CHAPTER 89
Mallet Toe
Vasilios A. Lirofonis, DPM; Robert J. Scardina, DPM
Definition
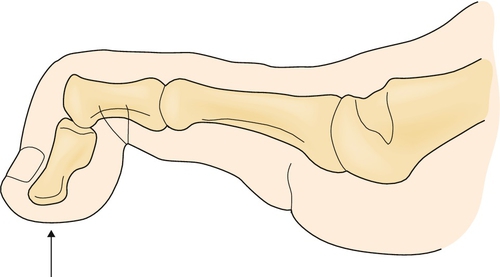
Mallet toe refers to an abnormal flexion deformity at the distal interphalangeal (DIP) joint (Fig. 89.1). Typically, the metatarsophalangeal and proximal interphalangeal joints are aligned in neutral position without extension or flexion. The most commonly affected toe is the longest toe, usually the second. The deformity may be fixed (rigid), semirigid, or flexible; it may occur unilaterally or bilaterally, and it may be acquired or congenital. High-heeled shoes and shoes with a narrow toe box may aggravate the deformity; it is present symptomatically more in women [1,2]. There is some observational evidence to suggest that a toe longer than adjacent toes is at increased risk for development of lesser toe deformities [3]. The incidence of a mallet toe deformity is much less common than that of a hammer toe deformity at almost 1:10 [4]. This is likely to be related to presentation rates as hammer toes are typically more problematic compared with mallet toe deformity.
Symptoms
Patients typically complain of pain or tenderness in the area of the dorsal DIP joint or distal aspect of the toe, most commonly when wearing shoes, particularly with a narrow toe box. The symptoms are also worse during weight-bearing activities, such as running. Patients may also have complaints of toenail deformities, which eventually may become painful. A painful corn or clavus may develop on either the dorsal aspect of the DIP joint (as a result of shoe irritation) or the distal aspect of the toe.
Physical Examination
The degree of DIP joint flexion should be evaluated, both weight bearing and non–weight bearing. Passive range of motion should be determined to evaluate whether the deformity is flexible, rigid, or semirigid, which will influence treatment options. One should inspect for cutaneous lesions (corns) on both the dorsal and distal aspects of the toe. Corns may progress to ulcers with subsequent superficial or deep infection, especially in the diabetic population with neuropathy. If the patient has peripheral arterial disease, ulceration may lead to necrosis and possible toe loss.
Swelling, increased temperature, or erythema might indicate inflammatory arthritis or joint infection. The patient’s footwear should be examined to determine sufficient or insufficient toe box height to accommodate the deformity. Traditional neurologic and vascular examinations generally reveal no abnormal findings in uncomplicated mallet toe conditions.
Functional Limitations
Functional limitation in ambulation occurs most often as the result of pain, particularly with wearing of closed shoes and with weight-bearing activities. Walking may be limited, and high-impact activities such as running may be altogether too painful. Women may complain that they are unable to wear shoes (dress and high heeled) required for their work environment. Painless deformity generally neither causes functional limitations nor requires treatment [5].
Diagnostic Studies
The diagnosis of a mallet toe is primarily clinical. However, foot radiographs can be useful in assessing the DIP joint with fixed deformity resulting from traumatic, degenerative, or inflammatory arthritis. Weight-bearing views are preferred in assessing for functional or dynamic (versus fixed) deformity. Non–weight-bearing isolated or magnification toe views also may be helpful. Noninvasive arterial studies (toe-brachial index) are used to assess perfusion in cases in which ischemia is suspected before initiation of conservative and especially surgical treatment.
Treatment
Initial
Patient education to provide an understanding of the deformity and proper footwear are essential. Shoes fabricated with soft upper material and having (or modified to achieve) adequate toe box depth to accommodate the deformity should be recommended (e.g., extra-depth shoes). Shoes incompatible with the deformity, especially high heels, should be avoided as much as possible. A soft shoe insole may be helpful in relieving pressure at the distal aspect of the toe [7,8]. Moleskin or adhesive felt padding may be applied to painful corns, but the use of medicated (salicylic acid) plasters should be avoided, especially in patients with diabetes or peripheral vascular disease. Oral nonsteroidal anti-inflammatory drugs and analgesics can help reduce pain but should be used only as a short-term measure. Initial care should be palliative and not directed toward deformity correction. Orthodigital devices (custom, premade, or hand fashioned), such as crest pads or mallet toe regulators, may relieve pressure over the involved joint or distal aspect of the toe, resulting in passive realignment of flexible deformities. Painful corns may be treated with digital cps, sleeves, or silicone cushions. Superficial ulcers developing from a corn or clavus are treated with off-loading measures and local wound care. Patients with “high-risk” neuropathic or dysvascular feet should be educated to perform diligent daily inspection for skin breakdown.
Rehabilitation
Formal physical therapy is usually not required unless the toe deformity is accompanied by more global foot deformity due to a neuromuscular disorder. Although toe and foot flexor tendon stretching exercises are generally of little or no benefit, they may relieve the “tight” sensation in patients with a flexible or semirigid deformity. Functional foot orthoses can provide flexor tendon stabilization and, in some instances, symptomatic relief in patients with subtalar joint hyperpronation and flexible mallet toe deformity. In occasional cases, when extra-depth shoes provide insufficient toe box room to accommodate the deformity, custom shoes may be prescribed. Physical therapy after surgical correction is usually indicated for reduction of edema.
Procedures
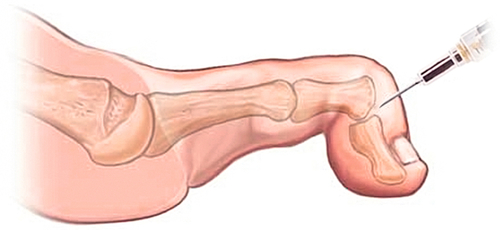
Steroid injections may be indicated for patients with a painful mallet toe deformity in the presence of inflammatory joint disease (Fig. 89.2). An intra-articular injection of a soluble corticosteroid with local anesthetic mixture, performed in sterile technique with a 27- or 30-gauge needle, may provide temporary relief. The patient should be advised about the possibility of a postinjection flare.
Surgery
Operative treatment should be considered when conservative treatments fail, painful cutaneous lesions persist, and especially if ulceration or infection develops. Cosmesis alone is a poor indication for surgical correction. Surgical treatment depends on the etiology, extent, and severity of the deformity. Contributory or associated digital or forefoot deformities (e.g., hallux valgus, hammer toe, neighboring underriding or overlapping toe deformities) may also require correction for optimal surgical outcome, including surgery for proximal interphalangeal joint flexion or metatarsophalangeal joint deformity of the same toe. For mild, flexible, manually reducible deformity, soft tissue procedures, such as long flexor tenotomy with or without plantar DIP joint capsulotomy, are indicated. For more severe and rigid deformity, DIP joint osseous and articular procedures (e.g., resection arthroplasty, arthrodesis, extension block method [9]) are required. Lesser toe mallet deformity does not absolutely require fusion [10]. Severe deformity, with the presence or threat of ulceration, may require partial digital amputation [11–13]. Cases involving osteomyelitis of the distal phalanx almost always require amputation at some level of the toe. In severe deformities, retrospective studies have shown that DIP joint resection arthroplasty combined with flexor tenotomy increases the likelihood of a good outcome [11,13]. Digital interphalangeal joint arthrodesis procedures may be performed in end-to-end or peg-in-hole fashion. The peg-in-hole technique has the advantage of shortening, which can reduce long flexor tendon tension. Temporary percutaneous 0.045-inch K-wire fixation of an end-to-end arthrodesis may result in better outcome.
Potential Disease Complications
Potential disease complications include mobility-limiting, chronic, intractable pain; metatarsalgia; dorsal or distal hyperkeratotic lesions or ulcerations, most commonly in the insensate foot; joint pain and stiffness; toenail deformities; bursitis; and synovitis. Gait abnormalities (antalgic) may contribute to more proximal pain of the low back, hip, and knee. A potential complication of nonsurgical treatment is deviation of the toes, especially overlapping second toes.
Potential Treatment Complications
Analgesics and nonsteroidal anti-inflammatory drugs have well-known side effects that most commonly affect the gastric, hepatic, and renal systems. Potential complications after corticosteroid injections include skin hypopigmentation at the injection site, infection, transient elevated blood glucose concentration, and postinjection flare (pain). Postsurgical complications include toe ischemia, digital nerve palsy, arthrodesis nonunion, joint malalignment, rigid or excessively straight toe, flail DIP joint, persistent or chronic toe edema, infection, flail toe, and periarticular osseous proliferation.







