CHAPTER 66 Epidural Analgesia and Anesthesia
1 Where is the epidural space? Describe the relevant anatomy
Beyond the epidural space lie the spinal meninges and CSF. The epidural space has its widest point (5 mm) at L2. In addition to the traversing nerve roots, it contains fat, lymphatics, and an extensive venous plexus. Superiorly the space extends to the foramen magnum, where dura is fused to the base of the skull. Caudally it ends at the sacral hiatus. The epidural space can be entered in the cervical, thoracic, lumbar, or sacral regions to provide anesthesia. In pediatric patients the caudal epidural approach is commonly used (see Question 3).
4 What are the advantages of using epidural anesthesia vs. general anesthesia?
 Avoidance of airway manipulation; useful for asthmatics, known difficult airways, and patients with a full stomach
Avoidance of airway manipulation; useful for asthmatics, known difficult airways, and patients with a full stomach Improved bowel motility with less distention; sympathetic blockade provides relatively more parasympathetic tone
Improved bowel motility with less distention; sympathetic blockade provides relatively more parasympathetic tone The patient can be awake during the procedure; desirable for cesarean deliveries and certain arthroscopic procedures
The patient can be awake during the procedure; desirable for cesarean deliveries and certain arthroscopic procedures6 What are the advantages of epidural anesthesia over spinal anesthesia?
 Epidural anesthesia can produce a segmental block focused only on the area of surgery or pain (e.g., during labor or for thoracic procedures).
Epidural anesthesia can produce a segmental block focused only on the area of surgery or pain (e.g., during labor or for thoracic procedures). There is more flexibility in the density of block; if less motor block is desired (for labor analgesia or postoperative pain management), a lower concentration of local anesthetic can be used.
There is more flexibility in the density of block; if less motor block is desired (for labor analgesia or postoperative pain management), a lower concentration of local anesthetic can be used. Theoretically with no hole in the dura there can be no spinal headache; however, an inadvertent dural puncture occurs 0.5% to 4% of the time with the large-bore epidural needle, and about 50% of such patients require treatment for headache. Because newer technology in spinal needles has decreased the incidence of headache requiring treatment to less than 1%, this advantage is probably no longer true.
Theoretically with no hole in the dura there can be no spinal headache; however, an inadvertent dural puncture occurs 0.5% to 4% of the time with the large-bore epidural needle, and about 50% of such patients require treatment for headache. Because newer technology in spinal needles has decreased the incidence of headache requiring treatment to less than 1%, this advantage is probably no longer true.7 What are the disadvantages of epidural compared with spinal anesthesia?
 The induction of epidural anesthesia is slower because of more complex placement, the necessity of incremental dosing of the local anesthetic, and the slower onset of anesthesia in the epidural space.
The induction of epidural anesthesia is slower because of more complex placement, the necessity of incremental dosing of the local anesthetic, and the slower onset of anesthesia in the epidural space.8 What factors should the anesthesiologist address in the preoperative assessment before performing an epidural anesthetic? Should special laboratory tests be performed?
 History
History
9 Describe the technique for performing a lumbar epidural anesthetic
 Resuscitation equipment must be immediately available: oxygen, equipment for positive-pressure ventilation and intubation, and pressors to treat hypotension.
Resuscitation equipment must be immediately available: oxygen, equipment for positive-pressure ventilation and intubation, and pressors to treat hypotension. Place a well-running intravenous (IV) line and give an appropriate preload of fluid to protect against hypotension after sympathetic blockade.
Place a well-running intravenous (IV) line and give an appropriate preload of fluid to protect against hypotension after sympathetic blockade. The patient may be sitting or in a lateral position. The spinous processes should be aligned in the same vertical or horizontal plane and maximally flexed. Administer sedation as deemed appropriate.
The patient may be sitting or in a lateral position. The spinous processes should be aligned in the same vertical or horizontal plane and maximally flexed. Administer sedation as deemed appropriate. For lumbar epidural placement, visualize a line between the iliac crests to locate the L4 spinous process. Palpate the L2-L3, L3-L4, and L4-L5 interspaces and choose the widest or the closest to the desired anesthetic level. For abdominal or thoracic surgeries, know the appropriate level for catheter placement.
For lumbar epidural placement, visualize a line between the iliac crests to locate the L4 spinous process. Palpate the L2-L3, L3-L4, and L4-L5 interspaces and choose the widest or the closest to the desired anesthetic level. For abdominal or thoracic surgeries, know the appropriate level for catheter placement. Make a skin wheal after sterile preparation and draping of the field. The anesthesiologist must wear a hat, mask, and sterile gloves.
Make a skin wheal after sterile preparation and draping of the field. The anesthesiologist must wear a hat, mask, and sterile gloves. The epidural needle is inserted in the midline through the skin wheal until increased resistance from ligaments is felt. Remove the needle stylet and attach a syringe with 3 to 4 ml of air or saline. When the barrel of the syringe is tapped, it should feel firm and bounce back while the tip of the needle is in the ligament.
The epidural needle is inserted in the midline through the skin wheal until increased resistance from ligaments is felt. Remove the needle stylet and attach a syringe with 3 to 4 ml of air or saline. When the barrel of the syringe is tapped, it should feel firm and bounce back while the tip of the needle is in the ligament. Advance several millimeters at a time, tapping the syringe intermittently. The ability to recognize the feel of various layers of ligament comes with experience. Ligamentum flavum is often described as leathery, gritty, or producing a marked increase in resistance. This is the last layer before the epidural space.
Advance several millimeters at a time, tapping the syringe intermittently. The ability to recognize the feel of various layers of ligament comes with experience. Ligamentum flavum is often described as leathery, gritty, or producing a marked increase in resistance. This is the last layer before the epidural space. As the needle passes through ligamentum flavum and enters the epidural space, there is often a pop or give, and the air or fluid in the syringe injects easily; this marks the loss of resistance.
As the needle passes through ligamentum flavum and enters the epidural space, there is often a pop or give, and the air or fluid in the syringe injects easily; this marks the loss of resistance.10 Are there any contraindications to epidural anesthesia?
 Patient refusal. Sometimes a more thorough explanation will allay the patient’s fears and make the technique acceptable. Some common concerns include:
Patient refusal. Sometimes a more thorough explanation will allay the patient’s fears and make the technique acceptable. Some common concerns include:
 Reassure patients that a curtain will block their view and that the desired degree of sedation can be provided. For lumbar epidural placements, explain that the spinal cord ends at about L1 in adults and that the needle is placed below that level. Compare the procedure to the placement of the IV line, which also uses a 16- or 18-G needle, and explain that a local anesthetic will be used in the skin.
Reassure patients that a curtain will block their view and that the desired degree of sedation can be provided. For lumbar epidural placements, explain that the spinal cord ends at about L1 in adults and that the needle is placed below that level. Compare the procedure to the placement of the IV line, which also uses a 16- or 18-G needle, and explain that a local anesthetic will be used in the skin. Sepsis with hemodynamic instability. The induction of sympathetic blockade decreases systemic vascular resistance (SVR) even further. There is also a remote risk of epidural abscess if bacteremic blood is introduced into the epidural space without prior antibiotic coverage.
Sepsis with hemodynamic instability. The induction of sympathetic blockade decreases systemic vascular resistance (SVR) even further. There is also a remote risk of epidural abscess if bacteremic blood is introduced into the epidural space without prior antibiotic coverage. Uncorrected hypovolemia. With ongoing hemorrhage the fall in SVR can produce severe refractory hypotension.
Uncorrected hypovolemia. With ongoing hemorrhage the fall in SVR can produce severe refractory hypotension.11 What are the potential complications of epidural anesthesia? Can they be anticipated or prevented?
 Hypotension caused by sympathetic blockade, which may be prevented by fluid preload and patient positioning.
Hypotension caused by sympathetic blockade, which may be prevented by fluid preload and patient positioning. Intravascular injection of local anesthetic, which can be prevented by aspirating the catheter for blood, injecting a marker such as epinephrine that will cause tachycardia if injected into a vessel, and using incremental dosing (no more than 5 ml at a time). If an intravascular injection occurs:
Intravascular injection of local anesthetic, which can be prevented by aspirating the catheter for blood, injecting a marker such as epinephrine that will cause tachycardia if injected into a vessel, and using incremental dosing (no more than 5 ml at a time). If an intravascular injection occurs:
 Stop convulsions with an induction agent or rapid-acting anticonvulsant. Intubate the trachea, if necessary, for ventilation and airway protection.
Stop convulsions with an induction agent or rapid-acting anticonvulsant. Intubate the trachea, if necessary, for ventilation and airway protection. Subarachnoid injection of a large volume of local anesthetic (“total spinal”). This can be prevented by aspirating the catheter for CSF and giving a small initial dose of local anesthetic to look for rapid onset of sensory block if the drug enters the CSF. (Remember: the onset of an epidural anesthetic is slow.) If a total spinal occurs, treat hypotension with pressors and support ventilation with positive pressure by mask or intubation.
Subarachnoid injection of a large volume of local anesthetic (“total spinal”). This can be prevented by aspirating the catheter for CSF and giving a small initial dose of local anesthetic to look for rapid onset of sensory block if the drug enters the CSF. (Remember: the onset of an epidural anesthetic is slow.) If a total spinal occurs, treat hypotension with pressors and support ventilation with positive pressure by mask or intubation. Postdural puncture headache caused by accidental dural puncture with the large-bore epidural needle. Although not completely preventable, this can be treated in various ways, depending on the preference of the patient and anesthesiologist. Common therapies include analgesics, caffeine, or an epidural blood patch. Factors determining choice of treatment include severity of the headache and how aggressively the patient wishes to be treated. To provide a blood patch, up to 20 ml of the patient’s blood is placed in the epidural space to seal the dural hole and elevate low CSF pressure.
Postdural puncture headache caused by accidental dural puncture with the large-bore epidural needle. Although not completely preventable, this can be treated in various ways, depending on the preference of the patient and anesthesiologist. Common therapies include analgesics, caffeine, or an epidural blood patch. Factors determining choice of treatment include severity of the headache and how aggressively the patient wishes to be treated. To provide a blood patch, up to 20 ml of the patient’s blood is placed in the epidural space to seal the dural hole and elevate low CSF pressure. Epidural hematomas, which are extremely rare and usually occur spontaneously in clinical settings outside of the operating room rather than following neuraxial procedures. When they are associated with regional anesthesia, there is almost always a preexisting coagulopathy. Epidural hematomas present as back pain and leg weakness and must be diagnosed by computed tomography (CT) or magnetic resonance imaging. If the hematoma is not surgically decompressed in 6 to 8 hours, neurologic recovery is rare.
Epidural hematomas, which are extremely rare and usually occur spontaneously in clinical settings outside of the operating room rather than following neuraxial procedures. When they are associated with regional anesthesia, there is almost always a preexisting coagulopathy. Epidural hematomas present as back pain and leg weakness and must be diagnosed by computed tomography (CT) or magnetic resonance imaging. If the hematoma is not surgically decompressed in 6 to 8 hours, neurologic recovery is rare.12 What physiologic changes should be expected after successful initiation of an epidural anesthetic?
 Decrease in blood pressure: Afterload reduction can actually be useful for patients with hypertension or congestive heart failure if preload is maintained.
Decrease in blood pressure: Afterload reduction can actually be useful for patients with hypertension or congestive heart failure if preload is maintained. Changes in heart rate: Tachycardia may occur as cardiac output increases to compensate for a drop in SVR. Bradycardia may occur if blockade above T4 disrupts the cardiac sympathetic accelerator fibers.
Changes in heart rate: Tachycardia may occur as cardiac output increases to compensate for a drop in SVR. Bradycardia may occur if blockade above T4 disrupts the cardiac sympathetic accelerator fibers. Ventilatory changes: In normal patients ventilation is maintained as long as the diaphragm is not impaired (phrenic nerve: C3-C5), but patients may become subjectively dyspneic as they become unable to feel their intercostal muscles. Patients who are dependent on their accessory muscles of respiration may be impaired at lower levels of anesthesia. The ability to cough and protect the airway may be lost even if ventilation is adequate.
Ventilatory changes: In normal patients ventilation is maintained as long as the diaphragm is not impaired (phrenic nerve: C3-C5), but patients may become subjectively dyspneic as they become unable to feel their intercostal muscles. Patients who are dependent on their accessory muscles of respiration may be impaired at lower levels of anesthesia. The ability to cough and protect the airway may be lost even if ventilation is adequate. Bladder distention: Sympathetic blockade and loss of sensation may require catheterization for urinary retention.
Bladder distention: Sympathetic blockade and loss of sensation may require catheterization for urinary retention.13 How does one choose which local anesthetic to use?
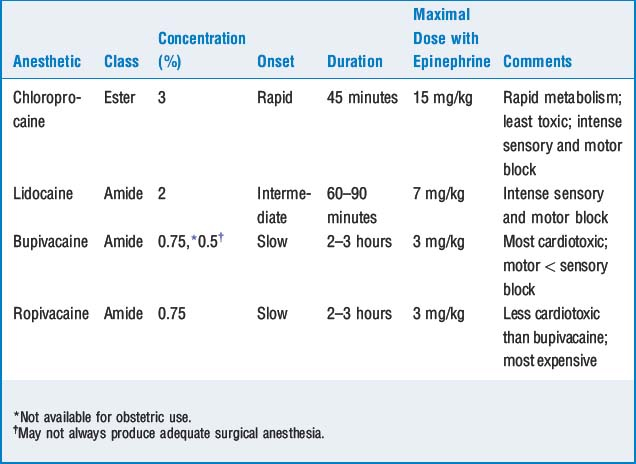
The choice of local anesthetic is usually based on the onset, duration, safety profile, and the special clinical characteristics of the patient and surgical procedure (Table 66-1).
14 Why is epinephrine sometimes combined with the local anesthetic? Should it be included in all cases?
 Improves quality and reliability of blockade, either by increasing the available local anesthetic through decreased uptake or by an intrinsic anesthetic mechanism on central α-adrenergic receptors
Improves quality and reliability of blockade, either by increasing the available local anesthetic through decreased uptake or by an intrinsic anesthetic mechanism on central α-adrenergic receptors15 When should opioids be included in the epidural anesthetic?
KEY POINTS: Epidural Analgesia and Anesthesia 
16 Why can some patients with epidural blocks move around and even walk, whereas others have a dense motor block?
18 How do you determine the level of anesthesia needed for different types of surgeries? What is a segmental block? When is it used?
19 How do you determine the amount of local anesthetic solution used for different procedures? What factors affect spread in the epidural space?
22 What should the anesthesiologist ask the patient postoperatively after an epidural anesthetic?
 Satisfaction with the anesthetic: Was there anything that the patient thought should have been done differently? Assess patient satisfaction and try to correct any misunderstandings.
Satisfaction with the anesthetic: Was there anything that the patient thought should have been done differently? Assess patient satisfaction and try to correct any misunderstandings. Regression of sensory and motor block: Is there any residual blockade? Can the patient ambulate? Does the patient have any problem with bowel or bladder function? Any of these complaints requires a thorough neurologic examination to localize the deficit. Although the complaint is usually caused by residual local anesthetic or nerve compression during the surgical procedure (which often resolves with time), in rare instances further evaluation may be needed. Depending on the pattern and severity of the neurologic dysfunction, a formal neurology consultation, electromyogram, or CT may be needed to rule out pathology in the epidural space (such as hematoma).
Regression of sensory and motor block: Is there any residual blockade? Can the patient ambulate? Does the patient have any problem with bowel or bladder function? Any of these complaints requires a thorough neurologic examination to localize the deficit. Although the complaint is usually caused by residual local anesthetic or nerve compression during the surgical procedure (which often resolves with time), in rare instances further evaluation may be needed. Depending on the pattern and severity of the neurologic dysfunction, a formal neurology consultation, electromyogram, or CT may be needed to rule out pathology in the epidural space (such as hematoma). Complaints of headache: If an accidental dural puncture occurred, the patient should be followed for several days; such headaches can appear up to 1 week later.
Complaints of headache: If an accidental dural puncture occurred, the patient should be followed for several days; such headaches can appear up to 1 week later.