Procedure 86 Proximal Row Carpectomy
![]() See Video 64: Proximal Row Carpectomy
See Video 64: Proximal Row Carpectomy
Indications
Examination/Imaging
Imaging
 Plain radiographs are usually sufficient to stage the disease and ensure that the midcarpal joint is preserved (Figs. 86-1 and 86-2).
Plain radiographs are usually sufficient to stage the disease and ensure that the midcarpal joint is preserved (Figs. 86-1 and 86-2).
 Advanced imaging (computed tomography) can be performed to determine the status of the midcarpal joint; however, patients are made aware preoperatively that an intraoperative decision to convert to a limited wrist fusion can be made if there is excessive, unrecognized midcarpal joint degenerative change.
Advanced imaging (computed tomography) can be performed to determine the status of the midcarpal joint; however, patients are made aware preoperatively that an intraoperative decision to convert to a limited wrist fusion can be made if there is excessive, unrecognized midcarpal joint degenerative change.
Surgical Anatomy
 In either SLAC or SNAC, there will be widening at the scapholunate interval.
In either SLAC or SNAC, there will be widening at the scapholunate interval.
 Significant scaphoid flexion, lunate extension, and dorsal lunate prominence develop.
Significant scaphoid flexion, lunate extension, and dorsal lunate prominence develop.
 Radioscaphoid degenerative change with styloid prominence or osteophytes.
Radioscaphoid degenerative change with styloid prominence or osteophytes.
 Proximal scaphoid pole necrosis and/or arthrosis.
Proximal scaphoid pole necrosis and/or arthrosis.
 Scaphotrapeziotrapezoid arthrosis may be present.
Scaphotrapeziotrapezoid arthrosis may be present.
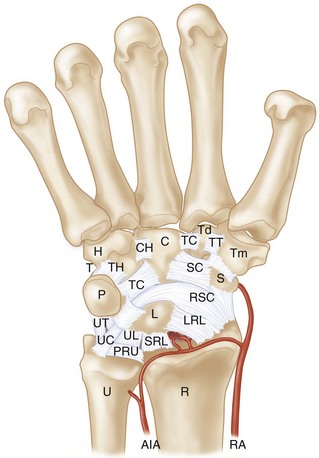
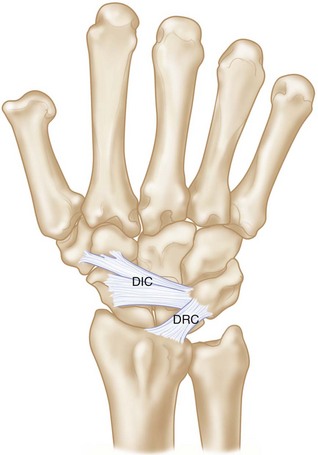
 The volar extrinsic ligaments (radioscaphocapitate, short and long radiolunate) originate from the volar radius and extend obliquely to the carpus. These should be intact; insufficiency or iatrogenic damage could lead to ulnar translation and radiocapitate instability after surgery (Fig. 86-3). The dorsal ligaments of the wrist—dorsal radiocarpal (DRC) and dorsal intercarpal (DIC)—have a conjoined insertion on the triquetrum. They provide the capsulotomy landmarks for wrist exposure (Fig. 86-4).
The volar extrinsic ligaments (radioscaphocapitate, short and long radiolunate) originate from the volar radius and extend obliquely to the carpus. These should be intact; insufficiency or iatrogenic damage could lead to ulnar translation and radiocapitate instability after surgery (Fig. 86-3). The dorsal ligaments of the wrist—dorsal radiocarpal (DRC) and dorsal intercarpal (DIC)—have a conjoined insertion on the triquetrum. They provide the capsulotomy landmarks for wrist exposure (Fig. 86-4).
Exposures
 A straight dorsal midline incision centered over the radiocarpal joint is used (Fig. 86-5).
A straight dorsal midline incision centered over the radiocarpal joint is used (Fig. 86-5).
 Flap elevation is performed sharply, protecting the cutaneous branches of the superficial radial and dorsal ulnar sensory nerves within the subcutaneous tissue.
Flap elevation is performed sharply, protecting the cutaneous branches of the superficial radial and dorsal ulnar sensory nerves within the subcutaneous tissue.
 The retinaculum over the third dorsal compartment is incised and the extensor pollicis longus (EPL) retracted (Fig. 86-6).
The retinaculum over the third dorsal compartment is incised and the extensor pollicis longus (EPL) retracted (Fig. 86-6).
 Retinacular flaps are raised exposing the second through fifth dorsal compartments.
Retinacular flaps are raised exposing the second through fifth dorsal compartments.
 Retractors are placed between the second and fourth dorsal compartment tendons.
Retractors are placed between the second and fourth dorsal compartment tendons.
 A posterior interosseous neurectomy is performed. The PIN is located on the floor of the fourth dorsal compartment
A posterior interosseous neurectomy is performed. The PIN is located on the floor of the fourth dorsal compartment
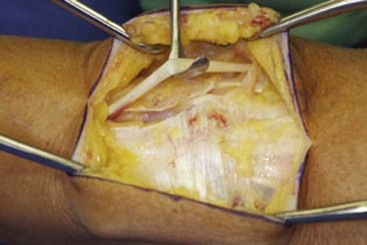
 The capsule is incised along the DIC and DRC ligaments raising a radially based flap (Fig. 86-7).
The capsule is incised along the DIC and DRC ligaments raising a radially based flap (Fig. 86-7).
 If a soft tissue interposition using the capsule is planned, a proximally based, rectangular flap of capsule is harvested instead of using the capsular exposure previously described. The soft tissue interposition procedure is used if there is some articular wear on the capitate.
If a soft tissue interposition using the capsule is planned, a proximally based, rectangular flap of capsule is harvested instead of using the capsular exposure previously described. The soft tissue interposition procedure is used if there is some articular wear on the capitate.
Pearls
The dorsal capsular ligaments are more prominent with the wrist in flexion. Placing a “bump” under the wrist facilitates visualization. Fatty perivascular tissue is sometimes prominent on the dorsal capsule. Bluntly dissecting it off the capsule with a sponge also facilitates visualization of the ligaments.
Leave a cuff of ligament along the radial rim for closure, but incise the ligament close enough to the radius to visualize the proximal carpal row.
Procedure
Step 1
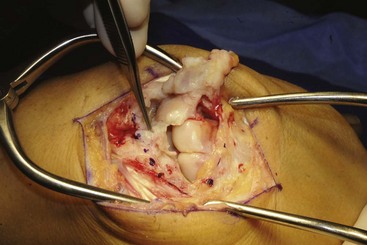
 Inspection of the distal radius and midcarpal joint is performed. Ensure that the lunate fossa and proximal capitate are intact. Alternative procedures should be considered if there is damage to the midcarpal or radiolunate articulations (Fig. 86-8).
Inspection of the distal radius and midcarpal joint is performed. Ensure that the lunate fossa and proximal capitate are intact. Alternative procedures should be considered if there is damage to the midcarpal or radiolunate articulations (Fig. 86-8).
Step 1 Pearls
Mild degenerative change at the capitate head or radiolunate joint can be treated with proximal row carpectomy (PRC) and concomitant capsular interposition.
Osteochondral resurfacing has also been described as an adjunctive procedure with PRC for capitate chondrosis. An osteochondral graft is obtained from the excised carpus, usually the lunate, and inserted into the defect created after excising the area of cartilage loss (limited to a single area <10 mm in diameter).
Step 2
 The lunotriquetral ligament is divided, and the lunate is excised in its entirety by carefully dissecting it off the volar ligament. This technique minimizes the chance of bone attached to the capsule being left behind.
The lunotriquetral ligament is divided, and the lunate is excised in its entirety by carefully dissecting it off the volar ligament. This technique minimizes the chance of bone attached to the capsule being left behind.
 Avoid injuring the cartilage surface of the radiolunate joint or capitate head.
Avoid injuring the cartilage surface of the radiolunate joint or capitate head.
Step 2 Pearls
A joystick can be placed in the lunate to facilitate manipulation.
Care is taken to avoid injury to the volar ligaments and cartilage of the distal radius and capitate.
It is easier to completely remove the bone using careful circumferential subperiosteal dissection rather than a piecemeal technique with a rongeur.
Step 4
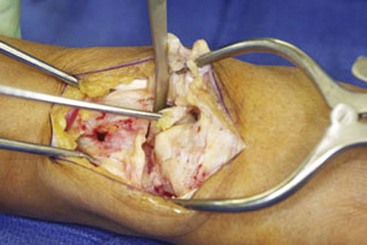
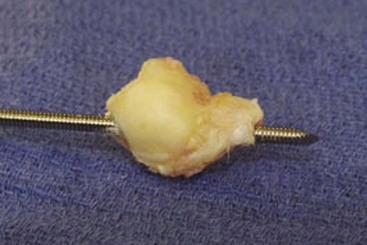
 After removal of the lunate and triquetrum, a joystick should be placed in the scaphoid (Fig. 86-9). Threaded Steinmann pins, Schanz screws, or threaded gimlets can be used. Avoid temptation for piecemeal excision using a rongeur because it is easier to remove the entire scaphoid using careful and deliberate subperiosteal dissection methods (Fig. 86-10).
After removal of the lunate and triquetrum, a joystick should be placed in the scaphoid (Fig. 86-9). Threaded Steinmann pins, Schanz screws, or threaded gimlets can be used. Avoid temptation for piecemeal excision using a rongeur because it is easier to remove the entire scaphoid using careful and deliberate subperiosteal dissection methods (Fig. 86-10).
Step 5
Additional Steps
 Anatomic capsular closure using nonabsorbable suture is performed.
Anatomic capsular closure using nonabsorbable suture is performed.
 The extensor retinaculum is closed, leaving the EPL transposed (Fig. 86-12).
The extensor retinaculum is closed, leaving the EPL transposed (Fig. 86-12).
 Skin is closed with interrupted nonabsorbable suture.
Skin is closed with interrupted nonabsorbable suture.
 A well-padded dressing is applied to control edema yet allow digital range of motion.
A well-padded dressing is applied to control edema yet allow digital range of motion.
 A radiograph is taken to ensure that the capitate is reduced on the radius (Figs. 86-13 and 86-14).
A radiograph is taken to ensure that the capitate is reduced on the radius (Figs. 86-13 and 86-14).
Postoperative Care and Expected Outcomes
 Dressing and suture are removed 2 weeks after surgery.
Dressing and suture are removed 2 weeks after surgery.
 A short-arm cast is worn until 6 weeks after surgery.
A short-arm cast is worn until 6 weeks after surgery.
 A removable splint is applied and range of motion initiated 6 weeks after surgery.
A removable splint is applied and range of motion initiated 6 weeks after surgery.
 Strengthening exercises can begin at 10 to 12 weeks.
Strengthening exercises can begin at 10 to 12 weeks.
 Expect 70 degrees of arc of motion and recovery of 70% of grip strength.
Expect 70 degrees of arc of motion and recovery of 70% of grip strength.
Cohen MS, Kozin SH. Degenerative arthritis of the wrist: proximal row carpectomy versus scaphoid excision and four-corner arthrodesis. J Hand Surg [Am]. 2001;26:94-104.
Croog AS, Stern PJ. Proximal row carpectomy for advanced Kienböck’s disease: average 10-year follow-up. J Hand Surg [Am]. 2008;33:1122-1130.
DiDonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: study with a minimum of ten years of follow-up. J Bone Joint Surg [Am]. 2004;86:2359-2365.
Lumsden BC, Stone A, Engber WD. Treatment of advanced-stage Kienböck’s disease with proximal row carpectomy: an average 15-year follow-up. J Hand Surg [Am]. 2008;33:493-502.
Tang P, Imbriglia JE. Osteochondral resurfacing (OCRPRC) for capitate chondrosis in proximal row carpectomy. J Hand Surg [Am]. 2007;32:1334-1342.