Procedure 93 Digital Ray Amputation
![]() See Video 69: Digital Ray Amputation
See Video 69: Digital Ray Amputation
Examination/Imaging
Surgical Anatomy
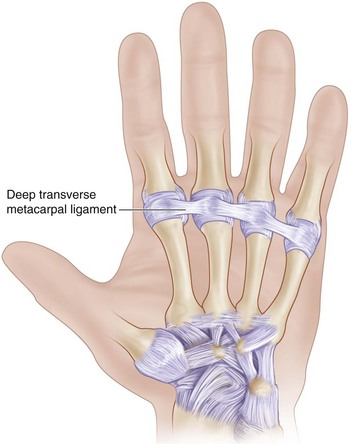
 The deep transverse metacarpal ligament connects the volar plates of the MCP joints of the index, long, ring, and small fingers. The flexor tendons, neurovascular bundles, and lumbrical tendon pass palmar to the deep transverse MCP ligament, whereas the interosseous tendon lies dorsal to it (Fig. 93-3).
The deep transverse metacarpal ligament connects the volar plates of the MCP joints of the index, long, ring, and small fingers. The flexor tendons, neurovascular bundles, and lumbrical tendon pass palmar to the deep transverse MCP ligament, whereas the interosseous tendon lies dorsal to it (Fig. 93-3).
Exposures
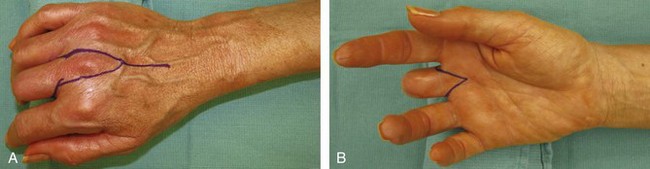
 A racket-shaped incision is marked around the base of the finger. On the dorsum, this incision extends over the proximal metacarpal in a longitudinal fashion (Fig. 93-4A). On the palmar aspect, it is designed as a V (Fig. 93-4B).
A racket-shaped incision is marked around the base of the finger. On the dorsum, this incision extends over the proximal metacarpal in a longitudinal fashion (Fig. 93-4A). On the palmar aspect, it is designed as a V (Fig. 93-4B).
Procedure
Step 1
 The extensor digitorum communis (EDC) tendon is identified on the dorsum, divided at mid-metacarpal shaft, and raised as a distally based tendon (Fig. 93-5). The juncturae to the adjacent fingers are also divided.
The extensor digitorum communis (EDC) tendon is identified on the dorsum, divided at mid-metacarpal shaft, and raised as a distally based tendon (Fig. 93-5). The juncturae to the adjacent fingers are also divided.
Step 2
 The periosteum is incised longitudinally on the dorsum of the metacarpal, and the interosseous muscle on both sides of the metacarpal shaft is separated from the metacarpal, along with the periosteum, to about 1 cm distal to the respective carpometacarpal (CMC) joint to preserve the insertion wrist flexor or extensor tendons.
The periosteum is incised longitudinally on the dorsum of the metacarpal, and the interosseous muscle on both sides of the metacarpal shaft is separated from the metacarpal, along with the periosteum, to about 1 cm distal to the respective carpometacarpal (CMC) joint to preserve the insertion wrist flexor or extensor tendons.
Step 3
 A transverse osteotomy of the metacarpal shaft is done using a saw about 1 cm distal to the CMC joint by preserving the insertions of the ECRL, ECRB, or ECU.
A transverse osteotomy of the metacarpal shaft is done using a saw about 1 cm distal to the CMC joint by preserving the insertions of the ECRL, ECRB, or ECU.
Step 3 Pearls
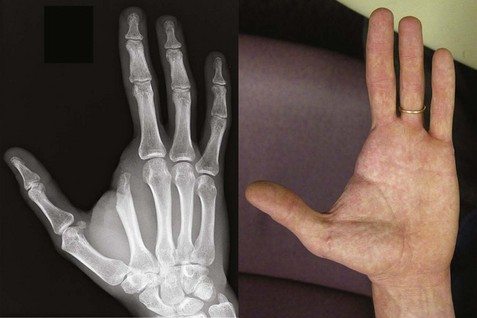
The osteotomy for the index finger is done more distally at the level of the neck of the metacarpal in an oblique fashion; this allows the new web space to have a more natural slope (Fig. 93-6). In addition, it preserves the transverse width of the palm and the origins of the first dorsal interosseous and the adductor pollicis muscle.
The osteotomy of the small finger metacarpal is also done like the index finger (oblique and distally).
Step 5
 The proper digital nerves to the finger undergoing ray amputation are divided distal to the origin from the common digital nerve using a blade and allowed to retract into the proximal soft tissues (Fig. 93-7).
The proper digital nerves to the finger undergoing ray amputation are divided distal to the origin from the common digital nerve using a blade and allowed to retract into the proximal soft tissues (Fig. 93-7).
Step 6
Step 8
Postoperative Care and Expected Outcomes
 A short-arm plaster of Paris volar splint is applied by immobilizing the wrist and the fingers.
A short-arm plaster of Paris volar splint is applied by immobilizing the wrist and the fingers.
 The wound is inspected, sutures are removed, and a thermoplastic splint applied 10 days after the operation.
The wound is inspected, sutures are removed, and a thermoplastic splint applied 10 days after the operation.
 Gentle active finger motion exercises are initiated, with splinting protection for another 4 to 6 weeks.
Gentle active finger motion exercises are initiated, with splinting protection for another 4 to 6 weeks.
 The K-wires are removed 4 to 6 weeks later, and the patient is allowed unrestricted motion.
The K-wires are removed 4 to 6 weeks later, and the patient is allowed unrestricted motion.
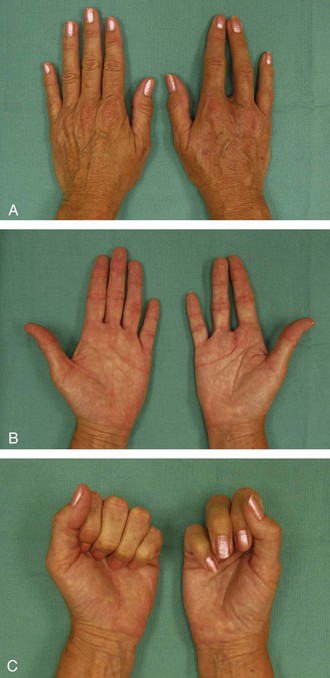
 Figure 93-13 shows the postoperative appearance at 5 months’ follow-up.
Figure 93-13 shows the postoperative appearance at 5 months’ follow-up.
 Most authors have reported 25% to 30% loss of grip strength following ray amputation. The average time off from work is about 13 weeks.
Most authors have reported 25% to 30% loss of grip strength following ray amputation. The average time off from work is about 13 weeks.