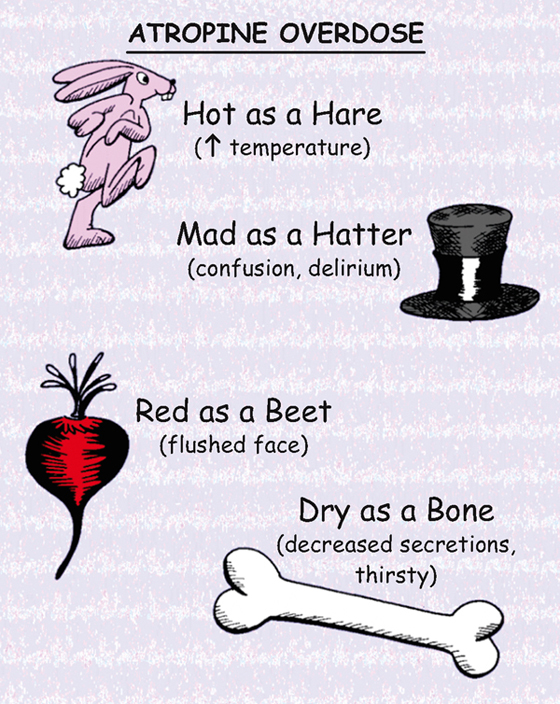
Atropine Overdose
CLASSIFICATION
Anticholinergic, antispasmodic, antidysrhythmic
ACTION
Inhibits action of acetylcholine. Primary affects are on the heart, exocrine glands, smooth muscles, and eye.
USES
• Antidysrhythmic—increases heart rate in symptomatic bradycardia, atrioventricular (AV) block.
• Preoperative—decreases secretions.
• Promotes mydriasis for retinal examination.
• Decreases intestinal hypermotility (diarrhea).
PRECAUTIONS AND CONTRAINDICATIONS
• Gastrointestinal (GI) problems—obstruction, ulcers, colitis, gastroesophageal reflux disease (GERD)
• Glaucoma, tachycardia, bladder obstruction (benign prostatic hyperplasia [BPH])
• Hyperthyroid, liver or renal disease, asthma, hypertension
ADVERSE EFFECTS
• Decreased sweating, which can lead to hyperthermia and flushing
• Central nervous system—toxic doses may cause delirium and hallucinations
• **Blurred vision,** urinary retention, **urinary hesitancy,** constipation
NURSING IMPLICATIONS
2. *Evaluate frequently for urinary retention, especially in older adult men with prostate problems.*
3. *Do not administer if patient has a tachycardia.*
4. *If used preoperatively, explain that warm, dry, flushed feeling may occur.*
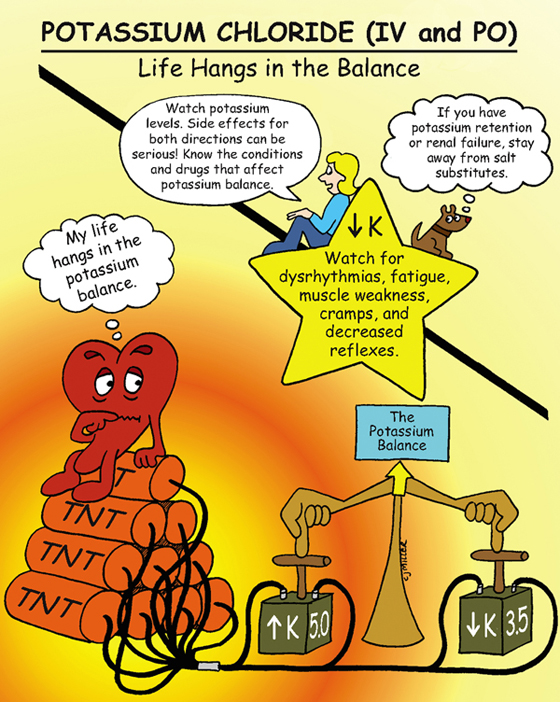
Potassium Chloride (Intravenous and Orally)
CLASSIFICATION
Electrolyte replacement
ACTIONS
Is necessary for nerve impulse conduction; maintains electrical excitability of the heart, and assists to regulate acid-base balance.
USES
• Prevent or correct (or both) potassium deficiency
CONTRAINDICATIONS
PRECAUTIONS
• Acute acidosis resulting in potassium shifts
SIDE EFFECTS
• **Gastrointestinal discomfort—nausea, vomiting, diarrhea**
• Hyperkalemia—(primarily from intravenous [IV] infusion of potassium) †ventricular tachycardia,† confusion, anxiety, dyspnea, weakness, and tingling
NURSING IMPLICATIONS
1. Give oral medication with a full glass of water with or after meals.
2. *Monitor serum potassium (3.5 to 5.0 mEq/L normal value).*
3. *Watch for signs of renal insufficiency—increased creatinine, increased blood urea nitrogen; stop potassium, and notify health care provider if symptoms of renal failure develop.*
4. †IV potassium must always be diluted before administering. Never administer potassium via IV push.†
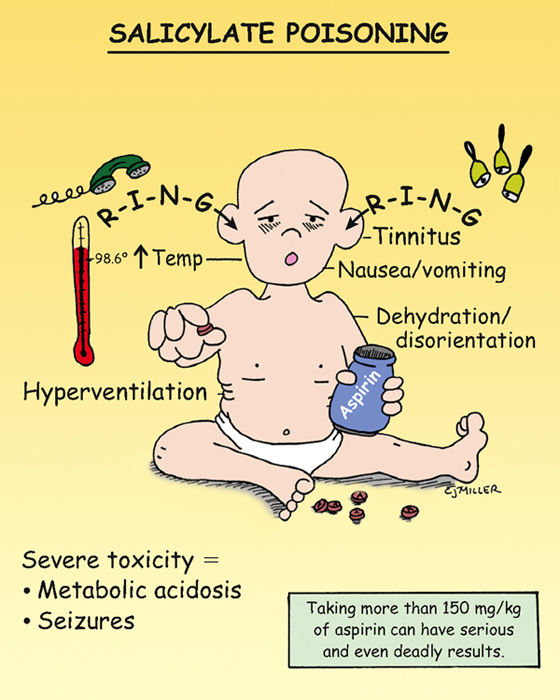
Salicylate Poisoning
PATHOPHYSIOLOGY
Initially, respiratory excitation occurs, producing a respiratory alkalosis. As toxicity occurs, a respiratory depression occurs, resulting in an increase in carbon dioxide levels, which produces respiratory acidosis. The respiratory acidosis is uncompensated because the bicarbonate stores are depleted during the early stages of poisoning. Metabolic acidosis results from the acidity of aspirin, along with an increased production of lactic and pyruvic acids.
SIGNS AND SYMPTOMS
• **Initial symptoms: tinnitus, sweating, headache, and dizziness**
• †Toxicity: hyperthermia, sweating, and dehydration; respiratory depression, resulting in respiratory acidosis, stupor, and coma†
TREATMENT
• Decrease gastrointestinal (GI) absorption—gastric lavage and activated charcoal.
• Provide oxygen or ventilation assistance as necessary.
• Provide dialysis, if necessary. Hemodialysis may be necessary.
NURSING IMPLICATIONS
1. ‡Teach parents safe medication storage.‡
2. ‡Teach parents not to administer aspirin to children who are suspected of having a viral infection, especially chicken pox or influenza.‡
3. *Monitor respiratory status, blood gases, and the progression of symptoms.*
4. *Assist older patients to evaluate the combination of over-the-counter (OTC) medications for the presence of aspirin.*
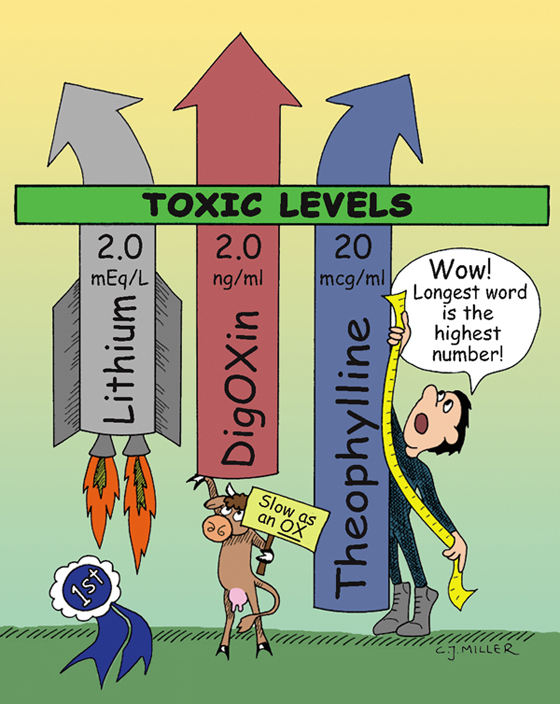
Toxic Levels of Lithium, Digoxin, and Theophylline
LITHIUM
• Therapeutic level: 0.8 to 1.4 mEq/L
• Toxic level: >2.0 mEq/L (levels should be kept below 1.5 mEq/L)
• ‡Levels are routinely monitored every 2 to 3 days initially, then every 1 to 3 months during therapy.‡
• *Sodium depletion is the most common cause of lithium accumulation.*
Signs and Symptoms
• **Side effects (at therapeutic levels) include fine hand tremors, polyuria, thirst, transient fatigue, muscle weakness, headache, and memory impairment.**
• Gastrointestinal (GI) effects are nausea, diarrhea, and anorexia.
• Effects of †acute toxicity† (above 2.0 mEq/L) include ataxia, high output of dilute urine, electrocardiographic (ECG) changes, tinnitus, blurred vision, †severe hypotension,† and †seizures.† Symptoms may progress to †coma† and †death.†
DIGOXIN
• Optimal level: 0.5 to 0.8 ng/ml
• *Hypokalemia is the most common predisposing factor to toxicity.*
• ‡Patients should not interchange various brands because of variations in absorption.‡
Signs and Symptoms
• **GI signs include anorexia and nausea and vomiting.**
• Central nervous system signs are **fatigue** and visual disturbances.
• †Dysrhythmias—digoxin can mimic most dysrhythmias; if cardiac rate or rhythm changes during therapy, the health care provider should be notified.†
THEOPHYLLINE
• Optimal level: 5 to 15 mcg/ml
Signs and Symptoms
• *Aminophylline is the preferred form for intravenous (IV) administration. It must infuse slowly (25 mg/min or slower); too rapid IV infusion may cause hypotension, tachycardia, hyperventilation, and seizures.*
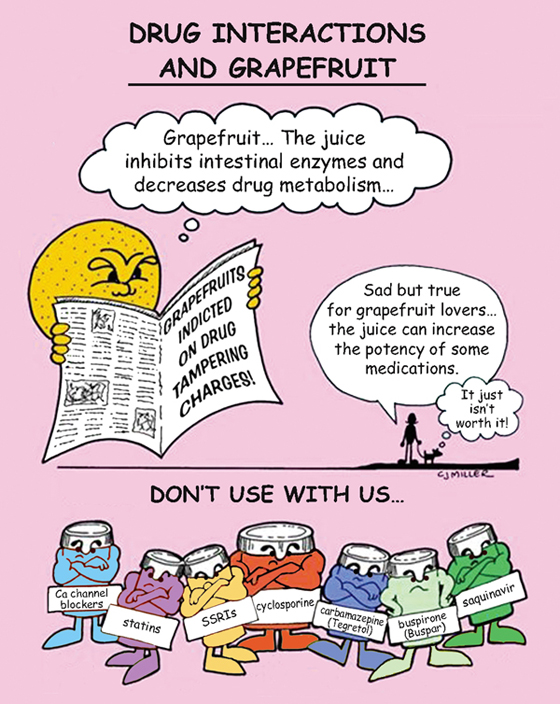
Drug Interactions and Grapefruit
CAUTION
*Grapefruit inhibits intestinal enzymes and decreases absorption with Tegretol, Buspar, calcium channel blockers, benzodiazepines (Halcion, Valium), cyclosporine (Sandimmune), saquinavir (Invirase), and SSRIs.*
EFFECT OF GRAPEFRUIT ON MEDICATIONS
Grapefruit and grapefruit juice are metabolized in the liver by the same enzyme (CYP3A4, an isoenzyme of cytochrome P450) that metabolizes many drugs. When the liver has too many substances to metabolize, the enzymes focus on metabolizing grapefruit while ignoring the medication.
†Because the medication is not being metabolized, it can build up to a dangerous level and can lead to intense peak effects.† The more grapefruit juice the patient drinks, the greater the inhibition.
NURSING IMPLICATIONS
1. ‡Teach the patient to avoid foods containing grapefruit or grapefruit juice with prescribed drugs such as calcium channel blockers, Tegretol, Buspar, selective serotonin uptake inhibitors (SSRIs), and statin medications.‡
2. *Does not affect intravenous (IV) preparations of the medications.*
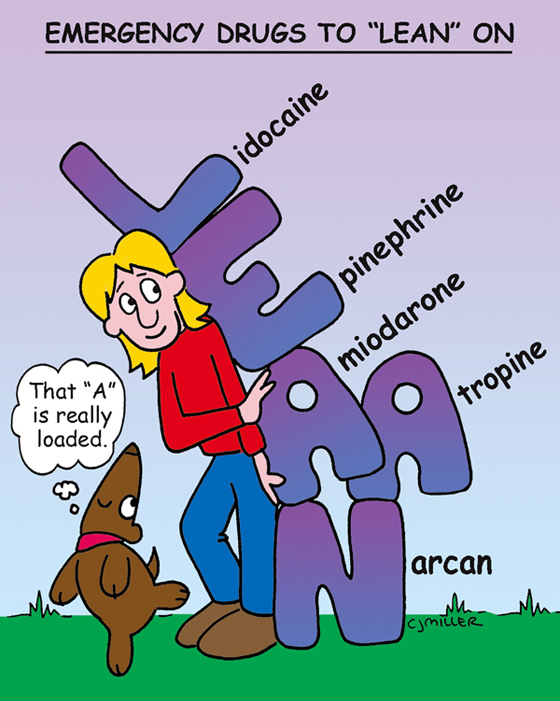
Emergency Drugs
LIDOCAINE
Classification: Antidysrhythmic, local anesthetic
Actions: Slows conduction, reduces automaticity, and increases repolarization of cardiac cycle. As an anesthetic, **lidocaine causes temporary loss of feeling and sensation.**
Uses: Intravenous (IV) preparation only for ventricular dysrhythmias (frequent premature ventricular beats, ventricular tachycardia)
EPINEPHRINE (ADRENALIN)
Classification: Adrenergic agonist, catecholamine
Actions: Causes vasoconstriction, increases heart rate and blood pressure, is a bronchodilator, is the *treatment of choice for anaphylactic reactions.*
Uses: For bronchodilation in patients with acute asthma; to treat hypersensitivity, anaphylactic reactions, cardiac arrest
ATROPINE
Classification: Anticholinergic, antidysrhythmic
Actions: Selectively blocks cholinergic receptors; increases heart rate in bradycardia; decreases secretions.
Uses: To treat symptomatic bradycardia; **to decrease respiratory secretions;** to reverse effects of anticholinesterase medications
AMIODARONE (CORDARONE)
Classification: Antidysrhythmic
Actions: Decreases atrioventricular (AV) and sinus node function, and suppresses dysrhythmias.
Uses: Ventricular tachycardia and fibrillation
NALOXONE (NARCAN)
Classification: Narcotic (opioid) antagonist
Actions: Blocks narcotic effects; *reverses opiate-induced sleep or sedation;* increases respiratory rate and blood pressure.
Uses: Reverses overdose by opioid analgesics (morphine, demerol, OxyContin); treats opioid-induced respiratory depression; *may be used in neonates to counteract or treat effects from narcotics given to mother during labor.*
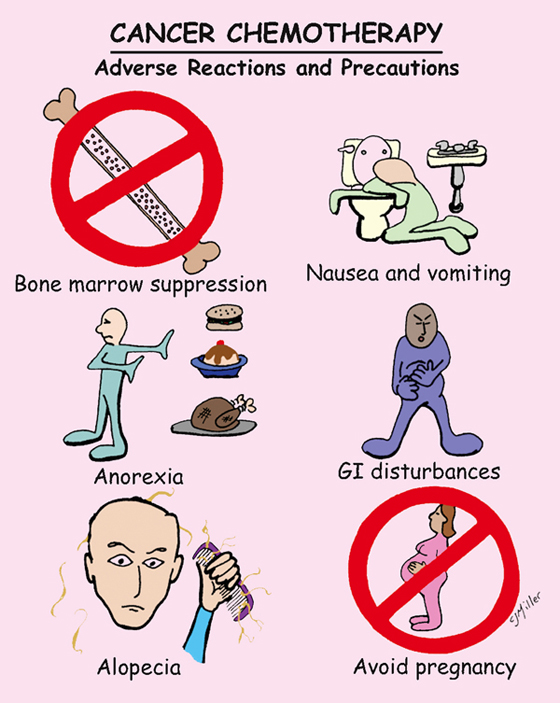
Cancer Chemotherapy: Adverse Reactions and Precautions
ACTIONS
Action occurs during the sequence of the cell cycle. Anticancer agents affect cells during any phase of the cell cycle. Other drugs are effective only during a specific phase of the cell cycle. Rapidly dividing cells are more vulnerable to chemotherapy.
DOSAGE, HANDLING, AND ADMINISTRATION
• Medication doses are individualized for each patient.
• *Because of the hazardous nature of these medications, it is important that direct contact with the skin, eyes, and mucous membrane is avoided.*
• Drugs are frequently given in combination to improve effectiveness of response.
SIDE EFFECTS
• Medications are harmful to normal tissue because they lack selectivity; they kill target cancer cells, but they also kill normal cells.
• **Bone marrow suppression: anemia (loss of erythrocytes), thrombocytopenia (bleeding from loss of platelets), neutropenia (infection from loss of neutrophils) may result.**
• **Gastrointestinal (GI) disturbances: includes stomatitis, nausea and vomiting, anorexia, and diarrhea.**
• **Alopecia results from injury to hair follicle, grows back in 1 to 2 months after treatment.**
• **Hyperuricemia may cause renal injury secondary to a deposit of urate crystals.**
• Reproductive toxicity: fetus is susceptible to injury and malformation.
• *Local injury may occur from extravasation of the anticancer drug.*
NURSING IMPLICATIONS
1. *Monitor for bone marrow suppression; may require an alteration of medication dose.*
2. ‡Side effects are expected, and patient is frequently taught how to manage the problems.‡
3. *Observe closely for signs of infection.*
4. ‡Routine laboratory blood tests are extremely important.‡
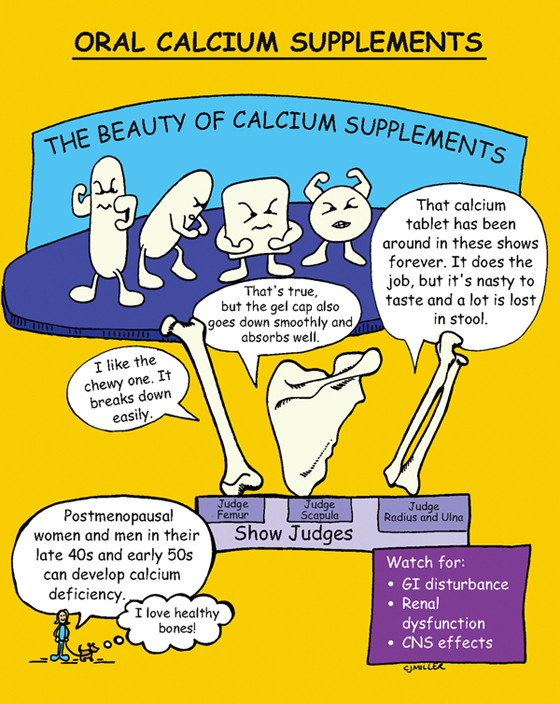
Oral Calcium Supplements
CLASSIFICATION
Calcium salt
ACTION
Is necessary for the normal function of the nervous, muscular, and skeletal systems.
USES
• Prophylactic for osteoporosis
CONTRAINDICATIONS AND PRECAUTIONS
• Presence or history of calcium renal calculi
SIDE EFFECTS
• Gastrointestinal (GI) disturbances (nausea, vomiting, **constipation)**
• Renal dysfunction (polyuria, stones)
• Central nervous system (CNS) effects (lethargy, depression)
NURSING IMPLICATIONS
1. ‡Encourage fluids with medication.‡
2. ‡Increase fiber-containing foods to decrease constipation.‡
3. ‡Encourage patient to check with health care provider regarding calcium and cardiac medications.‡
4. *Calcium carbonate has the highest percentage of calcium; however, calcium citrate preparations are more completely absorbed.*
5. *To maintain adequate absorption and decrease the loss of calcium, the patient should not take more than 600 mg at one time.*
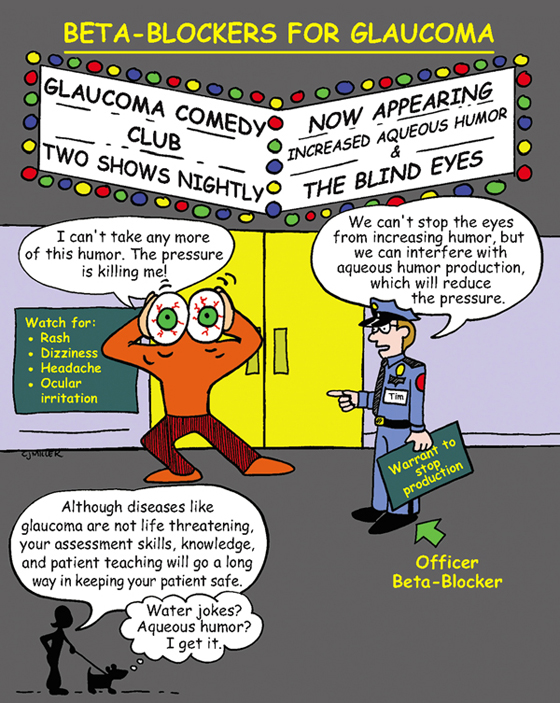
Beta-Blocking Drugs for Glaucoma Betaxolol (Betoptic), Timolol (Timoptic), Carteolol (Ocupress)
CLASSIFICATION
Beta-adrenergic blocking agents
ACTIONS
Is most commonly used as an ophthalmic gel or drops to reduce production of aqueous humor to promote a decrease in intraocular pressure. When systemically absorbed, blockage of beta1-receptors may cause bradycardia; blockage of beta2 receptors in the lung may cause bronchospasm.
USES
CONTRAINDICATIONS
• Severe bradycardia, greater than first-degree heart block
PRECAUTIONS
• Asthma or air-flow limitations
SIDE EFFECTS
• Decreased visual acuity, ocular burning
• Possible bradycardia and pulmonary implications if medication is absorbed systemically
NURSING IMPLICATIONS
1. Check patient’s medical history for chronic systemic diseases that may be associated with the eye disorder.
2. ‡Teach patient how to administer eye drops correctly.‡
3. *Assess patient for systemic absorption of medication (bradycardia, hypotension).*
4. ‡Teach patient to apply slight pressure at the inner canthus for 1 minute after instillation. This pressure will help decrease the systemic absorption of the medication.‡
5. ‡Patient should avoid over-the-counter (OTC) nasal decongestants or cold preparations.‡
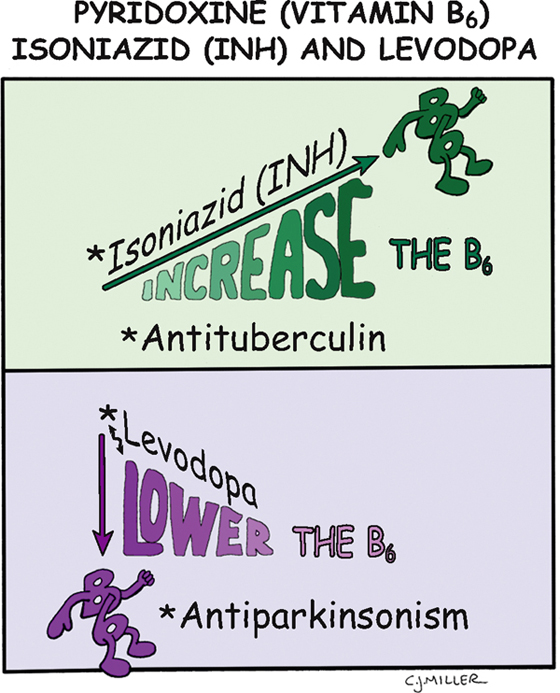
Pyridoxine (Vitamin B6): Isoniazid (INH) and Levodopa
CLASSIFICATION
Vitamin B6 is a member of the vitamin B complex of water-soluble vitamins.
ACTION
Functions as a coenzyme in the metabolism of amino acids and proteins; it must be converted to an active form of pyridoxal phosphate.
DEFICIENCIES
• *Are common among alcoholics.*
• Isoniazid (INH) prevents conversion to active form.
DRUG INTERACTIONS
• *Vitamin B6 interferes with the utilization of levodopa or carbidopa-levodopa, which are common medications in the treatment of Parkinson disease. Patients taking levodopa should not take vitamin B6 supplements.*
SIDE EFFECTS
• Low dose: no noticeable effect
• Extremely high dose: sensory neuropathy—ataxia and numbness to hands and feet
NURSING IMPLICATIONS
1. ‡Patients taking INH need an increased intake of vitamin B6 to prevent deficiency.‡
2. ‡Patients taking levodopa need a decreased intake of vitamin B6, which reverses the effects of the levodopa.‡
3. Evaluate nutritional adequacy.
4. *Perform neurologic checks in the patient with vitamin B6 issues.*
5. ‡Teach patient about dietary sources—meats and fish, especially organ meats; heavily fortified cereals; and soy-based products.†
6. *Deficiency most often occurs in combination with deficiency of other B vitamins in patients who abuse alcohol.*