Procedure 89 Total Wrist Fusion
![]() See Video 67: Total Wrist Fusion
See Video 67: Total Wrist Fusion
Indications
Exposures
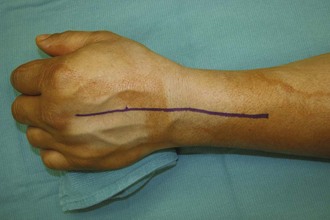
 A dorsal midline incision is used, centered at the radiocarpal joint and extending past the midpoint of the long finger metacarpal and proximally, about 5 cm proximal to the Lister tubercle (Fig. 89-2).
A dorsal midline incision is used, centered at the radiocarpal joint and extending past the midpoint of the long finger metacarpal and proximally, about 5 cm proximal to the Lister tubercle (Fig. 89-2).
 Flaps are elevated, keeping cutaneous nerves in the flaps (Fig. 89-3).
Flaps are elevated, keeping cutaneous nerves in the flaps (Fig. 89-3).
 Incise third dorsal compartment and retract the extensor pollicis longus (EPL) tendon (Fig. 89-4).
Incise third dorsal compartment and retract the extensor pollicis longus (EPL) tendon (Fig. 89-4).
 Raise retinacular flaps, exposing the second to fifth extensor compartments.
Raise retinacular flaps, exposing the second to fifth extensor compartments.
 The posterior interosseous nerve (PIN) is located on the floor of the fourth extensor compartment. A PIN excision is performed after retracting the extensor tendons.
The posterior interosseous nerve (PIN) is located on the floor of the fourth extensor compartment. A PIN excision is performed after retracting the extensor tendons.
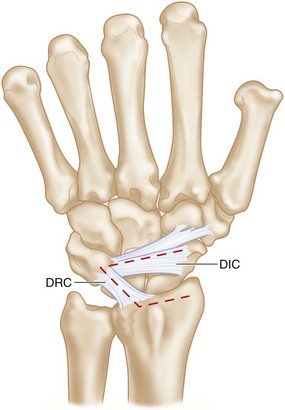
 A radially based capsular flap is formed by incising the dorsal intercarpal and dorsal radiocarpal ligaments and elevating them off the dorsal triquetrum (Fig. 89-5).
A radially based capsular flap is formed by incising the dorsal intercarpal and dorsal radiocarpal ligaments and elevating them off the dorsal triquetrum (Fig. 89-5).
 Subperiosteal dissection is used to expose the dorsal radius, the carpus, and the long finger metacarpal (Fig. 89-6).
Subperiosteal dissection is used to expose the dorsal radius, the carpus, and the long finger metacarpal (Fig. 89-6).
Pearls
The extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) tendons can be released from the dorsal aspects of index finger and long finger metacarpals, respectively, and used to augment soft tissue coverage of the hardware when closing the capsular flap.
An alternative capsulotomy is straight midline longitudinal (see Fig. 89-6).
Procedure
Step 1
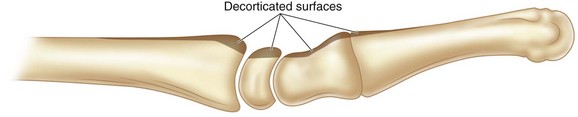
 The dorsal aspect of the radius, carpus, and third carpometacarpal (CMC) joints are decorticated with an osteotome. The dorsal radius, including Lister tubercle, must be contoured by decortication or else it will be difficult to seat the plate on the dorsal radius (Fig. 89-7).
The dorsal aspect of the radius, carpus, and third carpometacarpal (CMC) joints are decorticated with an osteotome. The dorsal radius, including Lister tubercle, must be contoured by decortication or else it will be difficult to seat the plate on the dorsal radius (Fig. 89-7).
 The joints to be fused are prepared by removing articular cartilage and subchondral bone. These include the radioscaphoid, radiolunate, scaphocapitate, lunocapitate, and third CMC joints (Fig. 89-8).
The joints to be fused are prepared by removing articular cartilage and subchondral bone. These include the radioscaphoid, radiolunate, scaphocapitate, lunocapitate, and third CMC joints (Fig. 89-8).
 The ulnar joints (lunotriquetral, triquetrohamate) are not included in the fusion mass.
The ulnar joints (lunotriquetral, triquetrohamate) are not included in the fusion mass.
Step 1 Pearls
Ensure that the joint can be reduced and aligned. Soft tissue releases may be necessary to facilitate alignment of the radius, lunate, capitate, and long finger metacarpal.
In chronic cases with severe carpal deformity (e.g., neglected perilunar fracture-dislocations), excision of the proximal carpal row will facilitate alignment before fusion.
The entire joint height should not be taken down for preparation. This ensures that carpal height will be maintained.
Step 2
 Determine the plate location on the dorsal radius, carpus, and metacarpal, paying particular attention to rotation.
Determine the plate location on the dorsal radius, carpus, and metacarpal, paying particular attention to rotation.
 In some cases, a groove in the distal radial articular surface may need to be created to accept the curved portion of the plate.
In some cases, a groove in the distal radial articular surface may need to be created to accept the curved portion of the plate.
 Harvest bone graft from the distal radius through a cortical window or drill hole adjacent to the plate.
Harvest bone graft from the distal radius through a cortical window or drill hole adjacent to the plate.
Step 2 Pitfalls
Failure to contour the dorsal radius will result in poor adaptation of the plate to the bone and will compromise fixation.
In addition, a prominent plate that does not lie on the bone will be difficult to cover with soft tissue when closing the capsule and retinaculum. Retinacular deficiency may lead to extensor dysfunction.
Step 3
 The prepared articular surfaces are filled with bone graft harvested from the distal radius and from the dorsal decorticated bony surfaces.
The prepared articular surfaces are filled with bone graft harvested from the distal radius and from the dorsal decorticated bony surfaces.
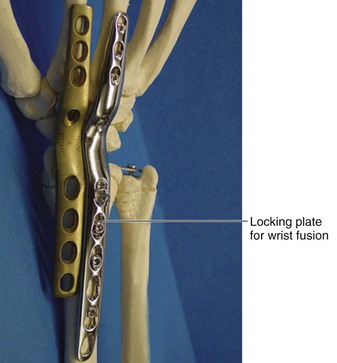
 The plate is applied to the dorsum of the radius, carpus, and long finger metacarpal.
The plate is applied to the dorsum of the radius, carpus, and long finger metacarpal.
 Affix plate to the long finger metacarpal in neutral rotation (Fig. 89-9).
Affix plate to the long finger metacarpal in neutral rotation (Fig. 89-9).
 Affix plate to radius in compression mode (Fig. 89-10).
Affix plate to radius in compression mode (Fig. 89-10).
 Supplement fixation with the oblique carpal screw (Fig. 89-11).
Supplement fixation with the oblique carpal screw (Fig. 89-11).
 Use intraoperative fluoroscopy to assess plate and screw position.
Use intraoperative fluoroscopy to assess plate and screw position.
Step 3 Pearls
Expose enough of the metacarpal so that the plate can be centrally positioned and aligned with the appropriate rotational orientation.
The location of the metacarpal screw can be marked with a marker, and with the plate removed, the orientation of the screw can be assessed.
Locking screw fixation can be used in patients with poor bone stock (Fig. 89-12).
Alternative sources of bone graft are iliac crest, olecranon, proximal tibia, and allograft.
Step 4
 Once the plate is secured, additional bone graft is packed around prepared joints.
Once the plate is secured, additional bone graft is packed around prepared joints.
 The capsular flap can frequently be closed over the plate by advancing the ulnar attachment radially.
The capsular flap can frequently be closed over the plate by advancing the ulnar attachment radially.
 The extensor retinaculum is closed leaving the EPL transposed (Fig. 89-13).
The extensor retinaculum is closed leaving the EPL transposed (Fig. 89-13).
 The skin is closed with nonabsorbable suture or a subcuticular absorbable suture (Fig. 89-14).
The skin is closed with nonabsorbable suture or a subcuticular absorbable suture (Fig. 89-14).
 A bulky dressing to control edema is applied with a splint supporting the wrist.
A bulky dressing to control edema is applied with a splint supporting the wrist.
Step 4 Pearls
The ECRL and ECRB tendons can be released from the metacarpals and incorporated into the capsular closure when soft tissue coverage is deficient or limited.
Alternative coverage of the plate can be achieved using a split extensor retinaculum, placing one flap deep to the extensor tendons over the plate and one flap dorsal to the extensor tendons.
Postoperative Care and Expected Outcomes
 If intraoperative fixation is stable, a removable splint can be fitted 2 weeks after surgery. This splint is worn full-time except for bathing.
If intraoperative fixation is stable, a removable splint can be fitted 2 weeks after surgery. This splint is worn full-time except for bathing.
 If fixation or patient compliance is tenuous, then postoperative cast immobilization is recommended.
If fixation or patient compliance is tenuous, then postoperative cast immobilization is recommended.
 Digital ROM and edema control are emphasized during this timeframe.
Digital ROM and edema control are emphasized during this timeframe.
 A removable splint is worn until 3 months after surgery.
A removable splint is worn until 3 months after surgery.
 Strengthening exercises may begin at 12 weeks after surgery.
Strengthening exercises may begin at 12 weeks after surgery.
 Expected patient outcomes are pain relief, solid fusion, full digital ROM, and full forearm rotation.
Expected patient outcomes are pain relief, solid fusion, full digital ROM, and full forearm rotation.
 Radiographs should show consolidation of prepared articular surfaces with no hardware loosening or lucency (Fig. 89-15).
Radiographs should show consolidation of prepared articular surfaces with no hardware loosening or lucency (Fig. 89-15).
 The patient achieves of about 80% grip strength of the dominant hand.
The patient achieves of about 80% grip strength of the dominant hand.
 The patient is able to complete most activities of daily living (Fig. 89-16).
The patient is able to complete most activities of daily living (Fig. 89-16).
 Perineal care and using the hand and wrist in tight spaces may be limited.
Perineal care and using the hand and wrist in tight spaces may be limited.
Cavaliere CM, Chung KC. Total wrist arthroplasty and total wrist arthrodesis in rheumatoid arthritis: a decision analysis from the hand surgeons’ perspective. J Hand Surg [Am]. 2008;33:1744-1755.
Cavaliere CM, Chung KC. A cost-utility analysis of nonsurgical management, total wrist arthroplasty, and total wrist arthrodesis in rheumatoid arthritis. J Hand Surg [Am]. 2010;35:379-391.
Solem H, Berg NJ, Finsen V. Long term results of arthrodesis of the wrist: a 6-15 year follow up of 35 patients. Scand J Plast Reconstr Surg Hand Surg. 2006;40:175-178.