Procedure 87 Four-Corner Fusion
![]() See Video 65: 4-Corner Fusion Using Kirschner Wires
See Video 65: 4-Corner Fusion Using Kirschner Wires
Examination/Imaging
Imaging
 Plain radiographs are usually sufficient for diagnosis. SLAC wrist, stage 3, demonstrates abnormal position of the scaphoid, scapholunate widening, radioscaphoid degenerative change and midcarpal arthrosis (Fig. 87-1).
Plain radiographs are usually sufficient for diagnosis. SLAC wrist, stage 3, demonstrates abnormal position of the scaphoid, scapholunate widening, radioscaphoid degenerative change and midcarpal arthrosis (Fig. 87-1).
 In cases in which there is uncertainty about the status of the radiolunate joint, advanced imaging (computed tomography) may be used.
In cases in which there is uncertainty about the status of the radiolunate joint, advanced imaging (computed tomography) may be used.
Surgical Anatomy
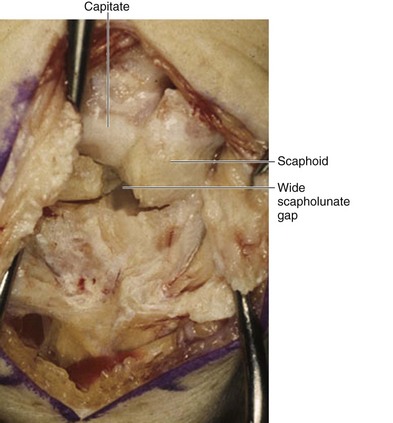
 In either SLAC or SNAC, there will be widening at the scapholunate interval.
In either SLAC or SNAC, there will be widening at the scapholunate interval.
 Significant scaphoid flexion, lunate extension, and dorsal lunate prominence develop.
Significant scaphoid flexion, lunate extension, and dorsal lunate prominence develop.
 Radioscaphoid degenerative change with styloid prominence and osteophytes is noted.
Radioscaphoid degenerative change with styloid prominence and osteophytes is noted.
 Proximal scaphoid pole necrosis and/or arthrosis is present (Fig. 87-2).
Proximal scaphoid pole necrosis and/or arthrosis is present (Fig. 87-2).
 Scaphotrapeziotrapezoid arthrosis may be present.
Scaphotrapeziotrapezoid arthrosis may be present.
 The dorsal ligaments of the wrist—dorsal radiocarpal (DRC) and dorsal intercarpal (DIC)—have a conjoined insertion on the triquetrum. They provide the capsulotomy landmarks for wrist exposure.
The dorsal ligaments of the wrist—dorsal radiocarpal (DRC) and dorsal intercarpal (DIC)—have a conjoined insertion on the triquetrum. They provide the capsulotomy landmarks for wrist exposure.
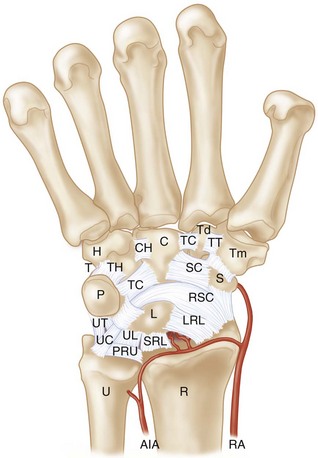
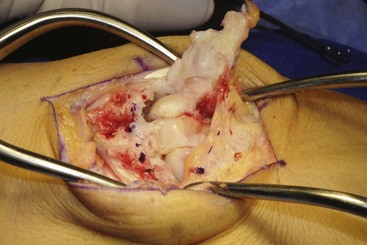
 The volar extrinsic ligaments (radioscaphocapitate, short and long radiolunate) originate from the volar radius and extend obliquely to the carpus. These should be respected during scaphoid excision (Fig. 87-3).
The volar extrinsic ligaments (radioscaphocapitate, short and long radiolunate) originate from the volar radius and extend obliquely to the carpus. These should be respected during scaphoid excision (Fig. 87-3).
Exposures
 A dorsal midline incision centered over the radiocarpal joint is used.
A dorsal midline incision centered over the radiocarpal joint is used.
 Thick flaps are elevated dorsal to the retinaculum, keeping cutaneous nerves within these flaps.
Thick flaps are elevated dorsal to the retinaculum, keeping cutaneous nerves within these flaps.
 The retinaculum over the third dorsal compartment is incised.
The retinaculum over the third dorsal compartment is incised.
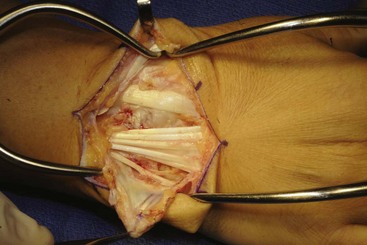
 Retinacular flaps are raised, exposing the second through fifth compartments (Fig. 87-4).
Retinacular flaps are raised, exposing the second through fifth compartments (Fig. 87-4).
 The extensor tendons are retracted using retractors placed between the second and fourth compartments.
The extensor tendons are retracted using retractors placed between the second and fourth compartments.
 A posterior interosseous neurectomy is performed.
A posterior interosseous neurectomy is performed.
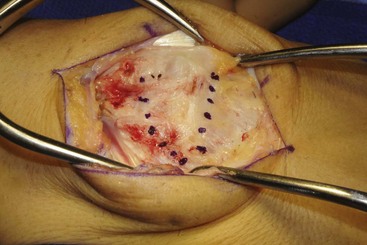
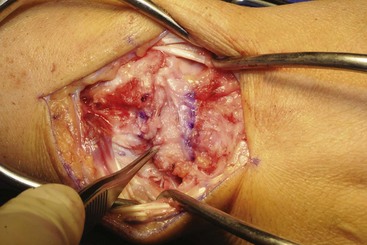
 A capsulotomy is performed by dividing the dorsal capsule along the dorsal intercarpal and dorsal radiocarpal ligaments (Fig. 87-5). The flap is elevated off the dorsum of the triquetrum and reflected, keeping it radially based (Fig. 87-6).
A capsulotomy is performed by dividing the dorsal capsule along the dorsal intercarpal and dorsal radiocarpal ligaments (Fig. 87-5). The flap is elevated off the dorsum of the triquetrum and reflected, keeping it radially based (Fig. 87-6).
Procedure
Step 1
 Inspection of the radiolunate joint is performed to ensure that it is free of degenerative change.
Inspection of the radiolunate joint is performed to ensure that it is free of degenerative change.
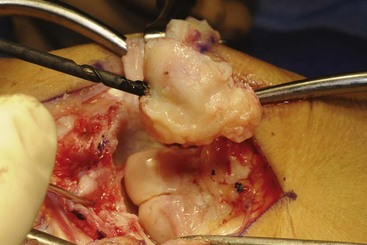
 A threaded gimlet, Schanz screw, or Steinman pin is used as a joystick to facilitate removal of the scaphoid (Fig. 87-7).
A threaded gimlet, Schanz screw, or Steinman pin is used as a joystick to facilitate removal of the scaphoid (Fig. 87-7).
Step 2
Step 3
 A 0.062-inch Kirschner wire is placed in the dorsal lunate as a joystick. The lunate is usually in an abnormally extended position, and it must be reduced to a colinear relationship with the capitate (Fig. 87-10). Soft tissue release may be necessary to achieve this relationship.
A 0.062-inch Kirschner wire is placed in the dorsal lunate as a joystick. The lunate is usually in an abnormally extended position, and it must be reduced to a colinear relationship with the capitate (Fig. 87-10). Soft tissue release may be necessary to achieve this relationship.
 After confirming that reduction is possible, the midcarpal joint is exposed, and the cartilage and subchondral bone of the distal lunate and capitate are removed.
After confirming that reduction is possible, the midcarpal joint is exposed, and the cartilage and subchondral bone of the distal lunate and capitate are removed.
 Bone graft is placed, and the lunate is reduced.
Bone graft is placed, and the lunate is reduced.
 Provisional K-wire fixation holds the lunate, and the capitate is reduced (Fig. 87-11).
Provisional K-wire fixation holds the lunate, and the capitate is reduced (Fig. 87-11).
Step 3 Pearls
Occasionally a large dorsal lunate osteophyte is present and may be removed to facilitate visualization of the midcarpal joint.
When correctly reduced, the capitate appears to overhang the radial margin of the lunate.
Colinearity of the lunate to the capitate, or even slight lunate flexion, is desirable.
Step 4
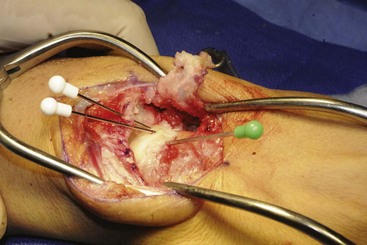
 The lunotriquetral, triquetrohamate, and capitohamate intervals are prepared by removing cartilage and subchondral bone.
The lunotriquetral, triquetrohamate, and capitohamate intervals are prepared by removing cartilage and subchondral bone.
 Graft is placed in these intervals.
Graft is placed in these intervals.
 Provisional fixation from the triquetrum to the capitate is performed.
Provisional fixation from the triquetrum to the capitate is performed.
Step 5
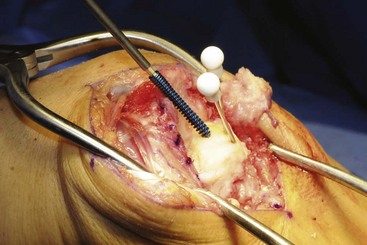
 The radiocarpal joint is flexed, and a guidewire for a cannulated screw is placed down the central lunate-capitate axis.
The radiocarpal joint is flexed, and a guidewire for a cannulated screw is placed down the central lunate-capitate axis.
 A cannulated screw is placed compressing the midcarpal joint.
A cannulated screw is placed compressing the midcarpal joint.
 A second screw is placed obliquely to the first screw, usually from the triquetrum into the capitate (Fig. 87-12).
A second screw is placed obliquely to the first screw, usually from the triquetrum into the capitate (Fig. 87-12).
Additional Steps
 An additional graft is placed to fill the prepared interfaces (Fig. 87-14).
An additional graft is placed to fill the prepared interfaces (Fig. 87-14).
 The capsule is closed anatomically with nonabsorbable suture (Fig. 87-15).
The capsule is closed anatomically with nonabsorbable suture (Fig. 87-15).
 The retinaculum is closed leaving the extensor pollicis longus (EPL) transposed.
The retinaculum is closed leaving the extensor pollicis longus (EPL) transposed.
 The skin is closed with nonabsorbable suture.
The skin is closed with nonabsorbable suture.
 A bulky compressive dressing is applied to allow digital range of motion and to help control edema (Fig. 87-16).
A bulky compressive dressing is applied to allow digital range of motion and to help control edema (Fig. 87-16).
Postoperative Care and Expected Outcomes
 The postoperative dressing is maintained for 2 weeks.
The postoperative dressing is maintained for 2 weeks.
 The wrist is then immobilized in a removable custom-molded splint that is worn full time except for bathing.
The wrist is then immobilized in a removable custom-molded splint that is worn full time except for bathing.
 Range-of-motion exercises can commence 6 to 8 weeks after surgery.
Range-of-motion exercises can commence 6 to 8 weeks after surgery.
 Strengthening exercises begin at 12 weeks.
Strengthening exercises begin at 12 weeks.
 Patients can expect to lose about 50% of their preoperative range of motion with a total arc of motion of about 60 to 90 degrees.
Patients can expect to lose about 50% of their preoperative range of motion with a total arc of motion of about 60 to 90 degrees.
Bain GI, Watts AC. The outcome of scaphoid excision and four-corner arthrodesis for advanced carpal collapse at a minimum of ten years. J Hand Surg [Am]. 2010;35:719-725.
Cohen MS, Kozin SH. Degenerative arthritis of the wrist: proximal row carpectomy versus scaphoid excision and four-corner arthrodesis. J Hand Surg [Am]. 2001;26:94-104.
Dacho AK, Baumeister S, Germann G, et al. Comparison of proximal row carpectomy and midcarpal arthrodesis for the treatment of scaphoid nonunion advanced collapse (SNAC-wrist) and scapholunate advanced collapse (SLAC-wrist) in stage II. J Plast Reconstr Aesthet Surg. 2008;61:1210-1218.
Vance MC, Hernandez JD, Didonna ML, et al. Complications and outcome of four-corner arthrodesis: circular plate fixation versus traditional techniques. J Hand Surg [Am]. 2005;30:1122-1127.