CASE 86


History: A patient presents with fatigue.
1. What should be included in the differential diagnosis? (Choose all that apply.)
A. Sleep apnea
2. This patient is acyanotic and has a shunt lesion. What is the most likely diagnosis?
C. Atrioventricular septal defect
3. Which of the following is not characteristic of Eisenmenger syndrome?
A. Cyanosis
C. Decreased pulmonary vascularity
4. Which pulmonary-to-systemic flow ratio (Qp : Qs) is characteristic of Eisenmenger syndrome?
A. 0.7 : 1
B. 1 : 1
C. 1.5 : 1
D. 3 : 1
ANSWERS
References
Diller GP, Gatzoulis MA. Pulmonary vascular disease in adults with congenital heart disease. Circulation. 2007;115(8):1039–1050.
Walker CM, Reddy GP, Steiner RM. Radiology of the heart. In: Rosendorff C, ed. Essential Cardiology. ed 3 New York: Springer; 2013.
Wang ZJ, Reddy GP, Gotway MB, et al. Cardiovascular shunts: MR imaging evaluation. Radiographics. 2003;23(Spec No):S181–S194.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 16–18.
Comment
Etiology and Clinical Implications
When an atrial septal defect is long-standing, pulmonary pressure can increase dramatically and cause marked enlargement of the pulmonary arteries. Although there are numerous causes of pulmonary hypertension, it has been reported that an intracardiac shunt is the most common cause when there is massive pulmonary artery enlargement. As the pulmonary pressure increases, left-to-right shunting decreases, and if the pulmonary pressure eventually exceeds systemic pressure, flow across the septal defect can reverse and become a right-to-left shunt; this is known as Eisenmenger syndrome. In the setting of Eisenmenger syndrome, patients may be cyanotic, and paradoxical embolism can result in a transient ischemic attack or a stroke.
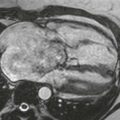
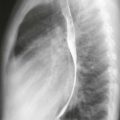
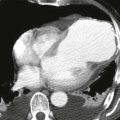
Imaging
Radiographs can demonstrate marked enlargement of the central pulmonary arteries, consistent with pulmonary arterial hypertension (Figs. A and B). The pulmonary vascularity is typically decreased in the setting of Eisenmenger syndrome. Velocity-encoded cine MRI can be performed to obtain the Qp : Qs and quantify the severity of the shunt.