CHAPTER 88
Hammer Toe
Definition
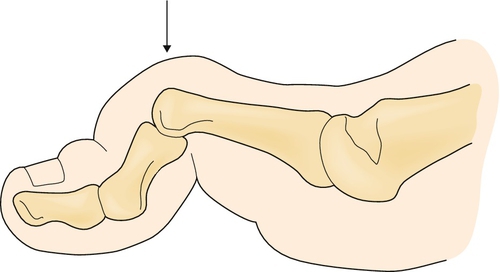
Hammer toe refers to an abnormal flexion posture at the proximal interphalangeal (PIP) joint of one or more of the lesser four toes [1]. If the flexion contracture is severe and of long duration, concomitant hyperextension of the metatarsophalangeal (MTP) joint and extension of the distal interphalangeal (DIP) joint may occur (Fig. 88.1). In contrast to clawing, which tends to involve all toes, hammer toe deformity usually affects only one or two toes [2]. Hammer toes are classified as either flexible (passively correctable) or rigid (not passively correctable to the neutral position). The most commonly affected toe is the second, although multiple digits can be involved [3].
Hammer toe is the most common of the lesser toe deformities and occurs primarily in the sagittal plane. It is arguably the most common toe disorder that presents to the foot and ankle surgeon’s office. Women are more commonly affected, and the incidence of hammer toe increases with age [4–6].
Contributing factors include long-term wear of poorly fitting shoes, especially those with tight, narrow toe boxes. Crowding and overlapping from hallux valgus are other causes. A long second ray with subsequent buckling of the toe may also lead to the deformity. Other predisposing factors are diabetes, connective tissue disease, and trauma [5].
Symptoms
Patients commonly complain of pain or tenderness in the area of the PIP joint, especially when wearing shoes or during weight-bearing activities. Patients also commonly present with cosmetic complaints. Pain may be the result of corn or callus formation over the dorsal aspect of the PIP joint from shoe compression. In cases in which hyperextension of the MTP joint has occurred, there is also increased pressure under the metatarsal heads. Metatarsalgia with subsequent callus formation underneath the metatarsal heads may occur secondary to their plantar displacement [2], with distal displacement of the plantar fat pad.
Physical Examination
The diagnosis is confirmed by the presence of MTP joint hyperextension, PIP joint flexion, and DIP joint extension in the affected toe. Palpation of the PIP joint usually causes tenderness, with the plantar aspect more commonly affected.
On inspection, determine the degree of PIP flexion. Also note accompanying foot deformities, such as ulcerations and callus formation over the PIP joint and tip of the toe. Hammer toe deformities become more prominent in stance phase. Examination of the joint range of motion of the affected toe will differentiate a fixed deformity from the one that is flexible. The presence or absence of crepitus should be noted. Flexor digitorum longus contracture is assessed with the ankle in dorsiflexion and plantar flexion. Correction of the deformity on plantar flexion signifies a flexible hammer toe. Dorsiflexion, in turn, accentuates the deformity [7].
The Kelikian push-up test is used to assess the degree of flexibility. Press upward on the plantar aspect of the metatarsal head; in flexible deformities, the MTP joint will align and the proximal phalanx will assume a more normal position.
A mild deformity hammer toe implies no fixed contracture at the MTP or PIP joint, but the deformity increases with weight bearing. A moderate deformity hammer toe has a fixed or partially fixed contracture at the PIP joint and zero to mild extension contracture at the MTP joint. A severe deformity hammer toe involves fixed flexion contracture at the PIP joint with a fixed extension contracture of the MTP joint. Subluxation or dislocation of the proximal phalanx on the metatarsal head may also be present [7].
Also assess for signs of swelling, temperature change, or erythema that might indicate the presence of an infectious or rheumatic process responsible for the deformity.
Inspection of the patient’s footwear is necessary to determine the ability of the toe box to accommodate the forefoot. The presence of corns or callus over the PIP joint, which may ulcerate, is often indicative of poorly fitting footwear.
Standard neurologic and vascular examinations will reveal no abnormal findings in uncomplicated hammer toe deformities. If there is a superficial peroneal nerve injury causing a dropfoot deformity, hammer toes will result because of extensor substitution. Likewise, a weakness of the gastrocnemius can lead to flexor substitution, causing a hammer toe.
If the patient has peripheral vascular disease or atherosclerosis, ulceration over a PIP joint may lead to toe loss unless the toe is revascularized.
Functional Limitations
Functional limitations mostly result from pain incurred by corn and callus formation. Walking and other weight-bearing activities can be painful. The ability to tolerate footwear with a narrow toe box is also impaired.
Diagnostic Studies
The diagnosis is primarily a clinical one. However, radiographs can be useful in the assessment of a rigid hammer toe, with weight-bearing views preferred. An apparent joint space narrowing on the anteroposterior view corresponds to subluxation of the proximal phalanx on the metatarsal head at the MTP joint [5,7].
Treatment
Initial
Patient education is critical. The first step involves fitting for shoes with an adequate toe box to accommodate the dorsiflexed position of the proximal phalanx. High heels should be avoided as much as possible. A soft insole can also be used, which is useful for pressure relief [8]. Oral or topical nonsteroidal anti-inflammatory drugs (NSAIDs) can help with pain and inflammation. Analgesic medications may be taken for pain relief. Ulcer and callus management may be necessary, and patients should be educated about monitoring their skin for breakdown, especially in the setting of peripheral neuropathy.
Local icing may also help with acute pain (10 minutes, two or three times a day). However, ice should be avoided in patients with significant peripheral vascular disease because of its vasoconstrictive properties and in individuals with impaired sensation, such as peripheral neuropathy, because of the risk of frostbite.
Initial treatment is palliative rather than corrective and predominantly consists of attempts to accommodate the toe deformity by changing the patient’s footwear and débridement of calluses if they are present. This may include stretching the shoes or switching to shoes with a deeper toe box or to extra-depth shoes. Padding, such as toe crest pads or custom or premade hammer toe regulators, may relieve pressure over the involved joints. Patients with calluses on the PIP joint may benefit from digital caps or silicone cushions.
Rehabilitation
Formal physical therapy is usually not required, although some patients might benefit from a supervised paraffin treatment, which should be followed by stretching exercises. Paraffin baths are contraindicated if ulcers or sensory deficits are present [9].
Stretching exercises can relieve the “tight” sensation in patients with a flexible or semiflexible deformity. Exercises such as picking up a towel with the toes are recommended for both stretching and strengthening of the intrinsic foot muscles.
Functional orthotics will provide flexor stabilization and, in some instances, symptomatic relief to overpronators with a flexible hammer toe deformity. Orthotics may slow the progression of the deformity by improving the biomechanics of the feet.
The clinician may prescribe shoes with deep, wide toe boxes. Alternatively, extra depth can be achieved in a standard shoe by trimming the existing shoe insert just distal to the metatarsal heads [10]. Lambswool or felt around the toes provides extra padding. An external metatarsal bar and rocker-bottom shoes may provide additional comfort-enhancing options. Specific strapping devices and hammer toe straightening orthoses are available. Again, patients with peripheral vascular disease or neuropathy should be cautious or avoid these.
Procedures
Steroid injections may be indicated for patients with painful PIP joint capsulitis or arthritic flare secondary to a hammer toe deformity. Combine steroid injections with padding or splinting for optimal relief. By use of a 27-gauge needle and corticosteroid with local anesthetic mixture, introduce the solution into the joint capsule through the dorsomedial or dorsolateral aspect of the joint. Always perform a surgical preparation before injecting the joint. The patient should be advised about the possibility of a steroid flare.
Surgery
Operative treatment should be pursued when conservative treatment fails. Cosmesis alone is not a good indication for surgery. Associated deformities must also be corrected for optimal surgical outcome (e.g., hallux valgus) [7].
Multiple procedures have been described for the surgical management of hammer toes. The procedures used are based on the degree of hammer toe deformity. A stepwise approach involving several procedures may be needed to accomplish correction on the basis of severity. Outcomes are varied by the specific procedures chosen. The following procedures are most commonly recommended and data supported [2]:
Moderate deformity/rigid hammer toe with MTP subluxation (fixed flexion contracture at the PIP; MTP subluxation in extension): resection of the condyles of the proximal phalanx, dermodesis (removal of an ellipse of skin on the volar aspect of the joint); lengthening of extensor digitorum longus, tenotomy of extensor digitorum brevis; MTP capsulotomy, collateral ligament sectioning.
Moderate to severe deformity/rigid hammer toe with MTP dislocation: similar to subluxation treatment with addition of MTP arthroplasty or Weil osteotomy.
Severe deformity/crossover toe (fixed flexion contracture at the PIP joint; MTP subluxation in varus or valgus): resection of the condyles of the proximal phalanx, dermodesis; collateral ligament/capsular repair; extensor digitorum brevis transfer [2,11].
Replacement of the PIP or MTP joint with toe deformity is another option, as are implants that have been developed for intramedullary placement to stabilize the PIP joint, promoting fusion. Such implants are not universally accepted and are exceedingly difficult to remove should the surgery fail. Their removal could lead to substantial bone loss, making subsequent revision procedures challenging. Kirschner wires are usually used to stabilize the hammer toes for several weeks and are most accepted at this time.
Postoperative Rehabilitation
After 2 or 3 days of elevation of the foot, patients can bear weight as tolerated. Surgical shoes with limited activity and use of crutches are recommended for approximately 4 weeks postoperatively. If Kirschner wires are used, they are typically removed between 3 and 6 weeks after operation. This varies by the surgeon’s preference [12]. Patients can start to gradually increase activities at approximately 8 weeks after surgery. More weight-bearing activities, such as running, are best started after 12 weeks of recovery. Such recommendations vary according to the severity of the deformity and complexity of the surgery.
Potential Disease Complications
Potential disease complications include chronic intractable pain that limits all mobility. Other complications may include metatarsalgia, plantar and point of contact ulcerations in the insensate foot, arthralgia and joint stiffness if subluxation has occurred, toenail deformities, and bursitis or synovitis [5]. Gait abnormalities may contribute to more proximal pain symptoms (e.g., low back and hip pain).
Diabetic neuropathy and advanced peripheral vascular disease are relative contraindications to splinting [13] when correction is nonsurgical.
Common potential complications include PIP joint ulceration due to excessive pressure, fixed foot deformity, and postural changes resulting from pain-induced gait deviations.
Potential Treatment Complications
Local icing can cause vasoconstriction and frostbite. Analgesics, NSAIDs, and cyclooxygenase 2 inhibitors have well-known side effects that most commonly affect the gastric, hepatic, and renal systems. Newer topical NSAIDs may have fewer side effects because of less systemic absorption. Postsurgical complications include toe ischemia, digital nerve palsy, nonunion, malalignment, reduced toe range of motion, rigid and excessively straight toe, persistent edema, flail toe, and osseous regrowth. Potential complications of surgical correction include flail or “floppy” toes, which can be repaired by collateral ligament repair or arthrodesis. Infection and, in severe cases, osteomyelitis can occur either before or as a complication of surgery. If intravenous antibiotic treatment is unsuccessful, partial or total toe amputation may be required. Because of the morbidity associated with surgical complications, appropriate patient selection is imperative in recommending operative correction of hammer toe deformities.







