Procedure 90 Total Wrist Arthroplasty
Indications
 Destructive and painful wrist conditions resulting from rheumatoid arthritis (RA), osteoarthritis (OA), or trauma
Destructive and painful wrist conditions resulting from rheumatoid arthritis (RA), osteoarthritis (OA), or trauma
 The procedure is contraindicated in patients with the following conditions:
The procedure is contraindicated in patients with the following conditions:
Examination/Imaging
Clinical Examination
 One must evaluate active and passive wrist range of motion to determine any presence of carpal subluxation or dislocation and distal radioulnar (DRU) joint stability.
One must evaluate active and passive wrist range of motion to determine any presence of carpal subluxation or dislocation and distal radioulnar (DRU) joint stability.
 Additionally, the integrity of the flexor and extensor tendons of the wrist and hand should be assessed.
Additionally, the integrity of the flexor and extensor tendons of the wrist and hand should be assessed.
 One must perform a detailed history of the patient’s functional demands, activities, occupation, hobbies, and home circumstances. Patients should be given a trial of splint immobilization, and arthroplasty should be considered for those who find that period of immobilization intolerable.
One must perform a detailed history of the patient’s functional demands, activities, occupation, hobbies, and home circumstances. Patients should be given a trial of splint immobilization, and arthroplasty should be considered for those who find that period of immobilization intolerable.
Imaging
 Posteroanterior, oblique, and lateral radiographs of the wrist are essential to determine extent of wrist destruction. Conditions such as scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) should be noted.
Posteroanterior, oblique, and lateral radiographs of the wrist are essential to determine extent of wrist destruction. Conditions such as scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) should be noted.
 Additional views of the wrist or computed tomography can be obtained to further evaluate arthritis or to assess less obvious intercarpal arthrosis.
Additional views of the wrist or computed tomography can be obtained to further evaluate arthritis or to assess less obvious intercarpal arthrosis.
 Wrist arthroscopy may determine whether limited wrist fusion is preferable. Patients with a preserved radiocarpal joint should be considered for motion-sparing wrist procedures such as four-corner bone fusion or proximal row carpectomy. Rheumatoid patients with radiocarpal arthritis but a preserved midcarpal joint may be eligible for radiolunate or radioscapholunate fusion to maintain midcarpal motion.
Wrist arthroscopy may determine whether limited wrist fusion is preferable. Patients with a preserved radiocarpal joint should be considered for motion-sparing wrist procedures such as four-corner bone fusion or proximal row carpectomy. Rheumatoid patients with radiocarpal arthritis but a preserved midcarpal joint may be eligible for radiolunate or radioscapholunate fusion to maintain midcarpal motion.
Surgical Anatomy
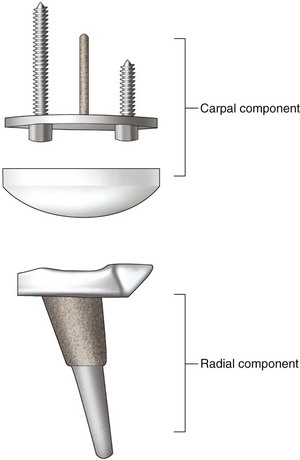
 The implant described in this chapter is the Universal II implant design, which is the most popular total wrist arthroplasty implant used in the United States. Other implant designs are available, but comparative or long-term studies are not presented to determine which implant type is most durable and has the lowest complication rate. The implant design consists of two components. The carpal component is fixated with two screws (Fig. 90-1).
The implant described in this chapter is the Universal II implant design, which is the most popular total wrist arthroplasty implant used in the United States. Other implant designs are available, but comparative or long-term studies are not presented to determine which implant type is most durable and has the lowest complication rate. The implant design consists of two components. The carpal component is fixated with two screws (Fig. 90-1).
 The radial component has an articular inclination of 15 degrees to simulate the anatomy of the distal radius.
The radial component has an articular inclination of 15 degrees to simulate the anatomy of the distal radius.
 Distal and proximal stems are porous coated, which has the theoretical advantage of allowing osseointegration of the components.
Distal and proximal stems are porous coated, which has the theoretical advantage of allowing osseointegration of the components.
 The size of the implant placed can be estimated preoperatively from the wrist radiograph.
The size of the implant placed can be estimated preoperatively from the wrist radiograph.
Exposures
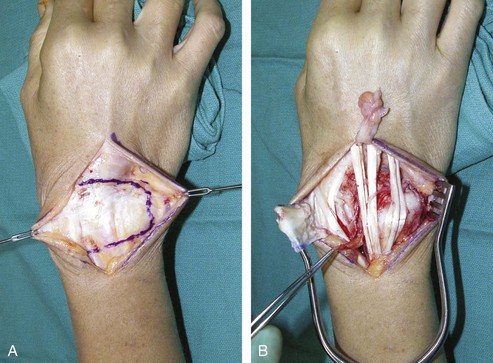
 An 8-cm incision is made on the dorsal wrist, centered on the axis of the long finger metacarpal (Fig. 90-2).
An 8-cm incision is made on the dorsal wrist, centered on the axis of the long finger metacarpal (Fig. 90-2).
 Radial and ulnar skin flaps are elevated, and the extensor retinaculum is visualized.
Radial and ulnar skin flaps are elevated, and the extensor retinaculum is visualized.
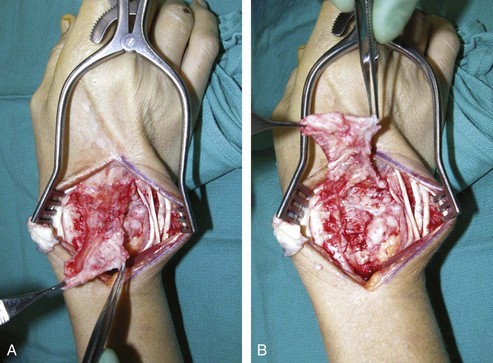
 The entire extensor retinaculum is elevated from the sixth dorsal compartment all the way to the radial attachment over the first compartment. The septa between the compartments are taken down to create a continuous flap of extensor retinaculum. The elevation of the extensor retinaculum stops between the first and second compartments (Fig. 90-3).
The entire extensor retinaculum is elevated from the sixth dorsal compartment all the way to the radial attachment over the first compartment. The septa between the compartments are taken down to create a continuous flap of extensor retinaculum. The elevation of the extensor retinaculum stops between the first and second compartments (Fig. 90-3).
 The extensor tendons are then retracted to expose the wrist.
The extensor tendons are then retracted to expose the wrist.
 The wrist capsule is elevated subperiosteally proximal to the radiocarpal joint as a rectangular, distally base flap (Fig. 90-4A and B). The purpose of the wrist capsular flap is to cover and to provide stout capsular support for the implant.
The wrist capsule is elevated subperiosteally proximal to the radiocarpal joint as a rectangular, distally base flap (Fig. 90-4A and B). The purpose of the wrist capsular flap is to cover and to provide stout capsular support for the implant.
Pearls
If there is arthritic change involving the DRU joint, a Darrach procedure is performed by resecting the distal ulna at a 45-degree oblique apex-ulnar angle. RA patients often have DRU disease, and distal ulna excision is performed to alleviate future problems. For OA patients with only radiocarpal disease, the radioulnar joint can be preserved.
The head of the resected ulna should be saved for bone graft.
The ECRB, and preferably the ECRL tendon as well, should be intact or otherwise reconstructible.
A segment of the posterior interosseous nerve can be excised just proximal to the radiocarpal joint.
Procedure
Step 1
 The wrist is flexed to have an end-on view of the radius articular surface. A bone awl is placed 5 mm below the dorsal articular surface of the radius just slightly radial to the Lister tubercle (Fig. 90-5).
The wrist is flexed to have an end-on view of the radius articular surface. A bone awl is placed 5 mm below the dorsal articular surface of the radius just slightly radial to the Lister tubercle (Fig. 90-5).
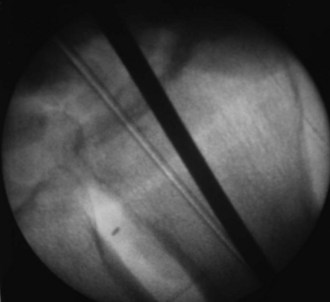
 The radial alignment guide is inserted into the cavity created by the awl, and fluoroscopy is used to confirm that the guide rod is centered in the radius, both in the anteroposterior and lateral planes (Fig. 90-6).
The radial alignment guide is inserted into the cavity created by the awl, and fluoroscopy is used to confirm that the guide rod is centered in the radius, both in the anteroposterior and lateral planes (Fig. 90-6).
Step 2
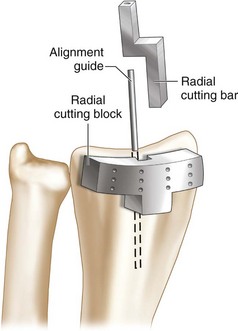
 After confirmation of the position of the alignment guide, the articular surface of the radius is cut. The radial cutting bar is slipped on the alignment guide, and the radial cutting block is then mounted onto the guide bar for positioning (Fig. 90-7). This system requires minimal resection of the articular surface to preserve the stability of the soft tissue envelope around the implant.
After confirmation of the position of the alignment guide, the articular surface of the radius is cut. The radial cutting bar is slipped on the alignment guide, and the radial cutting block is then mounted onto the guide bar for positioning (Fig. 90-7). This system requires minimal resection of the articular surface to preserve the stability of the soft tissue envelope around the implant.
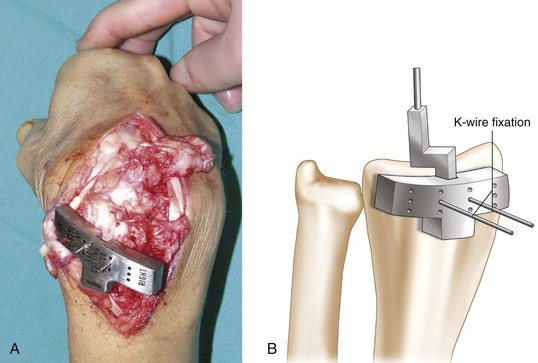
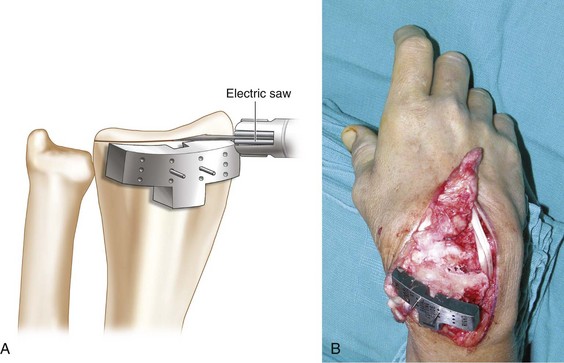
 Kirschner wires are used to stabilize the cutting guide block against the radius. There are three rows of K-wire fixation points that correspond to a distance of about 2 mm between the rows. This is to allow placement of the guide bars more proximally or more distally if necessary to achieve the appropriate amount of bone resection (Fig. 90-8A and B). After scoring the dorsal radius with the oscillating saw, the cutting block and the K-wires are removed, and the radius cut is completed (Fig. 90-9A and B).
Kirschner wires are used to stabilize the cutting guide block against the radius. There are three rows of K-wire fixation points that correspond to a distance of about 2 mm between the rows. This is to allow placement of the guide bars more proximally or more distally if necessary to achieve the appropriate amount of bone resection (Fig. 90-8A and B). After scoring the dorsal radius with the oscillating saw, the cutting block and the K-wires are removed, and the radius cut is completed (Fig. 90-9A and B).
Step 3
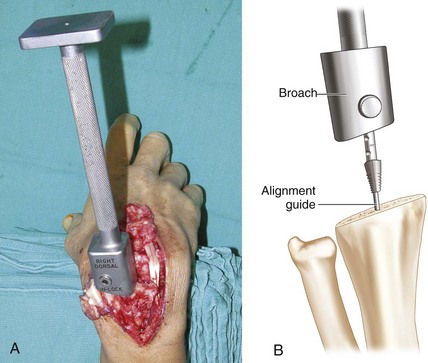
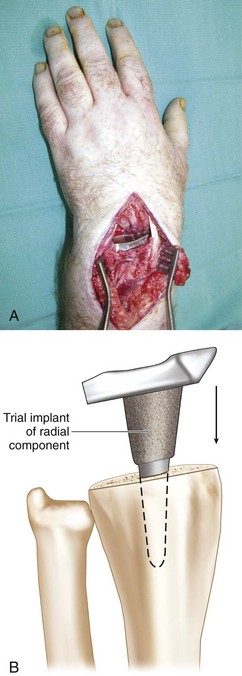
 The guide bar is again inserted into the medullary cavity, and a broach is used to prepare the cavity (Fig. 90-10A and B). A mallet is used to place the broach flush with the cut surface of the radius. A trial implant is inserted and tapped with an impactor to fully seat it (Fig. 90-11A and B). In most cases, this system is press-fit without the use of cement. An appropriate-sized trial implant should not extend past the radial and ulnar corners of the distal radius.
The guide bar is again inserted into the medullary cavity, and a broach is used to prepare the cavity (Fig. 90-10A and B). A mallet is used to place the broach flush with the cut surface of the radius. A trial implant is inserted and tapped with an impactor to fully seat it (Fig. 90-11A and B). In most cases, this system is press-fit without the use of cement. An appropriate-sized trial implant should not extend past the radial and ulnar corners of the distal radius.
Step 4
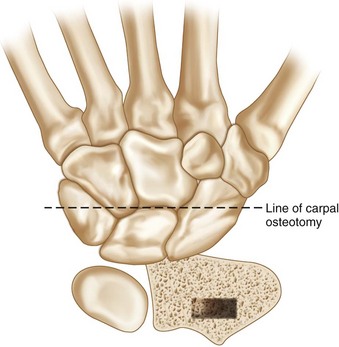
 The carpal osteotomy is now performed at the level of the capitate head and across the waists of both the scaphoid and the triquetrum (Fig. 90-12).
The carpal osteotomy is now performed at the level of the capitate head and across the waists of both the scaphoid and the triquetrum (Fig. 90-12).
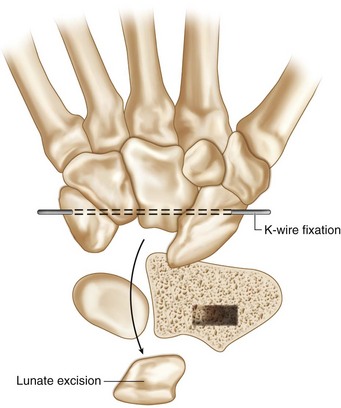
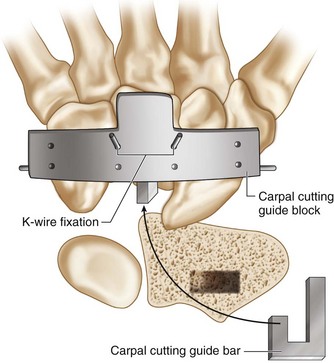
 To facilitate the carpal osteotomy, one should first remove the lunate. If the scaphoid and the triquetrum are mobile, provisional K-wires are placed over the volar cortices of both carpal bones to stabilize them during the procedure and to avoid interfering with the osteotomy (Fig. 90-13).
To facilitate the carpal osteotomy, one should first remove the lunate. If the scaphoid and the triquetrum are mobile, provisional K-wires are placed over the volar cortices of both carpal bones to stabilize them during the procedure and to avoid interfering with the osteotomy (Fig. 90-13).
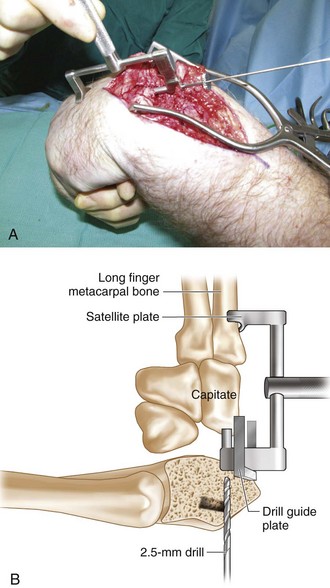
 An appropriate carpal drill guide corresponding to the chosen implant size is selected. The drill guide plate is placed over the long finger metacarpal, and a 2.5-mm drill bit is drilled into the capitate. The depth of the drill hole corresponding to the implant size is marked on the drill (Fig. 90-14A and B).
An appropriate carpal drill guide corresponding to the chosen implant size is selected. The drill guide plate is placed over the long finger metacarpal, and a 2.5-mm drill bit is drilled into the capitate. The depth of the drill hole corresponding to the implant size is marked on the drill (Fig. 90-14A and B).
Step 5
Step 6
 K-wires are placed through the cutting guide block to stabilize the carpal bone similarly to the surgical sequence in the radial component. The osteotomy is made a few millimeters distal to the head of the capitate across the waist of the scaphoid and the proximal portion of the hamate. The carpal component is inserted into the capitate hole. The dorsal edge of the carpal component must be flush with the dorsal cortex of the capitate (Fig. 90-16).
K-wires are placed through the cutting guide block to stabilize the carpal bone similarly to the surgical sequence in the radial component. The osteotomy is made a few millimeters distal to the head of the capitate across the waist of the scaphoid and the proximal portion of the hamate. The carpal component is inserted into the capitate hole. The dorsal edge of the carpal component must be flush with the dorsal cortex of the capitate (Fig. 90-16).
Step 7
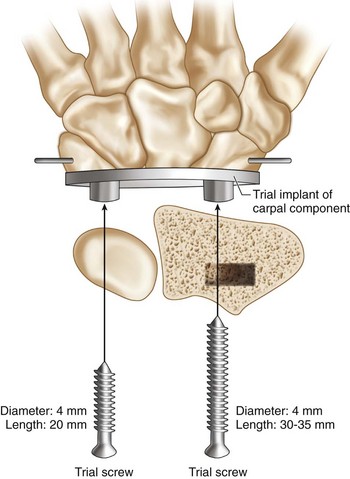
 Screws are inserted into the radial and ulnar screw holes of the carpal component. A drill guide with the saddle sitting on the index metacarpal will be placed over the radial hole of the carpal component. A 30- to 35-mm long 2.5-mm drill hole is drilled into the trapezoid across the carpometacarpal (CMC) joint of the index metacarpal. A 4-mm screw is inserted into the radial screw hole. The ulnar hole is drilled in similar fashion, but the screw does not cross the CMC joint. The 2.5-mm drill bit is drilled into the triquetrum and the hamate. A 4-mm screw that is 20 mm in length is inserted into the triquetrum and the hamate (see Fig. 90-16).
Screws are inserted into the radial and ulnar screw holes of the carpal component. A drill guide with the saddle sitting on the index metacarpal will be placed over the radial hole of the carpal component. A 30- to 35-mm long 2.5-mm drill hole is drilled into the trapezoid across the carpometacarpal (CMC) joint of the index metacarpal. A 4-mm screw is inserted into the radial screw hole. The ulnar hole is drilled in similar fashion, but the screw does not cross the CMC joint. The 2.5-mm drill bit is drilled into the triquetrum and the hamate. A 4-mm screw that is 20 mm in length is inserted into the triquetrum and the hamate (see Fig. 90-16).
 A polyethylene trial component is inserted over the carpal component. One should feel a “pop” when the polyethylene component fits snugly over the metal trial component (Fig. 90-17).
A polyethylene trial component is inserted over the carpal component. One should feel a “pop” when the polyethylene component fits snugly over the metal trial component (Fig. 90-17).
Step 8
 Range of motion and stability are evaluated. The wrist should rest in a neutral position, and one should observe 35 degrees of extension and 35 degrees of flexion with about 10 degrees of radial- and ulnar-deviation angles. If the wrist feels lax, a thicker polyethylene implant is inserted to add more volume to the wrist and impart more stability.
Range of motion and stability are evaluated. The wrist should rest in a neutral position, and one should observe 35 degrees of extension and 35 degrees of flexion with about 10 degrees of radial- and ulnar-deviation angles. If the wrist feels lax, a thicker polyethylene implant is inserted to add more volume to the wrist and impart more stability.
 The trial components are removed. We place drill holes on the dorsal cortex of the radius to accommodate three 2-0 braided permanent sutures for dorsal capsular repair to the radius (Fig. 90-18).
The trial components are removed. We place drill holes on the dorsal cortex of the radius to accommodate three 2-0 braided permanent sutures for dorsal capsular repair to the radius (Fig. 90-18).
Step 8 Pearls
Step-cut tendon lengthening of the flexor carpi ulnaris and the flexor carpi radialis may be needed to achieve proper balance.
If the prosthesis remains tight, additional bone can be resected from the radius.
It is important to perform axial distraction and evaluate for excessive laxity that may lead to implant dislocation.
Step 9
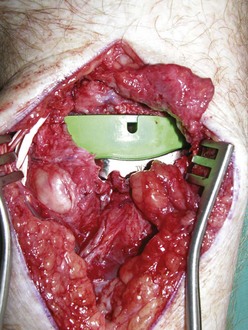
 The carpal component is then inserted into the capitate, and the appropriate length screws are placed.
The carpal component is then inserted into the capitate, and the appropriate length screws are placed.
 The radial component is press-fit and impacted into the radius. An appropriate-sized polyethylene component is fitted over the carpal component using an impactor (Fig. 90-19). One must feel a “pop” as the polyethylene component fits securely into the groove in the carpal component.
The radial component is press-fit and impacted into the radius. An appropriate-sized polyethylene component is fitted over the carpal component using an impactor (Fig. 90-19). One must feel a “pop” as the polyethylene component fits securely into the groove in the carpal component.
 If there is motion between the carpal bones because these bones have not fused previously, a small bur is used to remove the articular surface between the triquetrum, hamate, capitate, scaphoid, and trapezoid. Previously removed bone graft is packed into the carpal intervals to achieve intercarpal fusion.
If there is motion between the carpal bones because these bones have not fused previously, a small bur is used to remove the articular surface between the triquetrum, hamate, capitate, scaphoid, and trapezoid. Previously removed bone graft is packed into the carpal intervals to achieve intercarpal fusion.
Step 10
 The dorsal capsule is reattached to the distal margin of the radius (Fig. 90-20).
The dorsal capsule is reattached to the distal margin of the radius (Fig. 90-20).
 The extensor retinaculum is sutured over the extensor tendons and secured either to the remnant of the retinaculum or over drill holes in the distal ulna if the distal ulna was resected (Fig. 90-21). If the dorsal wrist capsular closure is not sufficiently tight, half of the extensor retinaculum can be placed under the extensor tendons to augment the wrist capsular closure.
The extensor retinaculum is sutured over the extensor tendons and secured either to the remnant of the retinaculum or over drill holes in the distal ulna if the distal ulna was resected (Fig. 90-21). If the dorsal wrist capsular closure is not sufficiently tight, half of the extensor retinaculum can be placed under the extensor tendons to augment the wrist capsular closure.
 Preoperative and postoperative radiographs are shown in Figure 90-22A to D.
Preoperative and postoperative radiographs are shown in Figure 90-22A to D.
Postoperative Care and Expected Outcomes
 The wrist is immobilized in a short-arm splint for 2 to 4 weeks depending on stability of the implant. A removable short-arm splint is used for another 2 to 4 weeks.
The wrist is immobilized in a short-arm splint for 2 to 4 weeks depending on stability of the implant. A removable short-arm splint is used for another 2 to 4 weeks.
 During the splinting period, the patient will start active flexion, extension, pronation, and supination exercises several times a day. After 8 weeks, strengthening and passive exercises can be started. After 2 to 3 months, unrestricted exercises are initiated, but the patient is cautioned against repetitive strong loading and hard work.
During the splinting period, the patient will start active flexion, extension, pronation, and supination exercises several times a day. After 8 weeks, strengthening and passive exercises can be started. After 2 to 3 months, unrestricted exercises are initiated, but the patient is cautioned against repetitive strong loading and hard work.
Cavaliere CM, Chung KC. A systematic review of total wrist arthroplasty compared with total wrist arthrodesis for rheumatoid arthritis. Plast Reconstr Surg. 2008;122:813-825.
Cavaliere CM, Chung KC. A cost-utility analysis of nonsurgical management, total wrist arthroplasty, and total wrist arthrodesis in rheumatoid arthritis. J Hand Surg [Am]. 2010;35:379-391.
Divelbliss BJ, Sollerman C, Adams BD. Early results of the Universal total wrist arthroplasty in rheumatoid arthritis. J Hand Surg [Am]. 2002;27:195-204.
Murphy DM, Khoury JG, Imbriglia JE, Adams BD. Comparison of arthroplasty and arthrodesis for the rheumatoid wrist. J Hand Surg [Am]. 2003;28:570-576.
Radmer S, Andresen R, Sparmann M. Total wrist arthroplasty in patients with rheumatoid arthritis. J Hand Surg [Am]. 2003;28:789-794.
Vicar AJ, Burton RI. Surgical management of the rheumatoid wrist-fusion or arthroplasty. J Hand Surg [Am]. 1986;11:790-797.