CHAPTER 90
Metatarsalgia
Stuart Kigner, DPM; Robert J. Scardina, DPM
Definition
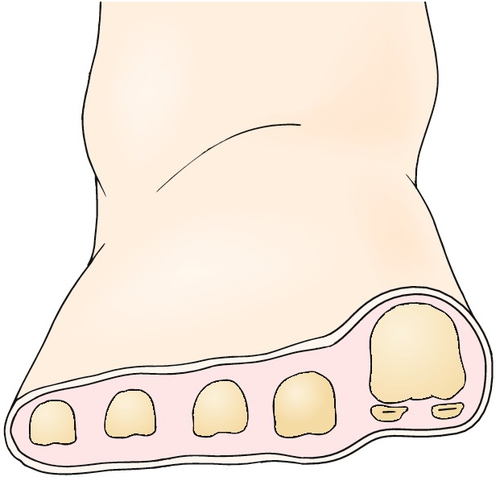
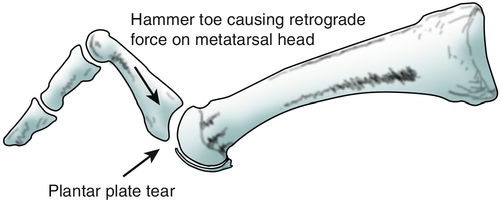
Metatarsalgia refers to pain in the forefoot under the metatarsal head region. Primary metatarsalgia is generally considered the result of mechanical overload of the metatarsal heads, whereas secondary metatarsalgia often has a rheumatic etiology. Primary metatarsalgia may be caused by hallux valgus, hallux rigidus, or sagittal plane first ray hypermobility, which causes a transfer of load to the lateral forefoot and lesser metatarsal heads (Fig. 90.1). A hammer toe with an associated dorsal contracture of a metatarsophalangeal (MTP) joint will cause a retrograde plantar flexion force on the metatarsal head (Fig. 90.2). Bunion surgery, with first metatarsal osteotomy resulting in excessive shortening or elevation of the first metatarsal and with resection of the base of the proximal phalanx of the hallux, is an iatrogenic cause of metatarsalgia [1]. Ankle equinus, leg length discrepancy, scoliosis, kyphosis, neuromuscular disorders, lower extremity trauma, or other foot surgery (elective or post-traumatic) may also result in increased forefoot pressures. Wearing of thin-soled high-heeled shoes may increase the risk for development of metatarsalgia. Although the relative risk of running barefoot or in “minimalist” shoes (compared with traditional running shoes) and developing metatarsalgia is not known, a case series of experienced runners who developed metatarsal stress fractures after transitioning to minimalist running footwear was recently reported [2]. Lieberman [3] has pointed out that runners who transition to barefoot or minimalist shoes may not have strong enough extensor muscles or metatarsal bones, which could lead to an increased risk of metatarsalgia or metatarsal stress fractures.
Secondary metatarsalgia has been associated with rheumatoid arthritis, psoriatic arthritis, reactive arthritis, and systemic lupus erythematosus. MTP joint synovitis may lead to weakening or rupture of the stabilizing structures around the joint, leading to dorsal subluxation of the toes on the lesser metatarsal heads [4]. Degenerative arthritis of the lesser MTP joint may be caused by Freiberg infraction (metatarsal head avascular necrosis).
Symptoms
Plantar forefoot pain is generally aggravated by weight bearing, is often worse during the propulsive phase of gait, and is often localized beneath the second metatarsal head or second MTP joint. Lesser MTP joint morning stiffness may be present. Neuritic radiating pain may occur from irritation, inflammation, or tethering of neighboring plantar intermetatarsal nerves.
Poorly defined pain in the forefoot is a common early symptom in patients with rheumatoid arthritis. Other symptoms include MTP joint symmetric swelling and stiffness after rest.
Physical Examination
The forefoot examination attempts to elicit pain on palpation directly beneath the metatarsal heads or MTP joints, commonly the result of mechanical overload from an unstable first ray or medial column. Pain elicited with lateral compression of neighboring metatarsal heads also suggests a plantar intermetatarsal neuroma. Stress fractures are commonly identified at the metatarsal neck, demonstrated by swelling, palpable pain, or bone fixation callus. Evaluate the excursion and pain of MTP joint passive range of motion and note the presence of swelling. Assess for first metatarsal hypermobility by applying a dorsiflexion force under the first metatarsal head. If hypermobility is present, the first metatarsal head will rise well above the second metatarsal head [5]. Examine for dorsal translation of the proximal phalangeal base on the metatarsal head (drawer test) to identify plantar plate or capsule disruption. Also check for Mulder sign, which may suggest a plantar intermetatarsal neuroma.
While the patient is standing, note the presence of forefoot deformities including hallux valgus, hammer toes, MTP joint dorsal contractures, and medial or lateral subluxation of the toes. The “paper pull-out test” to evaluate toe purchase is performed by asking the patient to flex the toe against a piece of paper placed on the floor under the toe. The test result is positive if the paper cannot be pulled out from under the toe. If there is a V-shaped alignment of adjacent toes noted while the patient is standing, indicative of web space widening, early synovitis [6], plantar intermetatarsal neuroma, or other space-occupying mass may be present. Weight-bearing bilateral or unilateral heel raise while standing barefoot often aggravates metatarsalgia pain. During gait examination, observe for early heel-off, antalgic gait, excessive or insufficient subtalar joint pronation, asymmetry, and lack of toe purchase. Inspect the skin for plantar calluses and their locations. Examine the shoe outsoles and insoles for signs of excessive or uneven wear indicative of areas of elevated pressure or abnormal foot mechanics.
Functional Limitations
Forefoot pain may limit standing, walking, and participation in high-impact activities, such as running or jumping. There will be a limitation to shoe style able to be worn comfortably. Metatarsalgia has its greatest impact on activities requiring prolonged standing or walking on hard floors (e.g., cashier, food preparation, or housekeeping jobs). Sales jobs requiring use of a dress shoe may be difficult. Walking speed may decrease while shopping or accessing public transportation. Recreational activities, such as walking, tennis, basketball, or running on a treadmill on an incline, may be particularly painful.
Diagnostic Studies
Weight-bearing foot radiographs will demonstrate the relative lengths of the metatarsals and transverse plane splaying, if it is present. A forefoot axial view may reveal a structural abnormality of the metatarsal head condyles or relative prolapse of a metatarsal head due to plantar flexion. Metatarsal stress fractures may be identified, but less so on initial radiographs, which may appear unremarkable. Radiographs may also reveal a displaced fracture, foreign body, and stigmata of tumor, osteomyelitis, and noninflammatory or inflammatory arthritis. Ultrasonography and magnetic resonance imaging may be used to evaluate inflammatory arthritis, MTP joint plantar plate disruption, early stress fracture, ligament or tendon tear, abscess, and plantar intermetatarsal neuroma. Laboratory tests may be ordered if inflammatory arthritis or infection is suspected. Although it is not widely used in the office setting, dynamic pedobarography including in-shoe pressure distribution measurement systems may reveal subtle regions of excessive plantar pressure and be used to monitor treatment results.
Treatment
Initial
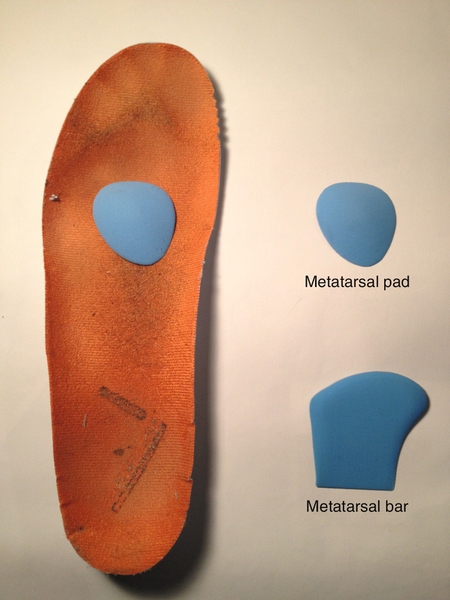
Focal plantar pressure can be reduced by applying a felt or foam rubber aperture pad to off-load a single metatarsal head, or a foam rubber or felt metatarsal pad or bar may be applied just proximal to a single metatarsal head or multiple neighboring metatarsal heads. Prefabricated pads are commercially available. The pads may be applied directly to the foot or to the shoe insole (Fig. 90.3). Cushioned shoe insoles composed of materials such as Plastazote, Poron, and Spenco may be used to replace the entire existing shoe insole. Prefabricated insoles with an incorporated metatarsal pad or bar are also available. Custom fabricated foot orthoses may be designed with a depression under the painful metatarsal head areas or with an incorporated metatarsal pad or bar. Although there is limited scientific evidence to support their use, foot orthoses and running shoes with antitorsional features may address abnormal biomechanical forces causing elevated pressure and shearing under the metatarsal heads. Wearing of a shoe with a full-length stiff outsole or “rocker” outsole under the forefoot is advisable [7]. Shoes should have a low heel height, soft insole, and extra depth to accommodate a custom or commercial cushion insole. For patients who stand most of the day because of their occupation, a cushion floor mat can be used. If a capsule or plantar plate tear is suspected (Fig. 90.2), initial immobilization with a prefabricated walking boot may be indicated. Manually reducible dorsal MTP joint contractures may be addressed by applying tape around the base of the toe and securing it to the bottom of the foot [8]. A prefabricated removable toe splint may also be effective for this condition. Mechanically induced metatarsalgia may be treated with oral nonsteroidal anti-inflammatory drugs or a short tapered course of oral glucocorticoids. Metatarsalgia secondary to rheumatoid or other inflammatory arthritis may be addressed by early use of oral disease-modifying antirheumatic drugs [9].
Rehabilitation
If there is posterior lower leg muscle tightness, gastrocnemius or soleus stretching exercises are recommended [10]. Aquatic exercises and bicycle riding are preferable to exercises involving running and jumping. Decreasing stride length while running or fitness walking may also be helpful. Manipulation may be used to stretch out dorsal MTP joint contractures [8]. After the Weil surgical procedure on a lesser metatarsal, vigorous physical therapy to strengthen the toe flexors and to maintain plantar flexion range of motion soon after surgery has been recommended [11,12]. Rehabilitation after hallux valgus surgery, in an effort to avoid “transfer” metatarsalgia, may include strengthening of the peroneus longus muscle, manipulation to improve hallux plantar flexion, plantar and dorsal sliding of the hallux proximal phalanx, oscillating traction of the first MTP joint, and concentric strengthening of the hallux flexor and extensor muscles [13].
Procedures
A diagnostic local anesthetic block of a plantar intermetatarsal nerve may be performed to differentiate between pain originating from an intermetatarsal neuroma and metatarsalgia pain originating from the metatarsal head or MTP joint.
Surgery
Compared with more traditional elevating or shortening distal lesser metatarsal osteotomies, the Weil osteotomy, involving metatarsal head translation with or without elevation, has been reported to achieve good to excellent results [14]. Metatarsalgia in patients with rheumatoid arthritis has traditionally been addressed by excision of the lesser metatarsal heads combined with fusion of the first MTP joint. Recently, with early institution of disease-modifying antirheumatic drugs resulting in sustained low disease activity and remission, MTP joint–sparing surgery has been recommended. However, at this time, there is limited evidence to support this approach [15]. A rupture of the MTP joint plantar plate may be repaired primarily. Hammer toe surgery involving arthrodesis of the proximal interphalangeal joint combined with surgical capsular release and lengthening of the extensor tendons will decrease retrograde plantar pressure on the metatarsal head. A decrease in metatarsalgia has been reported after isolated gastrocnemius recession [16]. Bunionectomy with first metatarsal osteotomy, designed to decrease the angle between the first and second metatarsals, has been shown to decrease painful calluses under the second metatarsal head [17], and a lengthening osteotomy for an iatrogenic short first metatarsal has resulted in decreased metatarsalgia symptoms [18].
Potential Disease Complications
Metatarsalgia pain may result in functional limitation, including antalgic gait, and may lead to falls in the elderly patient population. Rupture of the plantar plate and collateral ligaments may result in MTP joint instability, dorsal toe subluxation, and transverse plane positional toe deformity, including overlapping toes.
Potential Treatment Complications
Intra-articular corticosteroid injections, especially acetate steroids, are generally not recommended in the presence of lesser MTP joint predislocation syndrome [8]. After corticosteroid injection, MTP joint dislocation [19] and plantar fat pad atrophy have been reported [20]. Other adverse reactions after injection of corticosteroids include skin hypopigmentation at injection site, infection, transient elevated blood glucose concentration, and postinjection flare (pain). Neuroma excision surgery was found to be more technically demanding because of the degree of fibrosis after a series of 20% ethyl alcohol (sclerosing) injections [21], which may also result in adhesive neuritis or “stump” neuroma formation. Topical salicylic acid used to treat painful plantar calluses may injure the skin and lead to open wounds and infection, especially in patients with diabetes. Adverse reactions associated with oral nonsteroidal anti-inflammatory drugs and disease-modifying antirheumatic drugs are listed elsewhere in the text. Shoes with stiff rocker outsoles may cause gait instability and possibly lead to falls, especially in the elderly patient population.
Because of the difficulty in precisely determining the optimal length of a metatarsal when a shortening osteotomy is performed to address metatarsalgia, excessive shortening may result in metatarsalgia of an adjacent metatarsal head and insufficient shortening may lead to some degree of persistent pain [10]. A not uncommon complication of the Weil lesser metatarsal osteotomy is a “floating toe” that does not purchase the floor while standing and walking [10]. Complications of foot orthotic therapy may include mild strain of ligaments, tendons, or muscles; orthotic edge irritation of the skin; and shoe fit difficulty. Improper positioning of a metatarsal pad may result in elevated pressure under the metatarsal head.







