Procedure 92 Excision of a Dorsal Wrist Ganglion
![]() See Video 68: Treatment of Dorsal Wrist Ganglions
See Video 68: Treatment of Dorsal Wrist Ganglions
Examination/Imaging
Clinical Examination
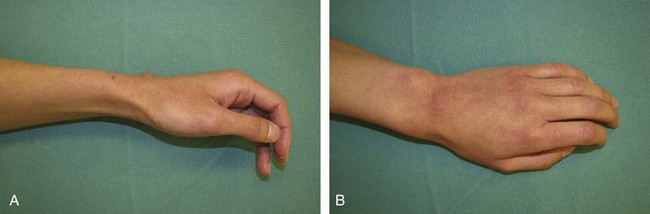
 Patients are usually asymptomatic, and a specific history of antecedent trauma is available only in 10% of patients. Patients with pain or history of trauma should be examined for evidence of scapholunate (SL) instability. This includes tenderness at the SL joint, the Watson scaphoid shift test, and the resisted finger extension test. The resisted finger extension test is done by asking the patient to extend the index and middle fingers against resistance with the wrist partially flexed. These tendons pass over the SL joint, and if there is inflammation of the SL joint with synovitis, resisted extension compresses the area of synovitis, resulting in pain.
Patients are usually asymptomatic, and a specific history of antecedent trauma is available only in 10% of patients. Patients with pain or history of trauma should be examined for evidence of scapholunate (SL) instability. This includes tenderness at the SL joint, the Watson scaphoid shift test, and the resisted finger extension test. The resisted finger extension test is done by asking the patient to extend the index and middle fingers against resistance with the wrist partially flexed. These tendons pass over the SL joint, and if there is inflammation of the SL joint with synovitis, resisted extension compresses the area of synovitis, resulting in pain.
 Pain associated with a ganglion may not go away after excision of the ganglion, and patients must be appropriately counseled.
Pain associated with a ganglion may not go away after excision of the ganglion, and patients must be appropriately counseled.
 The clinical diagnosis of a ganglion is relatively simple and can be confirmed by transillumination. The differential diagnosis for swellings on the dorsum of the hand includes extensor tendon ganglion (moves with the tendon), extensor tendon tenosynovitis (diffuse and moves with the tendon), lipoma, and sebaceous and epidermal cysts (do not transilluminate).
The clinical diagnosis of a ganglion is relatively simple and can be confirmed by transillumination. The differential diagnosis for swellings on the dorsum of the hand includes extensor tendon ganglion (moves with the tendon), extensor tendon tenosynovitis (diffuse and moves with the tendon), lipoma, and sebaceous and epidermal cysts (do not transilluminate).
Surgical Anatomy
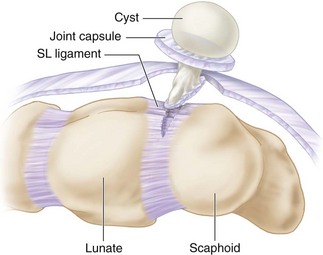
 A dorsal wrist ganglion typically arises from the SL joint and usually presents on the dorsum of the hand over the SL joint (1 to 2 cm distal to Lister tubercle). However, depending on the course of the ganglion and the length of the stalk, it may present anywhere on the dorsum of the hand. Irrespective of anatomic location of the ganglion on the dorsum of the hand, it must be presumed that it is arising from the SL joint and incisions planned accordingly.
A dorsal wrist ganglion typically arises from the SL joint and usually presents on the dorsum of the hand over the SL joint (1 to 2 cm distal to Lister tubercle). However, depending on the course of the ganglion and the length of the stalk, it may present anywhere on the dorsum of the hand. Irrespective of anatomic location of the ganglion on the dorsum of the hand, it must be presumed that it is arising from the SL joint and incisions planned accordingly.
Exposures
 A transverse incision is preferred because it is more aesthetic and the most common indication for excision of the ganglion is appearance. For dorsal wrist ganglions that present in the typical location over the SL joint, the incision is made directly over the ganglion. However, if the ganglion is not located directly over the SL joint, one must plan the incision in such a manner that the ganglion can be dissected and the stalk followed to the SL joint. Occasionally this may need two transverse incisions or a single longitudinal incision. If a clinical diagnosis of a ganglion is doubtful, a longitudinal incision is preferred because it can easily be extended.
A transverse incision is preferred because it is more aesthetic and the most common indication for excision of the ganglion is appearance. For dorsal wrist ganglions that present in the typical location over the SL joint, the incision is made directly over the ganglion. However, if the ganglion is not located directly over the SL joint, one must plan the incision in such a manner that the ganglion can be dissected and the stalk followed to the SL joint. Occasionally this may need two transverse incisions or a single longitudinal incision. If a clinical diagnosis of a ganglion is doubtful, a longitudinal incision is preferred because it can easily be extended.
 A 2-cm transverse incision is made over the skin (Fig. 92-2). The capsule of the ganglion is identified.
A 2-cm transverse incision is made over the skin (Fig. 92-2). The capsule of the ganglion is identified.
Procedure
Step 1: Mobilization of Ganglion Cyst
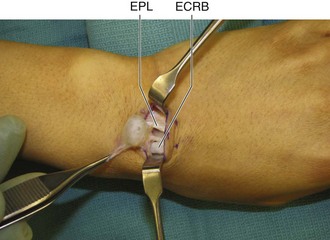
 The portion of the ganglion superficial to the extensor retinaculum is dissected free from the surrounding soft tissue. This is done by holding the ganglion with a blunt forceps and retracting it to one side, while the assistant retracts the skin to the opposite side (Fig. 92-3).
The portion of the ganglion superficial to the extensor retinaculum is dissected free from the surrounding soft tissue. This is done by holding the ganglion with a blunt forceps and retracting it to one side, while the assistant retracts the skin to the opposite side (Fig. 92-3).
 Next the extensor retinaculum adjacent to the ganglion needs to be divided to allow deeper mobilization of the cyst.
Next the extensor retinaculum adjacent to the ganglion needs to be divided to allow deeper mobilization of the cyst.
Step 1 Pearls
Typically the cyst arises between the extensor pollicis longus (EPL) and the extensor digitorum communis (EDC) tendons. These tendons must be retracted radially and ulnarly. Figure 92-3 shows the cyst stalk arising between EPL and extensor carpi radialis brevis (ECRB).
Although excision of the entire cyst keeping the cyst intact is an admirable goal, it is much easier to dissect a punctured cyst. This is best done after the initial dissection through the retinaculum is complete and the cyst capsule is well defined. The cyst can be punctured, the gelatinous fluid evacuated, and the capsule held for further dissection (Fig. 92-4).
Step 2: Excision of Ganglion Cyst
 The cyst is followed deeper, and a rim of joint capsule is incised around the stalk.
The cyst is followed deeper, and a rim of joint capsule is incised around the stalk.
 The capsule is then opened proximal and distal to the stalk.
The capsule is then opened proximal and distal to the stalk.
 The cyst and its stalk along with the rim of joint capsule are dissected down to its attachment on the SL ligament.
The cyst and its stalk along with the rim of joint capsule are dissected down to its attachment on the SL ligament.
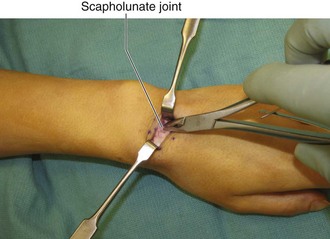
 The cyst and the stalk are excised tangentially off the SL ligament, taking a small portion of the ligament with it (Fig. 92-5).
The cyst and the stalk are excised tangentially off the SL ligament, taking a small portion of the ligament with it (Fig. 92-5).
Step 2 Pearls
The rim of capsular tissue usually measures 1.5 cm in diameter.
Any synovitis of the SL joint or adjoining joints should also be excised (Fig. 92-6).
The edge of the capsule should be cauterized with bipolar cautery before releasing the tourniquet because it is very difficult to cauterize it subsequently.
Postoperative Care and Expected Outcomes
 Patients should be splinted in slight flexion for a week and can resume normal activities thereafter.
Patients should be splinted in slight flexion for a week and can resume normal activities thereafter.
 There is 5% to 10% incidence of recurrence following excision, which usually is a result of incomplete excision. Other complications of surgical treatment of ganglions include wrist stiffness, hypertrophic scar, neuroma formation, and persistent pain.
There is 5% to 10% incidence of recurrence following excision, which usually is a result of incomplete excision. Other complications of surgical treatment of ganglions include wrist stiffness, hypertrophic scar, neuroma formation, and persistent pain.