CHAPTER 75 Laser Surgery and Operating Room Fires
2 What makes lasers behave differently from each other?
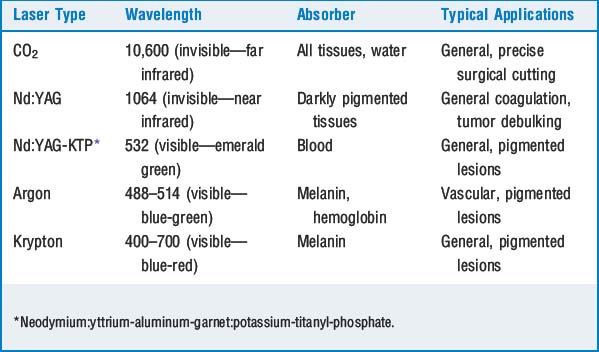
When excited, the source of the laser radiates light of a certain wavelength. The longer the wavelength, the more strongly it is absorbed by the tissue target, and the more shallow is the overall lasing effect. Conversely, the shorter the wavelength, the higher the energy, and the deeper the penetration of the laser light. For example, a carbon dioxide (CO2) laser has a longer wavelength and is absorbed almost entirely at the tissue surface. As a result, precise excision of superficial lesions is possible. Conversely, a neodymium:yttrium-aluminum-garnet (Nd: YAG) laser has a shorter wavelength, deeper penetration, and is useful for heating large tissue masses and tumor debulking (Table 75-1).
3 What are the hazards of lasers?
 The vaporization of tissue and dispersion of diseased particulate matter are hazards for all operating room (OR) personnel. The smoke produced by vaporization of tissues with lasers may be mutagenic, transmit infectious diseases, and cause acute bronchial inflammation.
The vaporization of tissue and dispersion of diseased particulate matter are hazards for all operating room (OR) personnel. The smoke produced by vaporization of tissues with lasers may be mutagenic, transmit infectious diseases, and cause acute bronchial inflammation. A laser beam in contact with flammable materials such as endotracheal tubes, anesthetic gas tubing, surgical drapes, and sponges may cause fires or explosion. Fires result in minimal or no harm to the patient if the situation is handled swiftly but may be catastrophic if not.
A laser beam in contact with flammable materials such as endotracheal tubes, anesthetic gas tubing, surgical drapes, and sponges may cause fires or explosion. Fires result in minimal or no harm to the patient if the situation is handled swiftly but may be catastrophic if not. Although rare, venous gas embolism may occur, especially during laparoscopic or hysteroscopic procedures. Reported cases have been associated primarily with Nd:YAG lasers, in which coolant gases circulate at the probe tips. It is these coolant gases that embolize.
Although rare, venous gas embolism may occur, especially during laparoscopic or hysteroscopic procedures. Reported cases have been associated primarily with Nd:YAG lasers, in which coolant gases circulate at the probe tips. It is these coolant gases that embolize. Inappropriate energy transfer: Laser light vaporizes whatever tissue lies in its path. Precise aim by the surgeon and a cooperative (well-anesthetized, paralyzed) patient are mandatory. In addition, laser light is easily reflected by surgical instruments and may be hazardous to all OR personnel. Laser contact with the eyes may impair vision or cause blindness. The nature of ocular damage depends on the wavelength of the laser light. For example, CO2 lasers cause corneal opacification, whereas Nd:YAG lasers cause damage to the retina. Any plastic lens protects against CO2 laser injury; contact lenses do not. Other lasers require more specialized eye protection.
Inappropriate energy transfer: Laser light vaporizes whatever tissue lies in its path. Precise aim by the surgeon and a cooperative (well-anesthetized, paralyzed) patient are mandatory. In addition, laser light is easily reflected by surgical instruments and may be hazardous to all OR personnel. Laser contact with the eyes may impair vision or cause blindness. The nature of ocular damage depends on the wavelength of the laser light. For example, CO2 lasers cause corneal opacification, whereas Nd:YAG lasers cause damage to the retina. Any plastic lens protects against CO2 laser injury; contact lenses do not. Other lasers require more specialized eye protection.4 What are some unique airway considerations for the patient having laser surgery of the airway?
 Upper airway lesions: In laser resection of upper airway lesions, tracheal intubation is optional. Techniques that do not involve an endotracheal tube allow better visualization of the operative field by the surgeon and also remove potentially flammable materials from the airway. Clearly the airway is being shared by surgeon and anesthesiologist, and a discussion of the operative course before the procedure begins is important.
Upper airway lesions: In laser resection of upper airway lesions, tracheal intubation is optional. Techniques that do not involve an endotracheal tube allow better visualization of the operative field by the surgeon and also remove potentially flammable materials from the airway. Clearly the airway is being shared by surgeon and anesthesiologist, and a discussion of the operative course before the procedure begins is important. Lower airway lesions: The CO2 laser beam is directed at the lesion through a rigid metal bronchoscope, coated with a matte finish to reduce reflected laser light. Ventilation is accomplished through the side arm of the bronchoscope, using saline-soaked gauze to form a seal around the bronchoscope. Jet ventilation is another option. In certain instances (e.g., lower tracheal and bronchial lesions) the laser approach is via fiber optic, and the Nd:YAG laser is required because it can travel through fiber-optic cables, whereas the CO2 laser cannot.
Lower airway lesions: The CO2 laser beam is directed at the lesion through a rigid metal bronchoscope, coated with a matte finish to reduce reflected laser light. Ventilation is accomplished through the side arm of the bronchoscope, using saline-soaked gauze to form a seal around the bronchoscope. Jet ventilation is another option. In certain instances (e.g., lower tracheal and bronchial lesions) the laser approach is via fiber optic, and the Nd:YAG laser is required because it can travel through fiber-optic cables, whereas the CO2 laser cannot.5 Describe ventilation techniques commonly encountered during airway laser surgery
 Jet ventilation: In this technique the surgeon aims a high-velocity jet of O2 at the airway opening. The high flow of O2 entrains room air as a result of the Venturi effect, thus ventilating the lungs with a high volume of O2–air mixture. Ventilation is accomplished by attaching a suction catheter to wall O2 and a Sanderson-type jet injector. This apparatus is mounted to the operating laryngoscope. Sometimes the mass of the airway lesion makes this method impossible. If the jet stream is not aimed in the trachea, gastric dilation may occur. Barotrauma to the airway and subsequent pneumothorax are also risks and may in turn lead to mediastinal or subcutaneous air. An intravenous anesthetic is necessary for this procedure.
Jet ventilation: In this technique the surgeon aims a high-velocity jet of O2 at the airway opening. The high flow of O2 entrains room air as a result of the Venturi effect, thus ventilating the lungs with a high volume of O2–air mixture. Ventilation is accomplished by attaching a suction catheter to wall O2 and a Sanderson-type jet injector. This apparatus is mounted to the operating laryngoscope. Sometimes the mass of the airway lesion makes this method impossible. If the jet stream is not aimed in the trachea, gastric dilation may occur. Barotrauma to the airway and subsequent pneumothorax are also risks and may in turn lead to mediastinal or subcutaneous air. An intravenous anesthetic is necessary for this procedure. Spontaneous ventilation: Allowing the patient to inhale volatile agents via the operating laryngoscope is also an option, although it is not feasible for some procedures. It is difficult to control the depth of anesthesia during spontaneous ventilation, and it is often necessary to paralyze the patient during many airway procedures. Hypoventilation, hypercarbia, and aspiration (surgical debris, secretions, vomitus, and smoke) are additional complications related to both jet and spontaneous ventilation.
Spontaneous ventilation: Allowing the patient to inhale volatile agents via the operating laryngoscope is also an option, although it is not feasible for some procedures. It is difficult to control the depth of anesthesia during spontaneous ventilation, and it is often necessary to paralyze the patient during many airway procedures. Hypoventilation, hypercarbia, and aspiration (surgical debris, secretions, vomitus, and smoke) are additional complications related to both jet and spontaneous ventilation.6 What are the three essential components necessary to create an operating room fire?
8 What strategies can reduce the incidence of airway fires?
 Laser-resistant endotracheal tubes should be chosen. The cuffs should be filled with saline, not air, and it is also recommended that the saline contain a small quantity of methylene blue to help identify rupture of the cuff, should this happen (as in an airway laser procedure). Many laser specialty tubes already have dye crystals within the cuffs. Cuffed tubes are also preferable to uncuffed tubes.
Laser-resistant endotracheal tubes should be chosen. The cuffs should be filled with saline, not air, and it is also recommended that the saline contain a small quantity of methylene blue to help identify rupture of the cuff, should this happen (as in an airway laser procedure). Many laser specialty tubes already have dye crystals within the cuffs. Cuffed tubes are also preferable to uncuffed tubes. Some authors advocate wrapping the endotracheal tube with metal tape; however, this method limits the pliability of the tube and increases the risk of a reflected laser beam and loss of metal tape fragments in the trachea.
Some authors advocate wrapping the endotracheal tube with metal tape; however, this method limits the pliability of the tube and increases the risk of a reflected laser beam and loss of metal tape fragments in the trachea.10 Should an airway fire occur, what are the recommended practices for its management?
1. American Society of Anesthesiologists. Practice advisory for the prevention and management of operating room fires. Anesthesiology. 2008;108:786-801.
2. Rampil I.J. Anesthesia for laser surgery. In: Miller R.D., editor. Miller’s anesthesia. ed 6. Philadelphia: Elsevier Churchill Livingstone; 2005:2573-2587.