CASE 9

1. What should be included in the differential diagnosis of the acute aortic syndrome? (Choose all that apply.)
B. Severe aortic regurgitation
B. Descending thoracic aortic aneurysm
3. How should this abnormality be classified?
4. What is the appropriate management of this patient?
A. Surgery
B. Nothing
ANSWERS
Reference
Baikoussis NG, Apostolakis EE, Siminelakis SN, et al. Intramural haematoma of the thoracic aorta: who’s to be alerted the cardiologist or the cardiac surgeon? J Cardiothorac Surg. 2009;4:54.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 407–411.
Comment
Classification and Management
Classification of intramural hematoma is similar to classification of aortic dissection; intramural hematoma involving the ascending aorta is Stanford type A, and intramural hematoma not involving the ascending aorta is Stanford type B. Differentiation between these two types is important because it determines the most appropriate treatment and is predictive of prognosis. Type A intramural hematoma has a high rate of complications (aortic rupture, pericardial tamponade, progression to aortic dissection, and death) and is generally treated surgically. Type B hematomas infrequently have complications, often resolve without intervention, and are usually managed conservatively. Occasionally, complicated type B intramural hematoma may require surgical or endograft therapy.
Complications
Intramural hematoma is caused by rupture of the vasa vasorum leading to bleeding within the media of the aortic wall. In contrast to aortic dissection, there is no intimal tear. The main complications of intramural hematoma include aortic rupture, hemorrhagic pericardial tamponade, progression to aortic dissection, and aneurysm formation.
Imaging
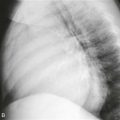
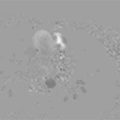
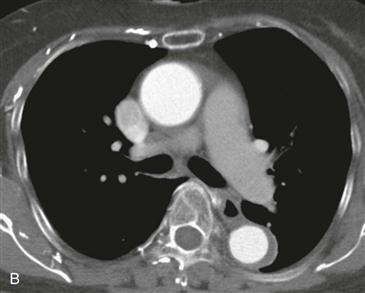
In this case, non–contrast-enhanced CT scan showed a crescent of high density within the wall of the descending thoracic aorta, consistent with a Stanford type B intramural hematoma (Fig. A). Axial contrast-enhanced CT scan performed 3 days earlier than Fig. 1 showed thickening of the descending thoracic aortic wall (Fig. B).