Procedure 91 Treatment of Mucous Cysts of the Distal Interphalangeal Joint
Indications
 Patients should be advised that cyst excision might not provide complete pain relief in the context of an underlying arthritic joint because pain can be due to either the cyst or the underlying arthritic joint. The only treatment that can ensure a cyst will not recur is distal interphalangeal (DIP) joint arthrodesis.
Patients should be advised that cyst excision might not provide complete pain relief in the context of an underlying arthritic joint because pain can be due to either the cyst or the underlying arthritic joint. The only treatment that can ensure a cyst will not recur is distal interphalangeal (DIP) joint arthrodesis.
Examination/Imaging
Clinical Examination
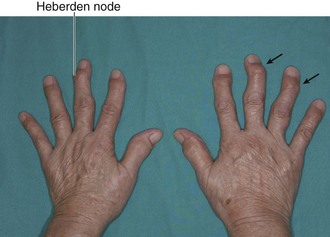
 A mucous cyst is a degenerative cyst of the DIP joint arising as a result of osteoarthritis. It usually occurs between the fifth and seventh decades of life, and patients have DIP joint osteoarthritis including Heberden nodes (Fig. 91-2).
A mucous cyst is a degenerative cyst of the DIP joint arising as a result of osteoarthritis. It usually occurs between the fifth and seventh decades of life, and patients have DIP joint osteoarthritis including Heberden nodes (Fig. 91-2).
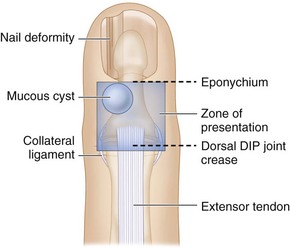
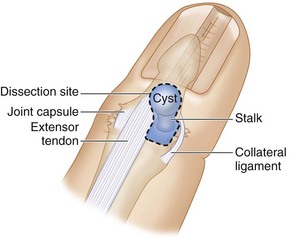
 The cyst may present on the dorsum at the level of the DIP joint on either side between the extensor tendon and the collateral ligament or under the eponychium to cause longitudinal grooving of the nail plate (Fig. 91-3).
The cyst may present on the dorsum at the level of the DIP joint on either side between the extensor tendon and the collateral ligament or under the eponychium to cause longitudinal grooving of the nail plate (Fig. 91-3).
Surgical Anatomy
 The mucous cyst originates from the DIP joint in relation to one of the osteophytes, and the stalk of the cyst passes between the collateral ligament and the extensor insertion to present on the dorsum of the DIP joint. Occasionally, the stalk can connect with another mucous cyst on the opposite side of the DIP joint. This cyst may not be clinically obvious (occult cyst), and the entire DIP joint should be examined during surgery.
The mucous cyst originates from the DIP joint in relation to one of the osteophytes, and the stalk of the cyst passes between the collateral ligament and the extensor insertion to present on the dorsum of the DIP joint. Occasionally, the stalk can connect with another mucous cyst on the opposite side of the DIP joint. This cyst may not be clinically obvious (occult cyst), and the entire DIP joint should be examined during surgery.
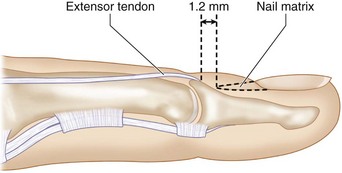
 The terminal extensor insertion is about 1.2 mm from the proximal edge of the nail matrix (Fig. 91-5).
The terminal extensor insertion is about 1.2 mm from the proximal edge of the nail matrix (Fig. 91-5).
Exposures
Procedure
Step 1: Mobilization of Cyst
Step 2: Removal of the Cyst
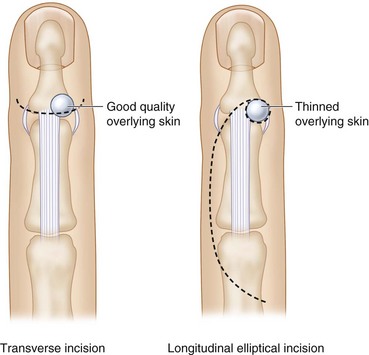
 The cyst is excised en-mass and includes any thinned overlying skin, the cyst and the stalk, and all soft tissue between the extensor tendon and collateral ligament (synovium and joint capsule). (Fig. 91-7 depicts the soft tissue zone that needs to be excised in the dotted line.)
The cyst is excised en-mass and includes any thinned overlying skin, the cyst and the stalk, and all soft tissue between the extensor tendon and collateral ligament (synovium and joint capsule). (Fig. 91-7 depicts the soft tissue zone that needs to be excised in the dotted line.)
Step 2 Pearls
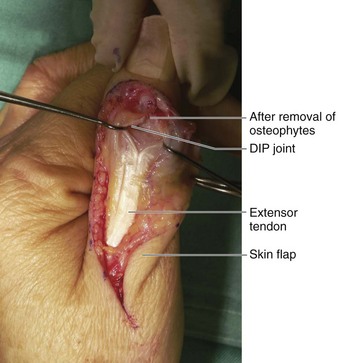
It is important to remove all synovium to allow a clear visualization of the DIP joint.
Both sides of the extensor tendon must be examined for any occult cysts.
It is preferable to leave behind a portion of the cyst wall that is in close relation to the nail bed rather than risk injury to the nail bed from an aggressive débridement.
Step 4: Flap Elevation
Step 5: Skin Closure
 The tourniquet is released and hemostasis secured.
The tourniquet is released and hemostasis secured.
 The flap is advanced into the defect (Fig. 91-9) and sutured with a few 5-0 Ethilon sutures.
The flap is advanced into the defect (Fig. 91-9) and sutured with a few 5-0 Ethilon sutures.
Step 5 Pearls
It is better to close the skin loosely and leave any residual skin defects to heal by secondary intention instead of attempting a watertight closure.
A Xeroform dressing with overlying gauze is applied as a wick to absorb any residual blood. A volar finger splint is applied to keep the DIP joint straight.
Postoperative Care and Expected Outcomes
 The splint is used to immobilize the DIP joint for 5 to 7 days, and the patient is asked to start gentle active range-of-motion exercises thereafter.
The splint is used to immobilize the DIP joint for 5 to 7 days, and the patient is asked to start gentle active range-of-motion exercises thereafter.
 Surgical excision has a high success rate (>90%) and low recurrence rate (2% to 3%), provided that all osteophytes are removed during surgery. A loss of 5 to 20 degrees of motion, joint stiffness, contour changes of the proximal nail fold, and nail dystrophies occur postoperatively in up to 25% of patients.
Surgical excision has a high success rate (>90%) and low recurrence rate (2% to 3%), provided that all osteophytes are removed during surgery. A loss of 5 to 20 degrees of motion, joint stiffness, contour changes of the proximal nail fold, and nail dystrophies occur postoperatively in up to 25% of patients.