CASE 99
History: A 38-year-old man presents with abdominal distention.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in the figure? (Choose all that apply.)
E. Emphysematous cholecystitis
2. What is the most likely underlying condition resulting in this abnormality?
D. Congenital hepatic fibrosis
3. Why is this finding important for future reference?
4. What is the name given to a chronically occluded portal vein?
ANSWERS
CASE 99
Gallbladder Varices
1. A, C, and D
2. A
3. A
4. A
References
Chawla Y, Dilawari JB, Katariya S. Gallbladder varices in portal vein thrombosis. Am J Roentgenol. 1994;162:643–645.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 211.
Comment
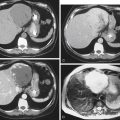
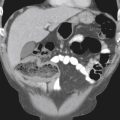
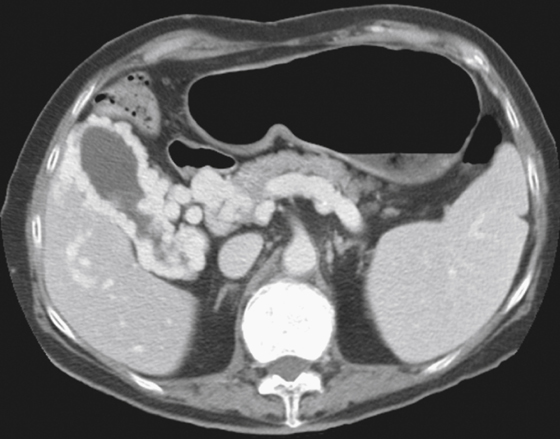
Gallbladder varices are a rare finding in patients with portal hypertension. In the West, the most common cause of portal hypertension is alcoholic cirrhosis of the liver. Fewer patients develop cirrhosis and portal hypertension as a result of portal or splenic vein thrombosis, parasitic infection involving the portal system (schistosomiasis), chronic hepatitis or liver injury secondary to hypervitaminosis A, congenital diseases such as congenital absence of portal vein or congenital hepatic fibrosis, and a host of relatively uncommon prehepatic, hepatic, and posthepatic causes. All these conditions can result in either occlusion or increased pressures in the portal vein, causing collateralization of veins in the splenic circulation. Although the incidence of varices in portal hypertension secondary to hepatic cirrhosis is high (up to 75% to 80%), the most common manifestation is distention of the coronary veins that ascend to the gastroesophageal junction and give rise to uphill varices. Other manifestations of varices are dilated veins in the abdominal wall around the umbilicus (caput medusa sign) and splenorenal shunting. Duplex Doppler ultrasound can gauge the flow in the portal vein, collateralization, and the texture of the liver. CT in patients who are able to have IV contrast material is an excellent way to demonstrate collateralizations without flow quantification, such as obtained in ultrasound, and to evaluate the liver (see figure).