CHAPTER 86
Foot and Ankle Bursitis
Rathi L. Joseph, DO; Thomas H. Hudgins, MD
Definition
Bursae are closed sacs lined by a synovium-like membrane; they contain synovial fluid and are usually located in areas that are subject to friction. Their purpose is to mitigate friction and thus to facilitate the motion that occurs between bones and tendons, bones and skin, or tendons and ligaments [1].
Bursae are classified according to their location, as shown in Table 86.1 [1,2].
Table 86.1
Classification of Bursae According to Location
| Bursal Type | Examples | Description |
| Deep | Retrocalcaneal | Found beneath the fibrous investing fascia Develop in utero Often communicate with joints |
| Subcutaneous | Olecranon, prepatellar | Develop during childhood Do not normally communicate with the adjacent joint |
| Adventitious | Malleolar, metatarsal head | Often have a thick, fibrous wall Are susceptible to inflammatory changes |
Symptomatic malleolar bursae most likely result from abnormal contact pressures. They may also be secondary to shear forces that arise between the bony malleoli and the patient s footwear, particularly boots or athletic shoes that surround the ankle. These may occur either medially or laterally. However, medial bursae are more common [1]. The bone prominences of the malleoli have little inherent soft tissue to protect them from these excessive pressures. The body responds to this abnormal stress by developing an adventitious bursa at this site. The skin and subcutaneous tissues are then able to glide over the bone prominences and thus dissipate these excessive forces. Sometimes, these bursae may become inflamed, resulting in bursitis.
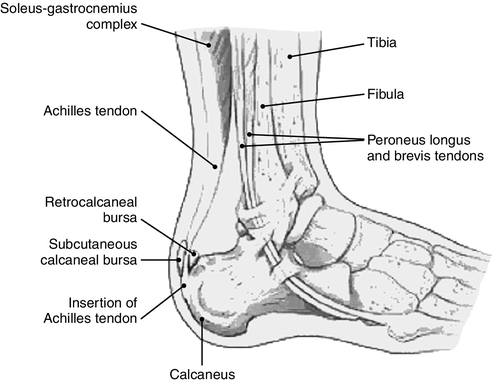
The posterior heel includes the retrocalcaneal bursa, which is located between the calcaneus and the Achilles tendon insertion site, and the retroachilles bursa, which is located between the Achilles tendon and the skin. Each bursa is a potential site of inflammation. The most common cause of posterior heel bursitis is ill-fitting footwear with a stiff posterior edge that abrades the area of the Achilles tendon insertion. Retrocalcaneal inflammation may also be associated with a prominence of the posterosuperior lateral aspect of the calcaneus, causing irritation of the bursa, called a Haglund deformity or pump bump. This entity often goes hand-in-hand with retrocalcaneal bursitis, and frequently there is an element of insertional tendinitis as well.
Although Haglund deformity is more commonly found in women who wear high-heeled shoes, it is sometimes found in hockey players who wear a rigid heel counter that causes irritation. The population of patients that has this superolateral bone prominence tends to be younger than the patients with retrocalcaneal bursitis [3]. Numerous biomechanical risk factors have been associated with Haglund deformity. These include a high-arch cavus foot, rearfoot varus, rearfoot equinus, and trauma to the apophysis in childhood [4–6] (Fig. 86.1).
Bursitis can also occur in the forefoot and may involve the intermetatarsal bursae or the adventitial bursae beneath the metatarsal heads [2].
Risk factors for foot and ankle bursitis are outlined in Table 86.2. Runners, especially those who train uphill, sustain repeated ankle dorsiflexion. Repetitive stress through this motion can lead to bursitis. Also, runners and recreational walkers with sudden increase in mileage are at risk for acquiring symptoms of tenderness, swelling, redness, and pain near the insertion of the Achilles tendon. The most common cause of ankle bursitis is tight-fitting shoes with a firm heel counter. Women wearing high-heeled shoes, runners with improper shoe fit or overworn footwear, skaters, and patients with lower extremity edema are susceptible to development of ankle bursitis. Other important causes of bursitis, in general, are trauma, infection, rheumatoid arthritis, and gout.
Table 86.2
Risk Factors for Foot and Ankle Bursitis
| Type of Bursitis | Risk Factors |
| Malleolar | Commonly found in repetitive overactivity in boot-wearing athletes, such as ice skaters |
| Retrocalcaneal | Athletic overactivity associated with repetitive trauma Most common in long-distance runners who run uphill as a training method Hindfoot varus Rigid plantar-flexed first ray |
| Retroachilles | Commonly found in women who wear high-heeled shoes In the athletic population, it is often found in hockey players who wear a rigid heel counter that causes irritation Retrocalcaneal bursitis Achilles tendinitis High-arch cavus foot Hindfoot varus Hindfoot equinus Trauma to the apophysis in childhood |
| Metatarsal | First metatarsal: dancers, squash players, or skiers Second to fourth metatarsals: chronic inflammatory arthritis |
Symptoms
With malleolar bursitis, there may be exquisite tenderness surrounding the inflamed bursa, a fluctuant mass over the medial malleolus, and decreased range of motion of the ankle.
Retrocalcaneal bursitis is hallmarked by pain that is anterior to the Achilles tendon and just superior to its insertion on the os calcis. Compression of the bursa between the calcaneus and the Achilles tendon occurs every time the ankle is dorsiflexed; in a runner, the repetitions are countless, particularly with uphill running, when ankle dorsiflexion is increased. Patients often develop a limp, and wearing of shoes may eventually become increasingly painful. Thus, it is not surprising that long-distance runners who use uphill running as a training method frequently develop retrocalcaneal bursitis.
Patients with retroachilles bursitis are often asymptomatic. However, when symptoms occur, the patient usually presents with a painful, tender subcutaneous swelling overlying the Achilles tendon, usually at the level of the shoe counter. The overlying skin may be hyperkeratotic or reddened.
Patients with metatarsal bursitis usually have exquisite tenderness surrounding the inflamed bursa, swelling over the metatarsal head, and decreased range of motion of the metatarsophalangeal joint.
Physical Examination
The physical examination findings in bursitis are described in Table 86.3.
Table 86.3
Bursitis—Physical Findings
| Type of Bursitis | Physical Findings |
| Malleolar | Painful, tender subcutaneous swelling overlying the malleolus Overlying skin may be hyperkeratotic or reddened. |
| Retrocalcaneal | Tenderness and bogginess along the medial and lateral aspects of the Achilles tendon at its insertion Posterior heel pain with passive ankle dorsiflexion Posterior heel pain with active-resisted plantar flexion A positive two-finger squeeze test result: pain elicited by application of pressure both medially and laterally with two fingers just superior and anterior to the Achilles insertion |
| Retroachilles | Painful, tender subcutaneous swelling overlying the Achilles tendon, usually at the level of the shoe counter, and on lateral side of Achilles tendon Overlying skin may be hyperkeratotic or reddened. |
| Metatarsal | If a superficial bursa is affected, there will be signs of acute inflammation, with fluctuant swelling and warmth. If a deep bursa is affected, tissues are tight and congested. Pain with direct pressure, compression, or dorsiflexion of the associated digit An overlying callus may suggest that this is a high-pressure site during normal gait. |
The physical examination includes inspection of the patient’s foot at rest and in a weight-bearing position. A visual survey of the foot may reveal swelling, bone deformities, bruising, or skin breaks. The physician should palpate bone prominences and tendinous insertions near the heel and midfoot, noting any tenderness or palpable defects. Passive range of motion of the foot and ankle joints is assessed for indications of restricted movement. Foot posture and arch formation are visually examined while the patient is bearing weight; the physician is looking for abnormal pronation or other biomechanical irregularities. The wear pattern on the posterior interior wall of the shoe should also be examined.
In general, the site of the inflamed bursa is fluctuant and may have some mild associated tenderness and warmth. The patient should be examined closely for any erythema, edema, hypersensitivity, fever, or swollen lymph nodes to rule out septic bursitis.
Insertional tendinosis involves degeneration, not inflammation, of the most distal portion of the Achilles tendon and its attachment on the calcaneal tuberosity. Distinguishing insertional Achilles tendinosis from retrocalcaneal bursitis or osseous impingement, although desirable, is difficult because both may be a continuum of the same disease process or can coexist.
Functional Limitations
Adhesions of the surface of a bursa limit the degree of movement of the associated joint. Pain is a common cause of decreased function. The patient may be limited in ambulation, climbing stairs, and sports activity. The patient also may be limited in footwear, such as protective boots for work.
Diagnostic Studies
Careful physical examination will often yield the cause of most heel pain. Nonetheless, physicians often order radiographs to aid in the diagnostic workup and to exclude osseous causes of the pain. The radiographic findings of bursitis are listed in Table 86.4.
Table 86.4
Bursitis—Radiographic Findings
| Type of Bursitis | Radiographic Findings |
| Malleolar | Diagnosis is essentially clinical, and further evaluation is not required. |
| Retrocalcaneal | Magnetic resonance imaging shows a bursal fluid collection with low signal intensity on T1-weighted images and high signal intensity on T2-weighted and STIR images. A bursa larger than 1 mm anteroposteriorly, 7 mm craniocaudally, or 11 mm transversely is considered abnormal [7]. |
| Retroachilles | Diagnosis is essentially clinical, and further evaluation is not required. It may be discovered incidentally at magnetic resonance imaging performed to evaluate other heel injuries. Its appearance is similar to that of retrocalcaneal bursitis and consists of a bursal fluid collection just posterior to the distal Achilles tendon. |
| Metatarsal | Magnetic resonance imaging shows a well-defined fluid collection at a pressure point and demonstrates low signal intensity on T1-weighted images and high signal intensity on T2-weighted and STIR images. Small fluid collections with a transverse diameter of 3 mm or less in the first three intermetatarsal bursae may be physiologic. Peripheral enhancement is with gadopentetate dimeglumine [8]. |
Levy and colleagues [9] demonstrated that routine radiographs are of limited value in the initial evaluation of nontraumatic plantar heel pain in adults and are not necessary in the initial evaluation. They suggested that radiographs should be reserved for patients who do not improve as expected or present with an unusual history or confounding physical findings.
Multiple studies have attempted to delineate Haglund deformity radiographically by looking at the height, length, and angular relationships of the calcaneus. Most authors cannot recommend one particular radiographic view as being consistently helpful in demonstrating this bone prominence or in making a diagnosis or planning treatment. Ultrasonography can be used to visualize an anechoic area of fluid and can be helpful in medication placement [10].
Treatment
The treatment of bursitis is summarized in Table 86.5.
Table 86.5
Bursitis—Treatment
| Type of Bursitis | Treatment |
| Malleolar | Boot modification or change of footwear Doughnut-shaped cushion made to fit over malleoli Rest and activity modification |
| Retrocalcaneal | Rest and activity modification (e.g., avoidance of running and walking up hills and stairs) Encourage athletes to change running shoes on a regular basis Biomechanical control in the form of temporary heel lifts, tape immobilization, and, if abnormal pronation is present, custom foot orthotics Slight heel elevation with a felt heel pad A night splint to help keep the Achilles tendon and plantar fascia stretched to relieve acute morning pain and stiffness |
| Retroachilles | Rest and activity modification Heat application Padding Wearing a soft, nonrestrictive shoe without a counter (e.g., clogs, sandals) |
| Metatarsal | Rest and activity modification Protective padding Assess for any underlying deformity or foot type with abnormal function |
Initial
In general, nonoperative treatment of foot and ankle bursitis is always recommended first. Conservative treatment of heel pain, in general, includes use of nonsteroidal anti-inflammatory agents, physical therapy, and avoidance of repetitive high-impact activities [11]. If there is some associated Achilles tendon or plantar fascia disease present, a night splint may help relieve the acute pain many patients experience when they first get up in the morning.
Conservative treatment of general heel pain also includes use of heel lifts and open-back shoes. A portion of the heel counter can be cut away and replaced with a soft leather insert to cause less friction at the site where the heel counter meets the skin. Shoes without laces are to be avoided because they inherently fit close to the heel. Insertion of a heel cup in the shoe may help raise the inflamed region slightly above the restricting heel counter of the shoe. A heel cup also should be placed in the other shoe to avoid introducing leg length discrepancy. Pressure-off silicone sheet pads can be used long term when shoes with counters are worn. Custom orthoses are prescribed for those who have underlying structural abnormalities causing the symptoms.
Rehabilitation
The rehabilitation of bursitis is described in Table 86.6.
Table 86.6
Bursitis—Rehabilitation
| Type of Bursitis | Rehabilitation |
| Malleolar | Physical therapy is usually not necessary unless joint range of motion is affected. Physical therapy is then necessary to maintain ankle range of motion. |
| Retrocalcaneal | Physical therapy to teach stretching exercises of the Achilles tendon and plantar fascia Ice can be applied for 15 to 20 minutes, several times a day, during the acute period. Some clinicians also advocate use of contrast baths. Alternative means of maintaining strength and cardiovascular fitness include swimming, water aerobics, and other aquatic exercises. |
| Retroachilles | Physical therapy to teach stretching exercises of the Achilles tendon |
The patient is allowed weight bearing as tolerated and should be instructed to elevate the foot when not walking. If the patient has had surgery, the dressing is removed 3 days postoperatively, and the patient is allowed to shower. The patient is encouraged to perform active range of motion exercises at least three times a day for 10 minutes each time. The patient is allowed to wear regular shoes as soon as this is tolerated.
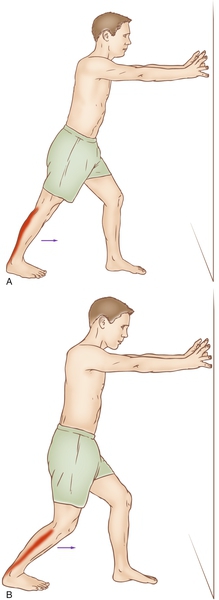
Physical therapy is used to teach stretching exercises of the Achilles tendon and plantar fascia to preserve range of motion. This gradual progressive stretching of the Achilles tendon may help relieve impingement on the subtendinous bursa. Stretching of the Achilles tendon can be performed in the following manner: place the affected foot flat on the floor and lean forward toward the wall until a gentle stretch is felt within the ipsilateral Achilles tendon; maintain the stretch for 20 to 60 seconds and then relax. These stretches should be performed with the knee extended and repeated with the knee flexed, as seen in Figure 86.2. For the benefit of the stretching program to be maximized, repeat for several stretches per set, several times per day. Avoid ballistic (abrupt, jerking) stretches. Progress to calf dips on a stair for functional stretching and eccentric strengthening. Contrast baths and ice massage are also used in the acute management. Icing can be performed for 15 to 20 minutes, several times a day, during the acute period.
The athlete may be expected to return to play without restrictions after demonstrating resolution of symptoms, resolution of physical examination findings (e.g., limping, tenderness on palpation), and adequate performance of sports-specific practice drills without recurrence of symptoms or physical examination findings.
Procedures
If the patient remains symptomatic or finds the bursa to be aesthetically displeasing, the bursa can be aspirated and injected with a 1- to 2-mL solution of a corticosteroid. Many clinicians prefer not to repeat this injection more than once because the risk of tendon rupture is not worth the limited benefits offered by corticosteroid injection. However, tendon rupture is a known complication when corticosteroids are injected directly into the tendon substance [12,13]. There is no available evidence suggesting an association between corticosteroid injections of ankle bursae and Achilles tendon rupture, although most practitioners believe that ultrasound guidance can decrease the possibility of injection within the tendon itself.
Surgery
About 10% of patients with retrocalcaneal or supracalcaneal bursitis do not respond to conservative treatment and seek a surgical solution [14]. Open surgical techniques focus on resection of the posterosuperior portion of the calcaneus or performance of a calcaneal wedge osteotomy with or without débridement of diseased Achilles tendon. Endoscopic techniques provide visualization of the tendon-bone relationship with endoscopic inspection and allow precise débridement and evaluation for residual impingement. The smaller access allows easier closure and less extensive postoperative care. The small incision minimizes the potential for wound dehiscence, a painful scar, and nerve entrapment in scar tissue, and it provides a cosmetically superior result. Endoscopic techniques have had higher patient satisfaction and lower complication rates than open surgical treatment [15].
Potential Disease Complications
The primary disease complication is chronic bursitis with intractable pain that may limit footwear and joint mobility. Adhesive bursitis is another potential disease complication that may occur with chronic bursitis. In adhesive bursitis, two adjacent layers of the bursa may adhere and significantly decrease joint range of motion.
The course of bursitis may also be complicated by infection causing a septic bursitis. In this case, immediate surgical débridement and intravenous antibiotics are indicated. A Staphylococcus aureus organism is most often responsible and should be treated with appropriate antibiotics.
Potential Treatment Complications
Risks of chronic nonsteroidal anti-inflammatory drug use include gastrointestinal bleeding, renal toxicity, hypertension, and other cardiovascular complications; thus, duration should be kept to a minimum. Systemic complications may be lessened by use of topical nonsteroidal anti-inflammatory drugs to the affected area only.
Complications of open, endoscopic, and fluoroscopic surgical procedures include skin breakdown, avulsion of the Achilles tendon, inadequate decompression with recurrent pain, sensitive and disfiguring scars, altered sensation, and stiffness. In one series, open treatment was associated with a 14% rate of infection, a 17% rate of wound breakdown, a 23% rate of scar tenderness, and a 38% rate of altered sensation [16].
The role of corticosteroid injections in the treatment of retrocalcaneal bursitis is controversial. There have been numerous case reports of patients who have sustained a tendon rupture after peritendinous injections of corticosteroids for the treatment of tendinitis or tendinosis; however, little has been reported on retrocalcaneal intrabursal injections for the treatment of bursitis. Martin and associates [17] investigated the mechanical properties of and histologic changes in rabbit Achilles tendons after peritendinous steroid injection. They found that local injections of corticosteroid, both within the tendon substance and into the retrocalcaneal bursa, adversely affected the biomechanical properties of rabbit Achilles tendons. Another animal study also showed adverse effects of local injections of corticosteroid (within the tendon substance and into the retrocalcaneal bursa) on the biomechanical properties of Achilles tendons [18].
Prolonged immobilization may result in adhesions and subsequent joint stiffening. Thus, patients should have early mobilization after low-grade ankle sprains to prevent increased risk of ankle bursitis.
Patients with ankle bursitis may benefit from accelerated rehabilitation within 7 days of injury to improve muscle strength, sensorimotor control, and range of motion, much like patients after ankle sprains [19], but this has not yet been studied.







