CASE 97
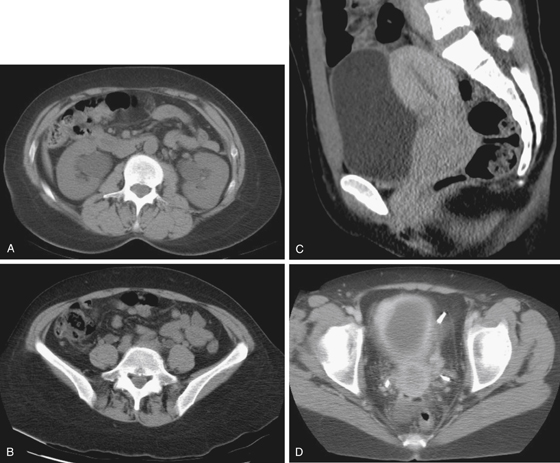
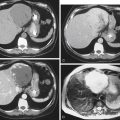
History: A 54-year-old woman presents with lower abdominal pain.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in Figures A and B? (Choose all that apply.)
2. Which of the following statements regarding clinical aspects of cervical carcinoma is true?
A. It is a disease of postmenopausal women.
B. Papillomavirus exposure is a risk factor.
C. Common symptoms are abdominal distention and constipation.
D. It commonly involves the adjacent bladder, producing urinary symptoms.
3. Which of the following statements about the spread of cervical carcinoma is true?
A. The close relationship of the rectum allows invasion from cervical cancer early in the disease.
B. Early spread of cervical carcinoma is usually anterior to the bladder.
C. Hematogenous spread usually occurs first to the vertebral column.
D. Lymph node status is the most important prognostic factor.
4. What is the optimal imaging modality for the local evaluation of cervical carcinoma?
ANSWERS
CASE 97
Cervical Carcinoma with Ureteral Obstruction
1. A, B, D, and E
2. B
3. D
4. D
References
Dahnert W. Radiology Review Manual. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2007. pp 1031-1033
Fielding JR. MR imaging of the female pelvis. Radiol Clin North Am. 2003;41:179–192.
Cross-Reference
Genitourinary Radiology: THE REQUISITES, 2nd ed, pp 305-309.
Comment
Cervical carcinoma is a disease of younger women compared with ovarian carcinoma, which usually affects middle-aged and older women. The most important risk factor is exposure to specific subtypes of the human papillomavirus (HPV). Other risk factors include early age at first intercourse, multiple sexual partners, high-risk male sexual partners, and low socioeconomic status.
Cervical carcinoma usually extends by contiguous spread laterally to the parametrium and to the vagina. Fascial planes delay its spread to adjacent gut (rectum) or bladder; these occur late in the course of the disease. Lymph node assessment is an important role of staging imaging because the state of the lymph nodes is a major prognostic factor. The 5-year survival rates are estimated to be 90% for node-negative disease and 55% for node-positive disease.
Endovaginal and endorectal ultrasonography play a limited role in the imaging of cervical cancer. Cervical cancer is isoechoic to normal cervical tissue; cervical enlargement may be the only sign of the presence of malignancy. Ultrasound can demonstrate uterine or urinary obstruction. CT lacks the contrast resolution to stage low-volume disease. CT is preferred for advanced disease. The superior contrast resolution of MRI makes it an ideal modality for evaluating cervical carcinoma. Cervical carcinoma is identified as a high signal intensity mass on T2-weighted images. This is in stark contrast to the low signal of normal cervical stroma.