CASE 93

History: A 36-year-old woman presents with 8-month history of nocturnal upper abdominal pain.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in the figures? (Choose all that apply.)
2. Which of the following predisposes to the development of hepatic adenoma?
3. How does a hepatic adenoma appear on a sulfur colloid liver scan?
C. Isointense uptake to normal liver
D. Uptake with gallbladder accumulation
4. What is the most common clinical presentation of a hepatic adenoma?
ANSWERS
CASE 93
Hepatic Adenoma
1. A, B, C, and E
2. D
3. A
4. B
References
Grazioli L, Federle MP, Brancatelli G, et al: Hepatic adenomas: imaging and pathologic findings. Radiographics. 2001;21:877–892.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 196.
Comment
Hepatic adenomas are composed of hepatocytes that are loosely arranged, have no portal tracts, and have poorly formed hepatic veins. They form bile to a slight extent. These tumors tend to be large and solitary, often exceeding 10 cm in diameter. They are also quite vascular and because of their poorly developed venous system have a propensity for spontaneous hemorrhage, which is the major clinical presentation. Usually the hemorrhage is internal within the adenoma, and liver produces pain by hepatic capsular distention, such as in this case, but if the hemorrhage spreads into the peritoneal cavity, it could be fatal.
Adenomas occur predominantly in women, usually younger women. They are believed to be estrogen-associated tumors, and their incidence is increased in women taking oral contraceptives. Cessation of oral contraceptive use causes the tumors to shrink. Rarely the tumor occurs spontaneously in men. Men taking anabolic steroids are at increased risk for developing a tumor that is similar to both an adenoma and a hepatocellular carcinoma. Patients with glycogen storage disease also are at greater risk for developing adenomas.
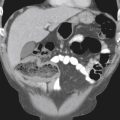
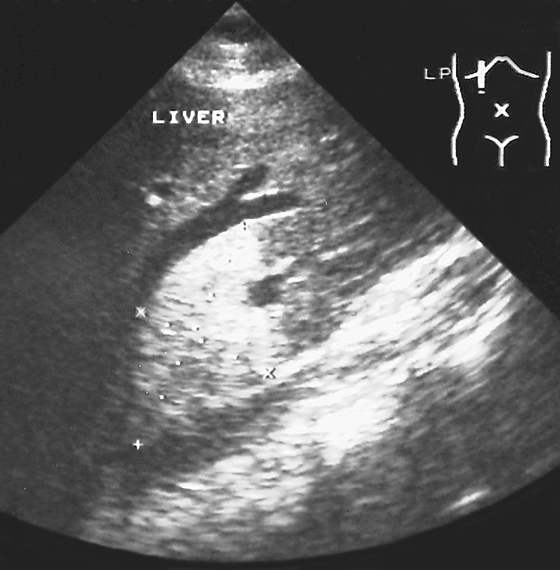
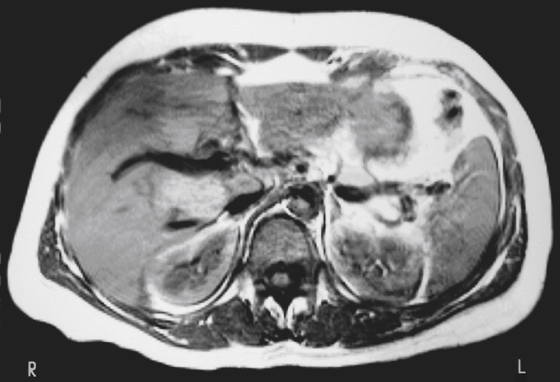
Hepatic adenomas are usually easily identifiable on cross-sectional imaging, but their differentiation from other hepatic tumors is the major concern. Ultrasound typically reveals a large hyperechoic lesion (see figure), which can have central areas of low density caused by hemorrhage or necrosis. On CT the lesion may be hypodense because of glycogen, which is often within the tumor (see figure). After contrast material is injected, the tumor enhances and can become isodense. At the periphery of the tumor are large vessels, which are feeding vessels for the tumor. This finding is apparent on angiography; large peripheral arteries can be seen draped around the tumor and feeding into the center of the mass. Adenomas are visible as cold defects on sulfur colloid scans; this point is important in differentiating the tumor from focal nodular hyperplasia, which appears “hot” on sulfur colloid scan. On MRI, adenomas may be hyperintense on T1-weighted images because of the presence of glycogen and fat in the tumors (see figure).