a . Accommodation measured without the subject’s judgment. This is accomplished by dynamic retinoscopy, by autorefractors or by visually evoked cortical potentials. The term is sometimes used incorrectly to refer to the amplitude of accommodation without the influence of the depth of focus (e.g. as measured by stigmatoscopy).
See accommodation, subjective; optometer; potential, evoked cortical; retinoscopy, dynamic; stigmatoscopy.
ocular a. The amplitude of accommodation referred to the front surface of the cornea. Symbol: A.
See accommodation, spectacle.
open-loop a . Accommodative response occurring without the usual stimulus to accommodation, such as a blurred retinal image. In these conditions, the accommodative system of the eye tends to return to its position of rest
Table A3
Relationship between viewing distance and spectacle and ocular accommodation of a contact lens wearer and of four corrected hyperopes (with thin spectacle lenses). The vertex distance was 14 mm and ocular accommodation was calculated using the formula A = K – B. The ocular accommodation exerted by a contact lens wearer is the same for all refractive errors and equal to that of an emmetrope
| distance from spectacle lens (cm) | spectacle accom. (D) | ocular accom. (D) of contact lens wearer | ocular accom. (D) of hyperopes | |||
| +2 | +4 | +6 | +8 | |||
| 100 | 1.00 | 0.99 | 1.04 | 1.11 | 1.17 | 1.25 |
| 67 | 1.49 | 1.46 | 1.55 | 1.64 | 1.74 | 1.86 |
| 50 | 2.00 | 1.95 | 2.06 | 2.18 | 2.31 | 2.46 |
| 40 | 2.50 | 2.42 | 2.55 | 2.71 | 2.87 | 3.05 |
| 33 | 3.03 | 2.91 | 3.07 | 3.25 | 3.45 | 3.67 |
| 25 | 4.00 | 3.79 | 4.00 | 4.24 | 4.49 | 4.77 |
| 20 | 5.00 | 4.67 | 4.94 | 5.22 | 5.54 | 5.88 |
| 16 | 6.25 | 5.75 | 6.07 | 6.42 | 6.80 | 7.22 |
| 14 | 7.14 | 6.49 | 6.86 | 7.25 | 7.68 | 8.14 |
| 12 | 8.33 | 7.46 | 7.88 | 8.32 | 8.81 | 9.34 |
| 10 | 10.00 | 8.77 | 9.25 | 9.77 | 10.34 | 10.95 |
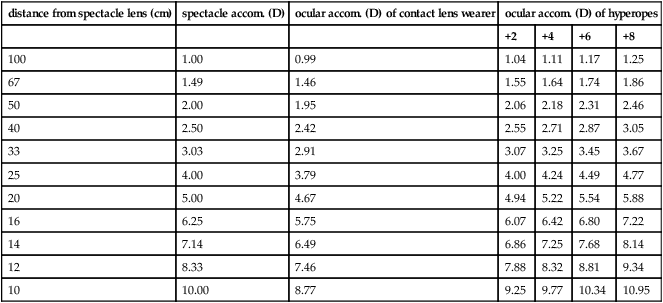
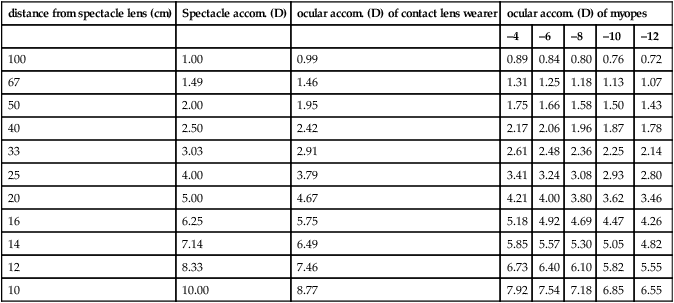
Table A4
Relationship between viewing distance and spectacle and ocular accommodation of a contact lens wearer and of five corrected myopes (with thin spectacle lenses). The vertex distance was 14 mm and ocular accommodation was calculated using the formula A = K – B. The ocular accommodation exerted by a contact lens wearer is the same for all refractive errors and equal to that of an emmetrope
| distance from spectacle lens (cm) | Spectacle accom. (D) | ocular accom. (D) of contact lens wearer | ocular accom. (D) of myopes | ||||
| –4 | –6 | –8 | –10 | –12 | |||
| 100 | 1.00 | 0.99 | 0.89 | 0.84 | 0.80 | 0.76 | 0.72 |
| 67 | 1.49 | 1.46 | 1.31 | 1.25 | 1.18 | 1.13 | 1.07 |
| 50 | 2.00 | 1.95 | 1.75 | 1.66 | 1.58 | 1.50 | 1.43 |
| 40 | 2.50 | 2.42 | 2.17 | 2.06 | 1.96 | 1.87 | 1.78 |
| 33 | 3.03 | 2.91 | 2.61 | 2.48 | 2.36 | 2.25 | 2.14 |
| 25 | 4.00 | 3.79 | 3.41 | 3.24 | 3.08 | 2.93 | 2.80 |
| 20 | 5.00 | 4.67 | 4.21 | 4.00 | 3.80 | 3.62 | 3.46 |
| 16 | 6.25 | 5.75 | 5.18 | 4.92 | 4.69 | 4.47 | 4.26 |
| 14 | 7.14 | 6.49 | 5.85 | 5.57 | 5.30 | 5.05 | 4.82 |
| 12 | 8.33 | 7.46 | 6.73 | 6.40 | 6.10 | 5.82 | 5.55 |
| 10 | 10.00 | 8.77 | 7.92 | 7.54 | 7.18 | 6.85 | 6.55 |
(or tonic accommodation). Examples: looking at an empty field; looking through a very small artificial pupil (0.5 mm or less).
See accommodation, closed-loop.
paralysis of a. Total or partial loss of accommodation due to paralysis of the ciliary muscle.
positive a. Normal accommodation that occurs when looking from a distant to a near object.
proximal a. That component of accommodation initiated by the awareness of a near object. Syn. psychic accommodation.
See accommodation, components of; accommodation, resting state of.
psychic a. See accommodation, proximal.
range of a. The linear distance between the far point and the near point. Part of the range of accommodation is virtual in the case of the hypermetrope.
reflex a. An adjustment of the refractive state of the eye stimulated by blur and aimed at reducing blur. It may be initiated when the eye changes fixation from far to near, or it may be induced by convergence. The amount of reflex accommodation rarely exceeds 2 D.
See accommodation, components of; reflex, near.
relative amplitude of a. The total amount of accommodation which the eye can exert while the convergence of the eyes is fixed. It can be positive (using concave lenses until the image blurs). This is called positive relative accommodation (PRA). It can be negative (using convex lenses until the image blurs). This is negative relative accommodation (NRA).
See zone of clear, single, binocular vision.
reserve a. See addition, near.
resting state of a. The passive state of accommodation of the eye in the absence of a stimulus, i.e. when the eye is either in complete darkness, or looking at a bright empty field. In this condition, the prepresbyopic eye is usually focused at an intermediate point (about 80 cm on average, although there are large variations), that is, the emmetropic eye becomes myopic. This is presumably due to a balance between a parasympathetic innervation to the circular fibres of the ciliary muscle and a sympathetic innervation to the longitudinal fibres of the ciliary muscle. Thus, the resting state of accommodation would correspond to a position of equilibrium between the two systems. Accommodation from this state to the near point of accommodation would be the response to parasympathetic stimulation; and accommodation from this state to the far point of accommodation would be the response to sympathetic stimulation. Syn. dark accommodation; dark focus (these terms are not strictly synonymous but as they have been found to correlate well, they have been adopted as synonyms); tonic accommodation (TA).
See hysteresis, accommodative; myopia, night; myopia, space; tonus; vergence, tonic.
spasm of a. Involuntary contraction of the ciliary muscle producing excess accommodation. It may be constant, intermittent, unilateral or bilateral. Patients typically complain of blurred distance vision and sometimes changes in perceived size of objects, and discomfort. If the patient is a low hyperope or emmetrope, it will give rise to pseudomyopia (false myopia, hypertonic myopia, spurious myopia). Diagnosis is facilitated by cycloplegic refraction to rule out latent hyperopia. Although spasm of accommodation can be a separate entity, it is often associated with excessive convergence (esotropia) and miosis; this is referred to as spasm of the near reflex. Management includes removal of the primary cause, if possible (e.g. uveitis, or patient taking parasympathomimetic drugs), correction of the underlying refraction, if any, changes in the visual working conditions, positive lenses, accommodative facility exercises and, only rarely, cycloplegics.
See accommodative facility; metamorphopsia.
spectacle a. The amplitude of accommodation referred to the spectacle plane. Symbol: As.
See accommodation, ocular.
subjective a. Measurement of the accommodation based on the subject’s judgements, such as the push-up or push-out method or the minus lens method.
See accommodation, objective; method, minus lens; method, push-up.
tonic a. See accommodation, resting state of.
vergence a. See accommodation, convergence.
accommodative Relating to accommodation.
accommodative astigmatism See astigmatism, accommodative.
accommodative convergence See convergence, accommodative.
accommodative convergence/accommodation ratio See AC/A ratio.
accommodative excess A condition in which the subject exerts more accommodation than required for the visual stimulus, or is unable to relax accommodation. It may be due to uncorrected hyperopia, very prolonged near work, emotional problems, spasm of accommodation, uveitis, trigeminal neuralgia, syphilis, meningitis, head trauma, or the side effect of some pharmaceutical agent (e.g. a miotic drug). It is usually associated with convergence excess. The subject reports blurred vision at distance, asthenopia and often headaches. Treatment commonly includes plus lenses and facility exercises, besides therapy of the underlying cause. Syn. hyperaccommodation. Note: spasm of accommodation is one aspect of the general condition of accommodative excess, although some authors consider this term a synonym.
See accommodation, spasm of; accommodative facility; convergence excess.
accommodative demand See accommodation, correction induced.
accommodative esotropia See strabismus, accommodative.
accommodative facility Ability of the eye/s to focus on stimuli at various distances and in different sequences in a given period of time. Clinically, this is measured either monocularly or binocularly, usually by having the subject fixate a small target alternately through plus and minus lenses, which are interchanged as soon as the target appears clear. The operation is repeated many times and the results are commonly presented in cycles per minute (one cycle indicates that both plus and minus lenses have been cleared). Syn. accommodative rock.
See accommodative insufficiency; lens flippers.
accommodative fatigue See accommodative insufficiency.
accommodative inertia Difficulty in altering the accommodative response, such that the latency and completion time of the process are delayed. It may occur as a result of prolonged near vision tasks. Orthoptic exercises may help in this condition.
accommodative hysteresis See hysteresis, accommodative.
accommodative infacility A condition in which there is a slowness in changing from one level of accommodation to another. Patients may complain of transitory blur. It may be due to diabetes, Graves’ disease, measles or the side effects of some drugs. It is commonly associated with asthenopia. Treatment is aimed at the primary cause, but plus lenses and, especially, accommodative facility exercises are usually prescribed. Syn. inert accommodation.
accommodative insufficiency Insufficient amplitude of accommodation that is unequivocally below the appropriate level for the age. It may be due to extreme fatigue, influenza, high stress, systemic medication, ocular inflammation, head trauma, thyroid disease or the juvenile form of diabetes mellitus. The condition is often associated with convergence insufficiency, general fatigue, measles, multiple sclerosis, or myotonic dystrophy, etc. It is the most common accommodative dysfunction. Patients complain of blurred vision, or difficulty in sustaining clear vision at near; this is often accompanied by a frontal headache and even sometimes by pain in the eye. A mild form of accommodative insufficiency is often referred to as ill-sustained accommodation (accommodative fatigue) in which the response may be initially normal but cannot be maintained. It is easily discovered with accommodative facility exercises. Ill-sustained accommodation may be a precursor of accommodative insufficiency. Treatment is aimed at the primary cause, but plus lens correction, and in some cases exercises such as accommodative facility training are prescribed. Syn. premature presbyopia.
See convergence insufficiency; headache, ocular; ophthalmopathy, thyroid.
accommodative reflex See accommodation, reflex.
accommodative response The response of the accommodative system when the eye changes fixation from one point in space to another. The reaction time for the accommodative response is about 370 ms. Clinically it can be estimated by measuring the accommodative lag or accommodative lead.
See accommodation, mechanism of; effect, Mandelbaum.
accommodative rock See accommodative facility.
accommodometer Instrument used to measure accommodation such as the near point rule.
acetazolamide See carbonic anhydrase inhibitors.
acetone Liquid ketone (dimethyl ketone and propanone) used as a solvent for many organic compounds (e.g. cellulose acetate) and for repairing spectacle frames.
acetylcholine (ACh) A neurotransmitter substance with special excitatory properties of all preganglionic autonomic neurons, all parasympathetic postganglionic neurons and a few postganglionic sympathetic neurons. Acetylcholine is synthesized and liberated by the action of the enzyme choline acetyl-tranferase from the compounds choline and acetyl coenzyme A (acetyl CoA) which occurs in all cholinergic neurons. ACh exists only momentarily after its formation, being hydrolysed by the enzyme acetylcholinesterase which is present in the neurons of cholinergic nerves throughout their entire lengths and at neuromuscular junctions: this process is essential for proper muscle function as otherwise the accumulation of ACh would result in continuous stimulation of the muscles, glands and central nervous system. Alternatively a shortage of ACh has devastating effect (e.g. myasthenia gravis). ACh binds to acetylcholine receptors on skeletal muscle fibres. Sodium enters the muscle fibre membrane, which leads to a depolarization of the membrane and muscle contraction. There are two main types of acetylcholine receptors (cholinergic receptors): muscarinic receptors, which are stimulated by muscarine and ACh, belong to a family of G proteins coupled receptors and are situated in parasympathetically innervated structures (e.g. the iris and ciliary body); and nicotine receptors, which are stimulated by nicotine and ACh, are ligand-gated receptors and are situated in striated muscles (e.g. the extraocular muscles). Cholinergic receptors are found in the sympathetic and parasympathetic nervous systems, in the brain and spinal cord. The action of ACh can be either blocked or stimulated by drugs: Anticholinesterase drugs (e.g. neostigmine) inhibit acetylcholinesterase and prolong the action of acetylcholine whereas antimuscarinic drugs (also referred to as anticholinergics or parasympatholytics) such as atropine, cyclopentolate, homatropine, hyoscine and tropicamide inhibit the action of acetylcholine at muscarinic receptors. Other drugs mimic the action of ACh, they are known as parasympathomimetics (e.g. pilocarpine).
See cholinergic; cycloplegia; miotics; mydriatic; neurotransmitter; nicotine; synapse; system, autonomic nervous.
acetylcholinesterase An enzyme that degrades and inactivates acetylcholine. This compound is mainly found in neurons and at neuromuscular junctions. Drugs that inhibit this enzyme (e.g. diisopropyl fluorophosphate, physostigmine, edrophonium, echothiophate, DFP) can be used in the diagnosis and possible treatment of myasthenia gravis as well as certain forms of esotropia and glaucoma. Syn. specific cholinesterase.
acetylcysteine See tears, artificial.
achromasia See achromatopsia.
achromat See lens, achromatic.
achromatic 1. See lens, achromatic. 2. The condition of being totally colour blind.
See achromatopsia; light, white; spectrum, equal energy.
achromatic axis; colour; interval; lens See under the nouns.
achromatic light stimulus, specified Any specified illuminant capable of being accepted as white under usual conditions of observation. Note: This includes the CIE standard illuminants (CIE).
achromatic prism See prism, achromatic.
achromatism 1 . The condition of being totally colour blind. Syn. achromatopsia. 2. Absence of colour. 3. Condition of a lens or an optical system corrected for, or free from, chromatic aberration.
See monochromat.
achromatizing lens See lens, achromatizing.
achromatopsia Total colour blindness. The majority of cases are autosomal recessively inherited and caused by a mutation in genes CNGA3, CNGB3 and CNAT2. There are two types of achromatopsia. Complete achromatopsia which results from having only rods and no functional cones (rod monochromat) have photophobia, poor acuity and nystagmus. Incomplete achromatopsia in which there are the same symptoms, but in a diminished form. Patients benefit from dark tinted lenses. Achromatopsia is non-progressive and very rare: one person in about 35 000 people. A few cases may be acquired resulting from a lesion in cortical area V4 (central achromatopsia). Syn. achromasia; achromatic vision; achromatism; acritochromacy; monochromatism.
See colour vision, defective; hemiachromatopsia; monochromat.
achromic Colourless.
aciclovir See antiviral agents.
acidosis An abnormal condition characterized by an increase in acidity and a relative decrease in alkaline content of the blood and body tissues. Corneal acidosis occurs as a result of contact lens wear, especially low gas permeable lenses, due to an accumulation of lactic acid and an increase in the concentration of carbon dioxide (hypercapnia), which is associated with a lower pH. This leads to polymegethism and polymorphism of endothelial cells.
acne rosacea A chronic inflammatory disease of the sebaceous glands of the skin of the face. It usually appears in middle-aged individuals. Nearly a third of these patients have blepharoconjunctivitis with staphylococcal infection and a few per cent will develop rosacea keratitis. The patient presents with papules, pustules, erythema, telangiectasia and in some cases, rhinophyma, as well as facial erythema. Treatment includes lid hygiene with hot compresses, removal of crusts from the lid margins, and topical and systemic antibiotics.
See blepharitis, marginal; keratitis, rosacea.
acorea Absence of the pupil of the eye.
acquired Pertaining to a condition which is contracted after birth and is not hereditary.
See congenital; familial; hereditary.
Acquired Immune Deficiency Syndrome (AIDS) See syndrome, acquired immune deficiency.
acritochromacy See achromatopsia.
acrocephalosyndactyly See syndrome, Apert’s.
actinic Pertaining to the chemical activity of radiant energy (especially ultraviolet) on absorption by certain substances. In the eye, the cornea, in particular, but also the lens and retina are most susceptible.
See blindness, eclipse; retinopathy, solar.
actinic keratoconjunctivitis; keratopathy See under the nouns.
action, primary Term referring to the greatest effect of an extraocular muscle in one plane. The other actions are called the subsidiary or secondary and tertiary actions. The primary action of the inferior rectus is depression; of the superior rectus, elevation; of the inferior oblique, extorsion; and of the superior oblique, intorsion. The medial and lateral recti muscles exert their primary action in the primary position, that is, pure adduction for the medial rectus and pure abduction for the lateral rectus.
See test, forced duction; test, red glass.
action spectrum See spectrum, action.
action, tertiary Term referring to the least effect of an extrocular muscle. The tertiary action of the inferior rectus is extorsion; of the superior rectus, intorsion; of the inferior and superior oblique, abduction. The medial and lateral recti muscles are regarded as having only a primary action, at least in the primary position.
active position; transport See under the nouns.
acuity Term derived from the Latin (acutus) meaning acute or sharp: sharpness of vision.
angular visual a. See acuity, monotype visual.
central visual a. Visual acuity of the fovea and the macular area.
decimal visual a. Visual acuity expressed as a decimal. The Snellen fraction is reduced, e.g. 6/18 (or 20/60 in feet) = 0.33. If the acuity is given in visual angle, decimal acuity is the reciprocal, e.g. 1/(3 minutes of arc) = 0.33.
dynamic visual a. Capacity to see distinctly moving objects. Syn. kinetic visual acuity.
kinetic visual a. See acuity, dynamic visual.
letter visual a. 1. Visual acuity determined with letters on a chart. 2. Visual acuity determined with single isolated letters.
line visual a. See acuity, morphoscopic visual.
minimum separable visual a. See acuity, visual.
monotype visual a. Visual acuity determined with single isolated optotypes and therefore uninfluenced by neighbouring contours. Syn. acuity, angular visual.
morphoscopic visual a. Visual acuity determined with a group of optotypes such as, for example, a line of letters or Landolt rings. The result may thus be influenced by neighbouring contours. Syn. line visual acuity.
See phenomenon, crowding.
near visual a. Capacity for seeing distinctly the details of an object at near. It is specified in various ways: (1) As the angle of resolution of the smallest resolvable print (in minutes of arc) at a given near distance. (2) As a Snellen fraction, either as one that is equivalent to the distance visual acuity (Snellen equivalent) or more correctly as one which indicates the actual distance (e.g. 16/32 if the distance is 16 inches). (3) As an arbitrary Jaeger notation (e.g. J6). (4) As N notation (using Times Roman typeface) or Points (using any typeface), such as N8 at 40 cm (or simply 8-point), where N refers to near and the number to the amount of points (a point is a unit used by printers to specify print size and is equal to 0.35 mm or 1/72 of an inch). Thus N8 indicates that the overall height is 8/72 inch (or 2.82 mm) or about 4/72 inch (or 1.41 mm) for lower-case letters. (5) As M Units. For the usual font styles (e.g. Times Roman, Century) used in newsprint, 8-point print is usually considered to be approximately equal to 1 M Unit, so 1 M = N8, 2 M = N16, etc.
See chart, Bailey–Lovie; Jaeger test types.
objective visual a. Visual acuity measured without the subject’s judgement.
See potential, visual evoked cortical; method, preferential looking; test, optokinetic nystagmus.
peripheral visual a. Visual acuity of the peripheral regions of the retina, outside the macula.
resolution visual a. See acuity, visual.
Snellen a. Visual acuity as measured with Snellen letters.
static visual a. Acuity determined with stationary test types or test objects.
See acuity, dynamic visual; test type.
stereoscopic visual a. The ability to detect the smallest difference in depth between two objects. It is expressed as the difference η between the two angles subtended at any two objects in the field of view by the base line (or interpupillary distance). This threshold angle η (eta) is given by the approximate relationship, in radians
where PD is the interpupillary distance, d the test distance of the reference object and ΔD the distance between the two objects. (To convert the result into seconds of arc it should be multiplied by 180/π × 60 × 60 = 206265.) The difference between the two angles u1 – u2 (the difference between the two retinal images) is called binocular disparity or retinal disparity and the difference between the two angles β – α is called the relative binocular parallax (Fig. A5). Stereoscopic visual acuity is extremely fine, varying between 5 and 15 seconds of arc. It tends to decrease with age and it is positively correlated with Snellen visual acuity. Example: suppose ΔD is equal to 2 mm, d is 827 mm and the PD is 64 mm
Syn. stereo-acuity; stereo-threshold.
See angle of stereopsis; disparity, retinal; test, Howard–Dolman; test, three needle; vectogram.
Teller a. cards Test cards used to assess the visual acuity of infants. The set consists of 16 rectangular grey cards, each approximately 26 by 56 cm. Fifteen of the cards contain a high contrast square-wave grating, 12 by 12 cm, each of a given spatial frequency, and located either on the left or the right of a central peephole in the card. The average luminance of the grating is approximately equal to that of the grey background. The spatial frequencies of the gratings range from 0.3 to 38 cpd when viewed from 55 cm. The procedure consists in starting with the card with the lowest spatial frequency (or coarser grating) and proceeding to cards with finer gratings. The observer watches the infant through the central peephole and his or her task is to make a subjective judgment, based on the infant’s head and eye movements, of which is the finest grating card that the child can just resolve. The spatial frequency of this last card represents the estimate of the visual acuity. The procedure using these cards is based on the method of preferential looking but it is simpler, quicker and equally reliable.
See cycle per degree; method, preferential looking.
unaided visual a. Visual acuity without any correction. Syn. vision; unaided vision.
vernier visual a. The ability to detect the alignment or otherwise of two lines as in the reading of a vernier scale. This is the finest acuity being of the order of 1–5 seconds of arc depending on the length of the line; the longer the line, the more acute the detection. Syn. aligning power.
See hyperacuity.
visual a. (VA) Capacity for seeing distinctly the details of an object. Quantitatively, it is represented in two ways: (1) As the reciprocal of the minimum angle of resolution (in minutes of arc). This is the resolution visual acuity. Syn. minimum separable visual acuity. (2) As the Snellen fraction. This is measured using letters or Landolt rings or equivalent objects.
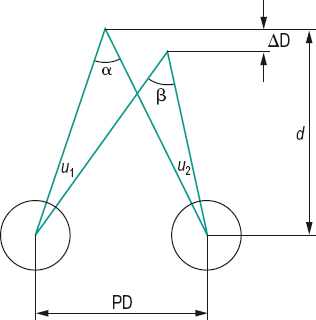
Table A5
Average relative visual acuity in the central region of the retina
| eccentricity | acuity | Snellen fraction | |
| (degrees) | (%) | (m) | (ft) |
| 0 | 100 | 6/6 | 20/20 |
| 0.5 | 80 | 6/7.5 | 20/25 |
| 1 | 66 | 6/9 | 20/30 |
| 1.5 | 57 | 6/11 | 20/37 |
| 2 | 49 | 6/12 | 20/40 |
| 2.5 | 41 | 6/14.5 | 20/48 |
| 3 | 39 | 6/15 | 20/50 |
| 3.5 | 37 | 6/16 | 20/53 |
| 4 | 35 | 6/17 | 20/57 |
| 4.5 | 33 | 6/18 | 20/60 |
| 5 | 32 | 6/19 | 20/63 |
| 6 | 29 | 6/21 | 20/70 |
| 7 | 27 | 6/22 | 20/73 |
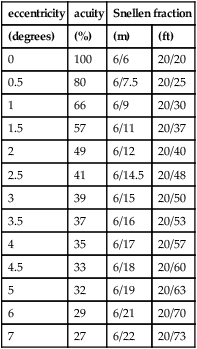
Table A6
Relationship between several near visual acuity notations
| Snellen equivalent in metres (feet) | |||
| 25 cm | 40 cm | points | M units |
| 6/240 (20/800) | 6/144 (20/480) | 80 | 10.0 |
| 6/192 (20/640) | 6/120 (20/400) | 64 | 8.0 |
| 6/144 (20/480) | 6/96 (20/320) | 48 | 6.4 |
| 6/120 (20/400) | 6/72 (20/240) | 40 | 4.8 |
| 6/96 (20/320) | 6/60 (20/200) | 32 | 4.0 |
| 6/72 (20/240) | 6/48 (20/160) | 24 | 3.2 |
| 6/60 (20/200) | 6/36 (20/120) | 20 | 2.4 |
| 6/48 (20/160) | 6/30 (20/100) | 16 | 2.0 |
| 6/36 (20/120) | 6/24 (20/80) | 12 | 1.6 |
| 6/30 (20/100) | 6/18 (20/60) | 10 | 1.2 |
| 6/24 (20/80) | 6/15 (20/50) | 8 | 1.0 |
| 6/18 (20/60) | 6/12 (20/40) | 6 | 0.8 |
| 6/15 (20/50) | 6/9 (20/30) | 5 | 0.6 |
| 6/12 (20/40) | 6/7.5 (20/25) | 4 | 0.5 |
| 6/9 (20/30) | 6/6 (20/20) | 3 | 0.4 |
| 6/6 (20/20) | 6/3.6 (20/12) | 2 | 0.25 |
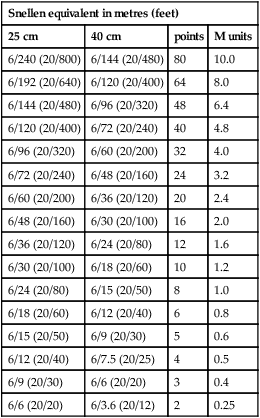
Table A7
Relationship between several distance visual acuity notations
| Snellen fraction | min. angle of resolution | decimal | |
| (m) | (ft) | (min. of arc) | |
| 6/180 | 20/600 | 30.0 | 0.03 |
| 6/150 | 20/500 | 25.0 | 0.04 |
| 6/120 | 20/400 | 20.0 | 0.05 |
| 6/90 | 20/300 | 15.0 | 0.07 |
| 6/60 | 20/200 | 10.0 | 0.10 |
| 6/30 | 20/100 | 5.0 | 0.20 |
| 6/24 | 20/80 | 4.0 | 0.25 |
| 6/21 | 20/70 | 3.5 | 0.29 |
| 6/18 | 20/60 | 3.0 | 0.33 |
| 6/15 | 20/50 | 2.5 | 0.40 |
| 6/12 | 20/40 | 2.0 | 0.50 |
| 6/9 | 20/30 | 1.5 | 0.67 |
| 6/7.5 | 20/25 | 1.3 | 0.80 |
| 6/6 | 20/20 | 1.0 | 1.0 |
| 6/4.5 | 20/15 | 0.75 | 1.33 |
| 6/3 | 20/10 | 0.5 | 2.0 |
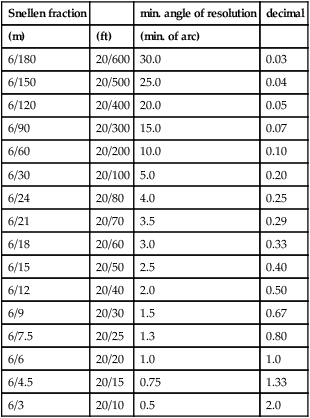
Average clinical visual acuity varies between 6/4 and 6/6 (or 20/15 and 20/20 in feet). Visual acuity varies with the region of the retina (being maximum in the foveola), with general illumination, contrast, colour and type of test, time of exposure, the refractive error of the eye, etc.
See angle of resolution, minimum; cycle per degree; Glasgow acuity cards; hyperacuity; isoacuity; optotype; sensitivity, contrast; Snellen fraction; test, Cardiff acuity; test, photostress; test, Sheridan–Gardiner; visual efficiency scale, Snell–Sterling.
acyanopsia Inability to recognize blue tints. See chromatopsia.
Adams desaturated D-15 test See test, Farnsworth.
adaptation 1 . Process by which a sensory organ (e.g. the eye) adjusts to its environment (e.g. to luminance, colour or contact lens wear). 2. The reduction in sensitivity to continuous sensory stimulation. The neurophysiological correlate corresponds to a decrease in the frequency of action potentials fired by a neuron, despite a stimulus of constant magnitude. Visual adaptation is prevented from occurring by the continuous involuntary movements of the eyes.
See movements, fixation; potential, action; stabilized retinal image.
chromatic a. Apparent changes in hue and saturation after prolonged exposure to a field of a specific colour.
dark a. Adjustment of the eye (particularly regeneration of visual pigments and dilatation of the pupil), such that, after observation in the dark, the sensitivity to light is greatly increased, i.e. the threshold response to light is decreased. This is a much slower process than light adaptation. Older people usually take longer to adapt to darkness and only reach a higher threshold than young people.
See adaptometer; hemeralopia; pigment, visual; theory, duplicity.
light a. Adjustment of the eye (particularly bleaching of visual pigments and constriction of the pupil), such that, after observation of a bright field, the sensitivity to light is diminished, i.e. the threshold of luminance is increased.
prism a. See adaptation, vergence.
sensory a. Mechanism by which the visual system adjusts to avoid confusion and diplopia of the perceptual impression due to an abnormal motor condition (e.g. strabismus).
vergence a. A process by which the eyes return to their condition of habitual heterophoria or orthophoria after a heterophoria has been induced by prisms (prism adaptation) in front of one or both eyes (as, for example, when lens centration does not coincide with the interpupillary distance), or by spherical lenses, or due to changes in the orbital contents with increasing age. This adaptation process may be related to the phenomenon of orthophorization. People who have symptomatic binocular vision anomalies do not, or only partially, show vergence adaptation to prisms. Vergence adaptation decreases with increasing age.
adaptometer An instrument for measuring the variations in threshold of luminance. The most common is that of Goldmann–Weekers.
addition, near (add) The difference in spherical power between the distance and near corrections. A common method of arriving at the power of the addition is to measure the patient’s working distance and the amplitude of accommodation. The add is obtained as follows

where x is the percentage of the total amplitude of accommodation which is to be used: two-thirds is usually more appropriate for young presbyopes (below about 52 years of age), while one-half is more appropriate for older presbyopes. Thus, this formula allows for a certain amount of the amplitude of accommodation to be left in reserve
(usually one-third or one-half). It can also be estimated based on age: +1.0 D to +1.25 D for age 45–50 years; +1.5 to +1.75 D for age 50–55 years; +2.0 D to +2.25 D for age 55–60 years; +2.5 D to +3.0 D for older patients. However these figures may need to be adjusted to take into account the average working distance of the patient. Syn. reading addition.
See bracketing; distance, reading; presbyopia; test at near, cross-cylinder.
adduct To turn towards the midline.
adduction Rotation of an eye towards the midline (Fig. A6).
See duction; paralysis of the third nerve; syndrome, Duane’s.
adductors Extraocular muscles that move the eye inward, such as the medial rectus, the inferior rectus and the superior rectus.
See muscles, extraocular.
adenoma, Fuchs’ A benign proliferation of small whitish nodules on the pars plicata of the ciliary body which may appear in elderly patients.
adenopathy See lymphadenopathy.
adenovirus A DNA virus, composed of over 40 serotypes. Many serotypes cause ocular infection, including epidemic keratoconjunctivitis caused by serotypes 8, 19 and 37. Other infections include follicular conjunctivitis with or without pseudomembranes and epithelial keratitis. The adenovirus can be identified using, among others, conjunctival swabs for viral antigen.
See conjunctivitis, acute.
adequate stimulus See stimulus, adequate.
adhesion See synechia.
Adie’s pupil; syndrome See under the nouns.
adipose tissue A type of fatty tissue that is present in large amounts in the orbit. The fat surrounds the orbit and acts as a cushion for the globe. The fat is divided by fibrous septae and is kept posteriorly by Tenon’s capsule.
adnexa oculi See appendages of the eye.
adrenaline (epinephrine) A hormone of the adrenal medulla which, instilled in the eye, causes a constriction of the conjunctival vessels, dilates the pupil and diminishes the intraocular pressure.
See adrenergic receptors; decongestant, ocular; naphazoline; neurotransmitter; noradrenaline (norepinephrine).
adrenergic 1 . Relating to a neuron that is activated or capable of releasing adrenaline (epinephrine). 2. Having an effect similar to adrenaline (epinephrine). 3. Relating to drugs that mimic the effects of the sympathetic nervous system (sympathomimetic drugs).
adrenergic agonist See sympathomimetic drugs.
adrenergic blocking agents See sympatholytic drugs.
adrenergic receptors Receptors which are stimulated by the catecholamines adrenaline (epinephrine) and noradrenaline (norepinephrine). These receptors belong to a family of G protein coupled receptors and are found in the central nervous system and many tissues innervated by the peripheral nervous system. There are two types of adrenergic receptors: (1) α-receptors, which are mainly excitatory to smooth muscles and gland cells but cause relaxation of intestinal smooth muscles; (2) β-receptors of which there are (at least) two types, β1 and β2. Generally, stimulation of β-receptors produces an inhibitory response, although in some cases the effect is excitatory (e.g. in the heart). Example: the dilator pupillae muscle contains mainly α-adrenergic receptors and stimulation (e.g. with adrenaline) produces mydriasis. On the other hand, there are drugs that block the effect of catecholamines on α- or β-adrenergic receptors and are called α- or β-blockers (or sympatholytic drugs or adrenergic receptor agonists). Example: the ciliary epithelium contains mainly β-receptors and a β-blocker such as timolol inhibits the secretion of aqueous humour, thus reducing intraocular pressure. Syn. adrenoceptor.
See alpha-adrenergic agonists; alpha-adrenergic antagonists; beta-blocker; miotics; mydriatic; sympatholytic drugs; sympathomimetic drugs; system, autonomic nervous.
adrenocorticosteroids Compounds created by the adrenal cortex that have distant metabolic effects. There are three types of compounds created by the adrenal cortex: glucocorticoids, mineralocorticoids, and androgens. Of these, the glucocorticoids are most important to the visual system due to their antiinflammatory effects. The antiinflammatory effect is thought to be mediated by inhibition of prostaglandin synthesis.
See antiinflammatory drug; steroid.
adult inclusion conjunctivitis See conjunctivitis, adult inclusion.
advancement procedure See recession.
aerial image See image, aerial.
aerial perspective See perspective, aerial.
aerobic Needing oxygen to sustain life.
See anaerobic.
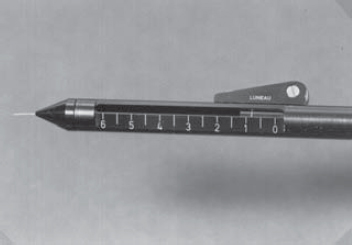
aesthesiometer Instrument for the measurement of sensitivity, especially tactile. The cornea and eyelid margins are the ocular structures measured. There are many types of aesthesiometers. The most common is that of Cochet–Bonnet (Fig. A7). It consists of a nylon monofilament of constant diameter which, depending upon its length, can exert more or less pressure. The length at which the subject responds to represents the corneal touch threshold. Others are non-contact and use a pulse of pressurised air or gas to stimulate the cornea. Note: also spelt esthesiometer.
See corneal fragility; hyperaesthesia, corneal; sensitivity, corneal; threshold, corneal touch.
aetiology The cause or origin of a disease. Note: also spelt etiology.
See diagnosis; epidemiology.
afferent Carrying from the periphery to the central or the main structure.
See efferent.
afferent limb, of pupillary pathway Section of the visual pathway originating in the rods and cones of the retina and terminating in the brainstem. The fibres follow the visual pathway, decussating in the optic chiasma, and continuing in the optic tracts. The fibres exit the optic tracts before reaching the lateral geniculate body, and project to the brainstem. After synapsing in the brainstem, the fibres then project to the ipsilateral and contralateral Edinger–Westphal nuclei.
See reflex, pupil light.
afferent pupillary defect See pupil, Marcus Gunn.
afocal Refers to a lens or an optical system with zero focal power, i.e. in which incident rays entering parallel emerge parallel.
See lens, afocal; lens, aniseikonic.
after-cataract An opacity in the posterior capsule of the crystalline lens which may have remained or occurred after extracapsular cataract extraction (manual or phacoemulsification). Treatment is typically with a neodymium-yag laser to create a central hole in the capsule (capsulotomy). Syn. secondary cataract.
See cataract extraction, extracapsular.
after-effect, motion See after-effect, waterfall.
after-effect, tilt Observation of a temporary change in the perceived orientation of lines after having adapted to lines tilted in another direction. If, for example, you stare at white and black bars tilted to the left for a minute or so, then look at vertical bars, these will now appear to tilt slightly to the right. This is an example of the adaptation of orientation-specific cells in the visual system which become fatigued and therefore temporarily less responsive.
See adaptation; after-effect, waterfall; cell, orientation-specific.
after-effect, waterfall Observation of a movement in the opposite direction when fixating a stationary object, after having looked at a waterfall for some time. This is an example of phenomena that are used to infer the existence of channels in the visual system. It is suggested that there are two opposed directionally sensitive neural channels (or neurons) which are normally in balance for stationary stimuli, but when the activity of one channel is fatigued by prolonged stimulation, the other one becomes the active one. The waterfall after-effect is a special case of motion or movement after-effect (or motion after-image). Syn. waterfall effect; waterfall illusion.
See channel; spiral, Plateau’s.
after-image Visual sensation persisting after the original stimulus has been removed. If observed in darkness following stimulation by a high intensity, brief duration light source, seven different after-image phases are frequently noted. The first phase, also called Hering’s after-image, is a positive after-image and it is followed by a negative after-image. After a short interval (less than half a second) a second positive after-image, called Purkinje after-image or Bidwell’s ghost, appears, the character of which depends upon the conditions of adaptation, the colour of the stimulus and the retinal region stimulated (best in the periphery). Afterwards, a second negative after-image is sometimes observed followed by a third positive after-image, called Hess after-image. After a long dark interval, a third negative after-image may appear followed after another long dark interval by a fourth positive after-image. If the light stimulus is of moderate intensity, the last phases will be absent.
See law, Emmert’s; test, after-image; test, after-image transfer.
complementary a. An after-image in which the colour is complementary to the colour of the original stimulus.
Hering’s; Hess a. See after-image.
homochromatic a. An after-image in which the colour appears the same as in the original stimulus.
motion a. See after-effect, waterfall; spiral, Plateau’s.
negative a. An after-image in which the light areas of the original stimulus appear dark, the dark areas appear light and the coloured areas appear in a complementary colour.
positive a. An after-image that appears the same as the original stimulus.
Purkinje a. See after-image.
against movement See movement, against.
agnosia Inability to recognize the import of sensory stimuli (e.g. to recognize colour, faces, shape and the orientation of objects), although the receptors and the sensory pathway are intact. The condition is attributed to bilateral lesions in the association areas of the cortex. If the sense of sight is affected, it is called visual agnosia (perceptual or psychic blindness).
See alexia; apraxia, optical; prosopagnosia.
agonist 1. An agonistic muscle. 2. A substance (e.g. a drug, hormone or neurotransmitter) that binds with a cell receptor to initiate a physiological response similar to that produced by the natural neurotransmitter or hormone. Example: pilocarpine, which mimics the effect of acetylcholine acting on cholinergic receptors.
See antagonist.
agonist drug A drug that combines with the receptor to mimic or enhance the effect of a neurotransmitter.
agonistic muscle See muscle, agonistic.
agraphia Inability to write, usually as a result of a brain lesion. If the person can write from dictation but not from copying, it is called visual agraphia.
Aicardi’s syndrome See syndrome, Aicardi’s.
AIDS See syndrome, acquired immunodeficiency.
aids, low vision Optical (e.g. loupe) or nonoptical (e.g. large numeral telephone) appliances and devices designed to assist the partially sighted patient.
See glass, magnifying; lamp, halogen; lens, telescopic; spectacles, pinhole; typoscope; vision, low.
air-puff tonometer See tonometer, non-contact.
akinaesthesia 1. Inability to perceive moving objects. Example: as a glass is filling up with water the person cannot see the level moving, but only a succession of fixed images. 2. Lack or loss of muscular sense.
alacrima Absence of secretion from the lacrimal gland. However, the typical picture is one of reduced tear secretion more correctly termed hypolacrima. It may occur as a result of occlusion of the orifices of the lacrimal gland due to trauma, cicatrization, diseases (e.g. trachoma); it may be congenital (e.g. Riley–Day syndrome) or it may be due to a neurogenic cause (secondary to brain damage) or to a systemic disease (e.g. Sjögren’s syndrome). Treatment includes artificial tears, bland ointments, sealed scleral contact lenses and, in very severe cases, tarsorrhaphy.
See keratoconjunctivitis sicca.
Alagille syndrome See syndrome, Alagille.
albedo retinae Oedema of the retina.
albinism Congenital anomaly due to a defect of melanin production as a result of one of several possible genetic defects. Oculocutaneous albinism type 1(OCA1) is due to a genetic defect in tyrosinase, the enzyme that metabolizes the amino acid tyrosine, which is essential for its conversion to melanin (formerly called tyrosinase-negative albinism). It is an autosomal recessive condition, which affects the skin, hair and eyes. The iris is a pale colour, the fundus and the pupil are reddish and the eye transilluminates markedly. There is poor visual acuity, photophobia, nystagmus and strabismus. Oculocutaneous type 2 (OCA2) is caused by a mutation of the OCA2 (‘P’) gene resulting in variable amounts of melanin synthesis. The hypopigmentation of the eyes, skin and hair varies from fair to normal (formerly called tyrosinase-positive albinism). It may be associated with the Hermansky–Pudlak syndrome in which there is albinism and easy bruising or bleeding. The other type of albinism is ocular albinism type 1 (OA1). It is inherited either as an X-linked or less commonly as an autosomal recessive trait. It affects mainly the eyes and in most instances males only and the skin colour is usually normal. Management involves full correction, possibly with tinted lenses. Surgery may be required for strabismus.
See fundus, ocular; inheritance; transillumination.
Albright’s syndrome See syndrome, Albright’s.
alcohol See antiseptic.
Alexander’s law See law, Alexander’s.
alexia Inability to recognize written or printed words due to a lesion in the brain. This is a form of visual agnosia. Syn. word blindness.
Algorithm, Swedish Interactive Thresholding (SITA) A program designed to shorten the time taken to determine the threshold values of each location of the visual field being tested with an automated perimeter. Stimulus presentation is altered according to the patient’s response time, the quicker the patient responds the faster the rate of presentation and vice versa. Patient’s reliability is also taken into account.
aligning power See acuity, vernier visual.
aligning prism See heterophoria, associated.
alignment fit See fitted on K.
alkaptonuria A rare, hereditary, metabolic disorder characterized by dark urine. It is caused by mutation in the homogentisate 1, 2-dioxygenase gene (HGD), which produces an error in the metabolism of the amino acids tyrosine and phenylalanine, which normally break down by oxidation to homogentisic acid. However, in this condition homogentisic acid is not broken down but stored in tissues, especially cartilage, which it turns bluish-black, and excreted in the urine. Ocular signs are pigmentation of the sclera, most markedly near the insertions of the recti muscles, and of the cornea and conjunctiva.
all or none law See law, all or none.
allele See genotype.
Allen–Thorpe gonioprism See gonioprism.
allergic reactions See hypersensitivity.
allergy A state of hypersensitivity induced by re-exposure to a particular antigen (called allergen), usually environmental, such as pollens, foods, microorganisms and drugs.
See conjunctivitis, allergic; hypersensitivity.
allesthesia, visual A rare disorder in which a visual stimulus located in one half of the visual field is perceived as being located in the other. Occasionally the visual stimulus may be transposed from the lower to the upper quadrant, or vice versa. The condition may occur as a result of damage to the parietal or occipital cortex.
allometropia Refraction of the eye along any line except the visual axis (or line of sight) therefore representing the refraction of any extrafoveal region. Example: if an eye is emmetropic along the visual axis, at 40 degrees of temporal retinal eccentricity the allometropia will be about plano –2.50 × 90° and at 50 degrees, +0.50–3.50 × 90°.
See astigmatism, oblique.
allowance See retinoscope.
allyl diglycol carbonate See CR-39 material.
all-trans See rhodopsin.
alpha-adrenergic agonist An agent that selectively binds and activates alpha-adrenergic receptors. In the eye it causes mydriasis and reduces the production of aqueous humour. It is used topically in the treatment of glaucoma. Common agents include adrenaline (epinephrine), noradrenaline (norepinephrine), apraclonidine and brimonidine tartrate.
See adrenergic receptor; sympathomimetic drugs.
alpha-adrenergic antagonist An adrenergic blocking agent which produces miosis and a slight reduction in intraocular pressure. It is used mainly to reverse the mydriatic effect of sympathomimetic drugs (e.g. phenylephrine hydrochloride), or even some antimuscarinic drugs (e.g. tropicamide). Common agents include dapiprazole and moxisylyte (thymoxamine). Syn. alpha-blocker.
See sympatholytic drugs.
alpha-blocker See alpha-adrenergic antagonist.
alpha waves Rhythmic oscillation in electrical potential occurring in the cortex of the human brain when awake and at rest. The rate of oscillation is 8–13 Hz. Syn. alpha rhythm.
See potential, resting membrane.
alphabet patterns See pattern, A; pattern, V; pattern, X; pattern, Y.
alternate cover test See test, cover.
alternating checkerboard stimulus A type of light stimulus used in performing electrophysiological testing. Most often used in the pattern electroretinogram (pERG), it maintains constant luminance to the entire retina. The pERG measures ganglion cell function, in contrast to the ERG, which measures the function of the photoreceptor and bipolar cell layers of the retina.
alternating hypertropia; strabismus See under the nouns.
altitudinal hemianopia See hemianopia, altitudinal.
Alvarez lens See lens, Alvarez.
amacrine cell See cell, amacrine.
amaurosis 1. Partial or total loss of sight due to a lesion somewhere in the visual pathway (usually the optic nerve), but not in the eye itself. 2. Synonym for blindness.
amaurosis fugax Transient unilateral loss of vision. The visual loss varies from partial to total blindness and rarely lasts longer than 10 minutes. It is usually caused by a temporary occlusion in the internal carotid artery, which produces an insufficient blood flow to the ophthalmic artery and may lead to closure of the central retinal artery. Syn. blackout.
See angiography, fluorescein; arteritis, temporal; blackout; bruit; plaques, Hollenhorst’s; retinal arterial occlusion.
amaurosis, Leber’s congenital See Leber’s congenital amaurosis.
ambiocularity 1. See dominance, ocular. 2. In strabismus, the condition in which the patient uses either eye.
ambiguous figure See figure, Blivet; figure, Kanisza; Necker cube; Schroeder’s staircase; vase, Rubin’s.
amblyope Person who has amblyopia.
amblyopia A condition characterized by reduced visual acuity due to a lesion in the eye or in the visual pathway, which hinders the normal development of vision, and which is not correctable by spectacles or contact lenses. The usual clinical criterion is 6/9 (or 20/30) or less in one eye, or a two-line difference or more, on the acuity chart between the two eyes. Amblyopia may occur as a result of: suppression in the deviated eye in strabismus (strabismic amblyopia; formerly called amblyopia ex anopsia, which amounts to about 20% of all cases); a blurred image in the more ametropic eye in uncorrected anisometropia (anisometropic amblyopia which amounts to about 50% of all cases); bilateral blurred images in uncorrected refractive errors (isoametropic amblyopia); a blurred image in one of the meridians of high uncorrected astigmatism (meridional amblyopia); any of the above three is also called refractive amblyopia; opacities in the ocular media (e.g. congenital cataract, severe ptosis) in infants (stimulus deprivation amblyopia or visual deprivation amblyopia or image degradation amblyopia) after the lesion has been removed; continuous occlusion of an eye as may occur in occlusion treatment (occlusion amblyopia); arsenic, lead or quinine poisoning (toxic amblyopia) or the more specific types of toxic amblyopia such as those caused by excessive use of alcohol (alcohol amblyopia), methanol (methanol amblyopia), quinine (quinine amblyopia) or tobacco (tobacco amblyopia), although the latter three may actually be due to nutritional deficiencies (nutritional amblyopia); psychological origin (hysterical amblyopia) or of unknown origin (idiopathic amblyopia).
Many of these amblyopias are functional, i.e. in which no organic lesion exists as in hysterical, refractive (e.g. meridional amblyopia), isoametropic, strabismic or stimulus deprivation amblyopia. Others are organic, i.e. they are due to some pathological (e.g. congenital cataract) or anatomical anomalies (e.g. malorientation of retinal receptors), as in nutritional or toxic. However, there may be cases in which a functional amblyopia is due in part to some accompanying undetected pathology or structural defects (e.g. a change in retinal fibre layer thickness). Amblyopia occurs in 2–4% of the population. There is usually a reduction in the amplitude of accommodation in amblyopic eyes. Treatment of amblyopia depends on the type. However, the younger the patient, the more likely that the treatment will be successful. Typically, the principal treatment is occlusion of the fixating eye (or the eye with the best acuity) by patching or blurring with atropine sulfate to force the other eye to take up fixation, after full refractive correction and treatment of the underlying pathology. Other procedures (alternatives or supplemental to patching) include penalization, kicking a ball towards a specific target, playing catch a ball, bar reading, pleoptics (when there is eccentric fixation as well), and any other procedures which require fixation like drawing, duplicating letter sequences on a typewriter, cutting out patterns, etc. See cheiroscope; disc, pinhole; fixation, eccentric; Glasgow acuity cards; occlusion treatment; penalization; period, critical; phenomenon, crowding; pleoptics; suppression; test, bar reading; test, neutral density filter.
hysterical a. Apparent loss of vision due to a psychological disorder. The patient really believes that he or she cannot see, although this is not supported by physiological impairment. The condition is often characterized by a constricted visual field or tunnel vision.
meridional a. Amblyopia in one of the two principal meridians of an astigmatic eye. The amblyopia usually affects the most defocused meridian and its severity tends to vary with the amount of astigmatism. This amblyopia is of neural origin. Optical correction of the patient as young as possible usually prevents this condition. Syn. astigmatic amblyopia.
amblyopiagenic Pertains to factors causing amblyopia, such as anisometropia, strabismus, opacities in the ocular media, etc.
amblyopic eye nystagmus See under the nouns.
amblyoscope, major See amblyoscope, Worth.
amblyoscope, Wheatstone Amblyoscope using mirrors to change the angle of convergence or divergence. Syn. Wheatstone stereoscope.
amblyoscope, Worth A modified haploscope introduced by Worth, consisting of two angled tubes held in front of the eyes which present a different image to each eye, and which can be turned to any degree of convergence or divergence. Using various images (slides), the instrument can be used to measure the angle of deviation and vergence amplitudes, and to investigate retinal correspondence, fusion, suppression and stereopsis. If the instrument is incorporated into a table, it is called a major amblyoscope of which there are various types called Synoptiscope or Synoptophore.
amethocaine hydrochloride See tetracaine.
ametrope Person who has ametropia.
ametropia Anomaly of the refractive state of the eye in which, with relaxed accommodation, the image of objects at infinity is not formed on the retina. Thus vision may be blurred. The ametropias are: astigmatism, hyperopia (hypermetropia) and myopia. The absence of ametropia is called emmetropia. Syn. refractive error; error of refraction; refraction (although not strictly correct since this term may also refer to the lack of ametropia).
See defocus, hyperopic; defocus, myopic; refraction; refractive error; theory, biological-statistical; theory, emmetropization; theory, nativistic.
axial a. Ametropia due primarily to an abnormal length of the eye while the refractive power is approximately normal (Fig. A8).
refractive a. Ametropia due primarily to an abnormal refractive power of the eye while the length is approximately normal. Refractive ametropias can be attributed to either an abnormal radius of curvature of the surfaces of the cornea, or the crystalline lens (curvature ametropia) or to an abnormal index of refraction of one or more of the ocular media (index ametropia).
amikacin sulfate See antibiotic.
aminoglycoside Any one of a group of antibiotics composed of amino sugars in glycoside linkage which act by interfering with the synthesis of bacterial proteins. It is used in the treatment of infections caused by Gram-negative bacteria. Examples: framycetin, gentamicin, neomycin and tobramycin.
Ammann’s test See test, neutral density filter.
amphotericin B See antifungal agent.
amplitude of accommodation See accommodation, amplitude of.
amplitude of convergence See convergence, amplitude of.
Amsler chart; grid See chart, Amsler.
anaerobic Ability to sustain life in an atmosphere devoid of oxygen.
See aerobic.
anaesthesia 1. A loss of sensation in a part, or in the whole body, induced by the administration of a drug (an anaesthetic agent). 2. A loss of sensation, usually touch, in a part of the body as a result of some nervous lesion. Example: corneal anaesthesia. Note: also spelt anesthesia.
See injection, peribulbar.
topical a. Application of a local anaesthetic agent to an area of the skin or mucous membrane (e.g. conjunctiva) to produce anaesthesia. The application may be via direct instillation, soaked swabs, ointments or sprays. Syn. surface anaesthesia.
anaesthetic Any substance used to produce a loss of pain sensation either in the whole of the body when unconscious (general anaesthetic) or to some part of the body when awake (local anaesthetic). Note: also spelt anesthetic.
local a’s. Chemical agents that prevent the transmission of nerve impulses by binding to the sodium channel and thus blocking the transient rush of sodium ions through the cell membrane. They act locally and without loss of consciousness. They can be either ester-linked (e.g. benoxinate, cocaine, oxybuprocaine hydrochloride (benoxinate), proxymetacaine hydrochloride, and tetracaine hydrochloride) or amide-linked (e.g. bupivacaine, lidocaine hydrochloride and procaine). Ester types are applied mainly topically whereas amide types are usually administered by injection.
See injection, peribulbar; potential, receptor.
anaglyph Stereogram consisting of two superimposed and laterally displaced drawings or photographs of the same scene but taken from two directions and in complementary colours (usually red and green). If the anaglyphs are viewed through filters of the same colour, one to each eye, and induce retinal disparity (of a fixed amount) they give rise to the perception of depth or stereopsis. A set of cards, or targets on the same card, to induce various amounts of retinal disparity can be used to detect and train fusion and stereopsis (e.g. Tranaglyphs).
See colour, complementary; disparity, retinal; fusion, sensory; perception, depth; stereogram, random-dot; stereopsis.
analgesic A remedy or agent that relieves pain.
analyser 1. Polarizing device used to determine the plane of vibration of a beam of polarized light. Examples: Nicol prism, polaroid sheet, tourmaline crystal. 2. In a polariscope, the second of the two polarizing elements, the first being the polarizer.
See light, polarized.
analyser, Friedmann visual field Instrument designed to examine the central visual field. It utilizes a single xenon discharge tube placed within an integrating bowl, in front of which are fenestrated plates which can present 15 different patterns composed of either two, three or four stimuli of variable intensity and brief duration. Mark II has two programmes with 18 and 31 patterns each.
Analyser, Humphrey Vision Subjective refractometer utilizing continuously variable-power lenses developed by Alvarez. The image of a target is formed by this variable-power lens and is reflected by a concave mirror situated 3 m away from the patient. The vergence of light entering the eye can be changed by changing the power of the Alvarez lens: spherical, as well as astigmatic, errors of refraction and binocular vision tests can be made. The spherocylinder correction is automatically computed.
anaphoria See hypertropia, alternating.
anastigmatic lens See lens, anastigmatic.
anastomosis A natural communication between two blood vessels or other tubular structures. Example: the long posterior ciliary artery divides into two branches as it enters the posterior part of the ciliary muscle and at its anterior end these branches anastomose with each other and with the anterior ciliary arteries to form the major arterial circle of the iris.
See arterial circle of the iris, major.
anatomical position of rest See position of rest, anatomical.
anatropia See hypertropia, alternating.
Andersen–Warburg syndrome See disease, Norrie’s.
anesthesia See anaesthesia.
aneuploidy See chromosome.
aneurysm A localized dilatation of the walls of a blood vessel, usually an artery, as a result of infection, injury or degeneration. It is filled with fluid or clotted blood. Aneurysms occur in diabetic retinopathy, and retinal veinocclusion leading to haemorrhages and oedema.
angiogenesis See VEGF.
angiogram The photographic image obtained in fluorescein angiography.
angiography, fluorescein A technique aimed at observing the vessels of the fundus of the eye and iris by using photography following the intravenous injection of fluorescein. It is a useful technique, which facilitates the diagnosis of various retinal (e.g. diabetic retinopathy, retinal artery occlusion, retinal vein occlusion, age-related maculopathy), choroidal (e.g. tumour of the choroid) and iris disorders. Those of the choroid and iris are more difficult to observe.
See choroidal flush; retinopathy, diabetic.
angioid streaks Degeneration of Bruch’s membrane of the choroid characterized by brown or reddish lines or streaks in the fundus of the eye. The condition is bilateral, although one eye may be affected more than the other. Patients may occasionally be aware of some visual impairment in the visual field depending on the location of the streaks. The membrane is very fragile and liable to rupture in the case of ocular trauma, which may lead to macular haemorrhage and visual loss. Angioid streaks are often found in association with pseudoxanthoma elasticum (an eruption of small, superficial, solid elevation of the skin of the neck and other areas), Paget’s disease, Ehlers–Danlos syndrome or sickle-cell anaemia.
See neovascularization, choroidal.
angioma Tumour of the blood vessels.
angiomatosis retinae See disease, von Hippel’s.
angioscotoma A scotoma produced by the shadow cast by the retinal blood vessels. It looks like the branches of a tree extending from the blind spot. It is seen only in special conditions of illumination as when illuminating the fundus of the eye by gently moving a penlight over the closed eyelid, or when illuminating the fundus through the sclera, or when plotting the visual field. This phenomenon is sometimes used as a test to predict gross macular function in a patient with dense cataract where visualization of the fundus is impossible, although better results are obtained with the blue field entoptoscope. Syn. Purkinje figures; Purkinje shadows; Purkinje tree.
angle 1. The figure formed by two intersecting lines or planes at one point. 2. The direction from which an object is viewed. 3. The form produced by a change in direction of a line or plane.
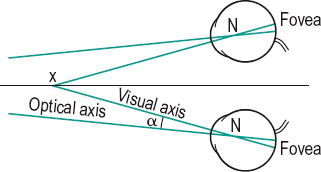
a. alpha Angle between the visual axis and the optical axis formed at the first nodal point of the eye. The visual axis usually lies nasal to the optical axis on the plane of the cornea (positive angle alpha). It is, on average, equal to about 5° in the adult eye. If it lies temporal to the optical axis, the angle is denoted negative (Fig. A9). Symbol: α.
See angle lambda.
a. of altitude 1. The angle through which the eyes have turned up or down from the primary position by a rotation about the transverse axis (x-axis). 2. The angle between the plane of regard and the subjective horizontal plane. Syn. angle of elevation.
a. of anomaly Angle between the line of visual direction of the fovea and the line of visual direction of the abnormal corresponding point of the same deviated eye. It is usually represented by the difference between the objective and subjective angles of deviation in abnormal retinal correspondence.
See line of direction; retinal correspondence, abnormal.
a. of the anterior chamber Angle at the periphery of the anterior chamber formed by the root of the iris, the front surface of the ciliary body and the trabecular meshwork. Syn. angle of filtration; drainage angle; iridocorneal angle.
See gonioscope; method, van Herick, Shaffer and Schwartz; method, Smith’s; test, shadow.
a. of azimuth The angle through which the eyes have turned right or left from the primary position by a rotation about the vertical axis.
Brewster’s a. See angle of polarization.
contact a. Angle formed by a surface and a tangent to a sessile drop of fluid (usually water) at the point where the drop meets the surface. This angle indicates the degree of wettability of that surface. The more wettable (or hydrophilic) the material, the smaller the angle, being equal to 0° for a completely hydrophilic material when water spreads evenly over that surface. Hydrophobic surfaces can have contact angles greater than 90°, e.g. silicone rubber in which the angle is about 120° (Fig. A10). Syn. wetting angle.
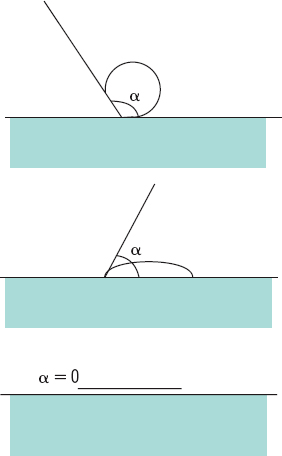
See test, sessile drop.
a. of convergence Angle between the lines of sight of the two eyes which are in a state of convergence. The angle is positive when the lines of sight intersect in front of the eyes, and negative when they intersect behind the eyes. Note: some authors regard the angle of convergence as the rotation of one eye only towards the fixation point, and refer to the angle of convergence of both eyes, defined above, as the total angle of convergence or the total convergence. The total angle of convergence required for binocular fixation of a target is equal to

or

where d is the distance between the target and the midpoint of the base line and PD the interpupillary distance. Syn. angle of triangulation.
See angle, metre; dioptre, prism; line of sight.
critical a. That angle of incidence which results in the refracted ray travelling along the surface between the two media (angle of refraction equal to 90°). If the angle of incidence is greater than the critical angle, the ray is totally reflected. If, however, the angle of incidence is smaller than the critical angle, the ray is refracted (with some light reflected). The critical angle ic is given by the following formula
where n and n’ are the indices of the media on each side of the surface, with the light travelling from the high index medium n to the low index medium n’ (Fig. A11). Syn. limiting angle.
See optics, fibre; prism, reflecting; reflection, total; refractometer.
a. of deviation 1. Angle through which a ray of light is deviated on reflection by a mirror, or refraction by a lens or prism. 2. Angle between the visual axis (or line of sight) of the deviated eye in strabismus and the straight-ahead position while the other eye fixates straight ahead. It can be assessed subjectively by having the patient report simultaneous perception (e.g. the lion in the cage seen in the amblyoscope) or objectively as measured by the practitioner either with the amblyoscope or using prisms and cover test, or by the Hirschberg test. Syn. angle of squint; angle of strabismus. See angle of anomaly; incomitance; method, Hirschberg’s; method, Javal’s; method, Krimsky’s; prism, minimum deviation of a.
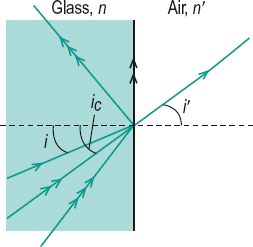
a. of divergence Angle between the lines of sight of the two eyes which are in a state of divergence.
drainage a. See angle of the anterior chamber.
a. of elevation See angle of altitude.
a. eta See acuity, stereoscopic visual.
external a. See canthus.
a. of filtration See angle of the anterior chamber.
a. gamma The angle between the optical axis and the fixation axis.
a. of incidence Angle between the incident ray and the normal to the surface at the point of incidence in either reflection or refraction at a surface separating two media.
irido-corneal a . See angle of the anterior chamber.
a. kappa Angle between the pupillary axis and the visual axis, measured at the nodal point. Symbol: κ.
See angle lambda; line of sight.
a. lambda Angle between the pupillary axis and the line of sight formed at the centre of the entrance pupil. It is this angle which is measured clinically as it is almost equal to angle alpha. Symbol: λ. See axis, pupillary; line of sight.
Table A8
Critical angle (in degrees) beyond which all the light is reflected at the surface separating various transparent substances from air or water
| substance | refractive index n | critical angle ic | |
| in contact with air n’ = 1 | in contact with water n’ = 1.333 | ||
| water | 1.333 | 48.6 | – |
| spectacle crown glass | 1.523 | 41.0 | 61.1 |
| flint glass (dense) | 1.62 | 38.1 | 55.4 |
| flint glass (extra dense) | 1.706 | 35.9 | 51.4 |
| PMMA | 1.49 | 42.2 | 63.5 |
| CR-39 | 1.498 | 41.9 | 62.9 |
| polycarbonate | 1.586 | 39.1 | 57.2 |
| diamond | 2.42 | 24.4 | 33.4 |
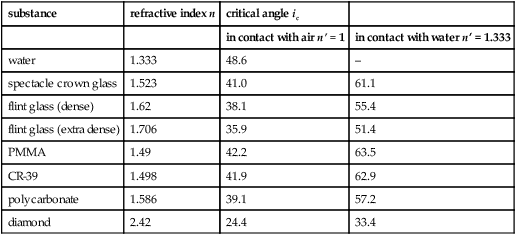
Table A9
Relationship between viewing distance and total convergence in metre angles and prism dioptres for 4 interpupillary distances (PD in cm)
| object distance from cornea (cm) | metre angle (ma) | convergence (in prism dioptres) | |||
| PD: 6.0 | 6.4 | 6.8 | 7.0 | ||
| 200 | 0.5 | 3.0 | 3.2 | 3.4 | 3.5 |
| 100 | 1.0 | 6.0 | 6.4 | 6.8 | 7.0 |
| 67 | 1.5 | 9.0 | 9.6 | 10.2 | 10.5 |
| 50 | 2.0 | 12.0 | 12.8 | 13.6 | 14.0 |
| 40 | 2.5 | 15.0 | 16.0 | 17.0 | 17.5 |
| 33 | 3.0 | 18.0 | 19.2 | 20.4 | 21.0 |
| 25 | 4.0 | 24.0 | 25.6 | 27.2 | 28.0 |
| 20 | 5.0 | 30.0 | 32.0 | 34.0 | 35.0 |
| 16 | 6.25 | 37.5 | 40.0 | 42.5 | 43.7 |
| 14 | 7.14 | 42.8 | 45.7 | 48.5 | 50.0 |
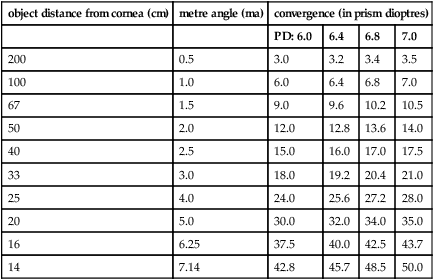
limiting a. See angle, critical.
metre a. (ma) Unit of convergence which is equal to the reciprocal of the distance (in metres) between the point of fixation assumed to lie on the median line and the base line of the eyes. Thus, if an object is located at 25 cm from the base line, each eye converges through 4 ma; at 1 metre, 1 ma, etc. Metre angles of convergence can be converted into prism dioptres of convergence by multiplying by the subject’s interpupillary distance expressed in cm. Example: for a PD of 6.0 cm, a convergence of 5 ma = 30 Δ.
See angle of convergence.
minimum a. of resolution (MAR) The angle subtended at the nodal point of the eye (or the centre of the entrance pupil) by two points or two lines which can just be distinguished as separate.
See acuity, visual; chart, log MAR.
palpebral a. See canthus.
pantoscopic a. Angle between the spectacle plane and the frontal plane of the face when the superior edge of the lens is farther away from the face than the inferior edge (Fig. A12). Syn. pantoscopic tilt.
See angle, retroscopic.
a. of polarization The angle of incidence at which the reflected light is maximally polarized. At this angle, the reflected and refracted rays are 90° apart (Fig. A13). This angle i is given by the equation
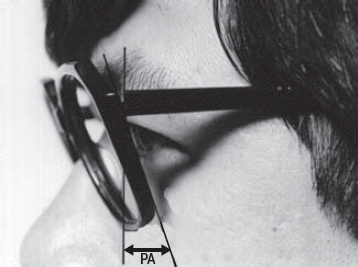
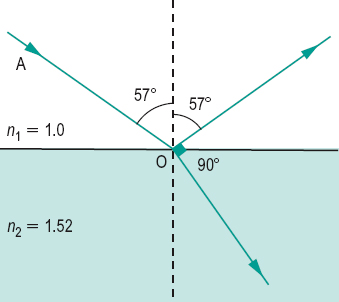
and measures 56.7° when the first medium n1 is air and the second medium n2 is a glass with an index of refraction equal to 1.523. Syn. Brewster’s angle.
See light, polarized.
prism a. The angle between the two refracting surfaces of a prism. Syn. apical angle; refracting angle (this term is deprecated because of the confusion with ‘angle of refraction’).
recession a. A tear between the longitudinal and circular muscles of the ciliary body. It is most often noted following blunt trauma to the anterior segment. It is typically followed by hyphaemia. This form of injury predisposes the individual to elevated intraocular pressure (i.e. increased risk of glaucoma) in the future. With a gonioscope, angle recession appears with an abnormally wide ciliary body band with a prominent scleral spur and some torn iris processes. There are also marked variations in the width and depth of the angle in different quadrants of the eye.
See cyclodialysis; hyphaemia; iridodialysis; muscle, ciliary.
a. of ref lection Angle between the reflected ray and the normal to the surface at the point of incidence.
a. of refraction Angle between the refracted ray and the normal to the surface at the point of emergence.
retroscopic a. Angle between the spectacle plane and the frontal plane of the face when the superior edge of the lens is closer to the face than the inferior edge. Syn. retroscopic tilt.
See angle, pantoscopic; plane, frontal; plane, spectacle.
a. of squint See angle of deviation.
a. of stereopsis The difference between the angles subtended at the centres of the entrance pupils of the two eyes by two points located in space at different distances from the eyes.
See acuity, stereoscopic visual; test, Howard–Dolman; test, three-needle.
a. of strabismus See angle of deviation.
total a. of convergence See angle of convergence.
a. of triangulation See angle of convergence.
visual a. The angle subtended by the extremities of an object at the anterior nodal point of the eye. If the object is far away, the point of reference can be the centre of the entrance pupil or even the anterior pole of the cornea. Syn. viewing angle.
wetting a. See angle, contact.
refracting a. See angle, prism.
angle-closure glaucoma See glaucoma, angle-closure.
angling Adjusting the angle which the sides of a spectacle frame make with the plane of its front. See angle, pantoscopic; angle, retroscopic.
ångström unit Unit of wavelength of radiant energy. One unit is equal to one ten thousand millionth of a metre (10–10 m). Symbol: A or Å. It is preferable to use the nanometre, which is an SI unit.
aniridia Complete, or almost complete, absence of the iris of the eye. It can be acquired, due to trauma, or inherited as an autosomal dominant trait. The patient is photophobic and in congenital cases there is usually amblyopia and sometimes nystagmus. Contact lenses incorporating an artificial iris, or tinted spectacle lenses, help in this condition.
See chromosome; irideremia; lens, cosmetic contact.
aniseikometer See eikonometer.
aniseikonia A difference in size and/or shape of the visual images of the two eyes. This may be due either to unequal axial lengths of the two eyes, to an unequal distribution of the retinal elements or an inequality of the cortical representation of the two ocular images (basic or intrinsic aniseikonia). It is most frequently induced by lenses of different power used in the correction of anisometropia (refractive aniseikonia). Symptoms include visual discomfort, visual distortion of space and sometimes difficulty in achieving binocular vision, as for example in spectacle corrected unilateral aphakia. Aniseikonia is measured with an eikonometer, although a simple test consists of separating the retinal images of a large target (e.g. a test chart) with prisms and comparing them: placing size lenses in front of one eye until the images appear equal will give an indication of the amount of aniseikonia.
See lens, aniseikonic; magnification, shape; test, New Aniseikonia; test, Turville infinity balance.
aniso-accommodation Unequal accommodative response in the two eyes when fixating an object binocularly. It may result from a disease (e.g. glaucoma, ophthalmoplegia, paralysis of the third nerve, unilateral cataract), uncorrected anisometropia, viewing a near object to the side, toxins affecting one eye more than the other, or trauma.
anisochromatic Not of uniform colour.
anisochromatopsia Deficiency of colour vision in one eye only, or of unequal severity in the two eyes.
anisochromia See heterochromia.
anisocoria Condition in which the pupils of the eyes are not of equal size. Typically one pupil is abnormal and cannot either dilate or constrict. It may be physiological (e.g. in antimetropia) or it may be part of a syndrome, the most common being those of Adie’s and Horner’s. Physiological anisocoria remains constant irrespective of the level of illumination. Anisocoria can occur as a result of injury (e.g. to the iris sphincter muscle), inflammation (e.g. iridocyclitis), diseases of the iris, paralysis of the third nerve, angle-closure glaucoma, systemic diseases (e.g. diabetes, syphilis) or accidental drug instillation into the eye (if the drug or substance has anticholinergic properties the condition is then referred to as anticholinergic mydriasis or ‘atropine’ mydriasis). The search for the cause of anisocoria is facilitated by testing the pupil light reflexes and responses to locally instilled drugs (Fig. A14).
See pupillary defect, efferent; reflex, pupil light; pupillometer.
anisocycloplegia Unequal responses following the binocular instillation of a cycloplegic.
anisohypermetropia Unequal amount of hypermetropia in the two eyes. Syn. compound hypermetropic anisometropia.
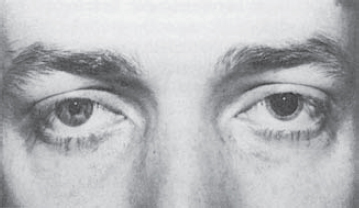
anisometrope A person who has anisometropia.
anisometropia Condition in which the refractive state of a pair of eyes differs and therefore one eye requires a different lens correction from the other. Correction may induce aniseikonia and when the eyes deviate from the optical axes of the lenses, anisophoria. Uncorrected anisometropia of low amounts may cause eyestrain or diplopia. Large amounts rarely cause symptoms as one of the retinal images is typically suppressed or there is amblyopia. Syn. asymmetropia; heterometropia; heteropsia.
See aniso-accommodation; antimetropia; effect, differential prismatic; isometropia.
compound hypermetropic a. See anisohypermetropia.
compound myopic a. See anisomyopia.
mixed a. See antimetropia.
simple a. Anisometropia in which one eye is emmetropic and the other either hypermetropic (simple hypermetropic anisometropia) or myopic (simple myopic anisometropia).
anisomyopia Unequal amount of myopia in the two eyes. Syn. compound myopic anisometropia.
anisophoria 1 . A type of heterophoria in which the amount varies with the direction of gaze. It may be due to: (a) a paresis or spasm of one or more of the extraocular muscles, or (b) an anisometropic spectacle correction in which different prismatic effects induce different phorias when the eyes look in different directions of gaze (this type is called optical anisophoria). 2. A latent deviation in which the angular relationship between the visual axes of the two eyes is not equal depending upon which eye is fixating. This is a form of incomitance.
Table A10
Approximate retinal image size differences (in %) for various anisometropias corrected by spectacles (vertex distance = 12 mm)
| refractive anisometropia† | |||
| anisometropia difference (D) | axial anisometropia (%)* | hyperopic (%) | myopic (%) |
| 1.0 | 0.25 | 1.50 | 1.25 |
| 1.5 | 0.37 | 2.25 | 1.88 |
| 2.0 | 0.50 | 3.00 | 2.50 |
| 2.5 | 0.62 | 3.75 | 3.12 |
| 3.0 | 0.75 | 4.50 | 3.75 |
| 3.5 | 0.87 | 5.25 | 4.38 |
| 4.0 | 1.00 | 6.00 | 5.00 |
| 4.5 | 1.12 | 6.75 | 5.62 |
| 5.0 | 1.25 | 7.50 | 6.25 |
| 5.5 | 1.37 | 8.25 | 6.88 |
| 6.0 | 1.50 | 9.00 | 7.50 |
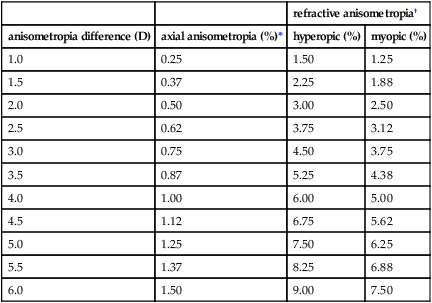
* The two eyes are assumed to be of the same refractive power but of different lengths.
† The two eyes are assumed to be of the same length but of different refractive powers.
See effect, differential, prismatic; incomitance.
anisopia Unequal vision in the two eyes.
anisotropic State of an optical medium in which the optical properties are not the same in all directions, due to the fact that the refractive index is not the same for all directions. An incident ray will be divided, within a uniaxial anisotropic medium, into two refracted rays; an ordinary ray which obeys Snell’s law and an extraordinary ray which follows a different law. Most crystals are anisotropic.
See birefringence; dichroism; isotropic.
ankyloblepharon Partial or complete adhesion of the edge of one eyelid to that of the other. It may occasionally result from a cicatrizing lesion of the eyelid margins or following tarsorrhaphy. It may also be congenital in which case the eyelids are joined together by bands of tissue and this condition is called ankyblepharon filiform adnatum.
ankylosing spondylitis See iridocyclitis; uveitis.
annealing A process of heating material (glass, metal or polymer) and slowly cooling it to avoid internal strain.
annular synechia See synechia, annular.
annulus ciliaris The ring-line structure between the iris and the choroid. Syn. ciliary ring.
annulus of Zinn The common tendon from which arise the four recti muscles of the eye. It surrounds the optic foramen and a part of the medial end of the superior orbital fissure. Syn. tendon of Zinn.
See muscle cone.
anomaloscope An instrument for testing colour vision in which the observer is required to match one-half of a circular field which is illuminated with yellow with a mixture of green and red in the other half. The yellow half can be varied in brightness, while the other may be varied continuously from red to green. A certain combination of the red and green mixture is considered normal, and variations from that mixture indicate anomalous colour vision. With this instrument one can distinguish between a protanope and a protanomal and between a deuteranope and a deuteranomal. Syn. Nagel anomaloscope. Some anomaloscopes also test for blue-yellow colour vision deficiencies, e.g. Pickford–Nicholson anomaloscope.
See colour vision, defective; Rayleigh equation.
anomalous retinal correspondence See retinal correspondence, abnormal.
anomalous trichromatism See trichromatism, anomalous.
anoopsia See hypertropia.
anophthalmia Congenital absence of all tissues of the eyes. It is due to a failure of the outgrowth of the optic vesicle to form the optic cup. However, in many cases some development occurs and there is a rudimentary presence of one or both eyes, such as extreme microphthalmia. Syn. anophthalmos; anophthalmus; anopia.
See cup, optic; microphthalmia; monophthalmia; vesicle, optic.
anophthalmia, unilateral See monophthalmia.
anophthalmos; anophthalmus See anophthalmia.






