Procedure 85 Wrist Denervation
Indications
 Painful arthrosis of the wrist, preservation of functional movement. Common etiologic conditions include scaphoid nonunion or scapholunate advanced collapse (SNAC/SLAC), Kienböck disease, inflammatory arthropathies, and posttraumatic arthritis following distal radius fractures or carpal dislocations.
Painful arthrosis of the wrist, preservation of functional movement. Common etiologic conditions include scaphoid nonunion or scapholunate advanced collapse (SNAC/SLAC), Kienböck disease, inflammatory arthropathies, and posttraumatic arthritis following distal radius fractures or carpal dislocations.
 Patients who require wrist motion for daily function, for example, contralateral upper extremity amputees or dependence on assistive devices for ambulation.
Patients who require wrist motion for daily function, for example, contralateral upper extremity amputees or dependence on assistive devices for ambulation.
 The patient in Figure 85-1 suffers from chronic wrist pain secondary to Kienböck disease. He is a bilateral above-knee amputee and depends on both upper extremities for ambulation.
The patient in Figure 85-1 suffers from chronic wrist pain secondary to Kienböck disease. He is a bilateral above-knee amputee and depends on both upper extremities for ambulation.
 Patient selection is controversial. Local anesthetic blocks with postinjection assessment of pain relief and functional improvement are useful in determining which patients may benefit from the procedure.
Patient selection is controversial. Local anesthetic blocks with postinjection assessment of pain relief and functional improvement are useful in determining which patients may benefit from the procedure.
Examination/Imaging
Clinical Examination
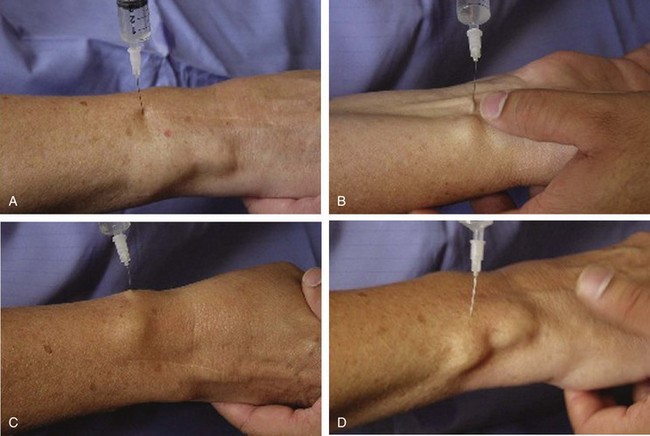
 Injection of 1 mL of bupivacaine (Marcaine) 0.5% approximately 1 cm ulnar and 3 cm proximal to the Lister tubercle has been shown to reliably deliver medication to both the posterior interosseous nerve (PIN) and the anterior interosseous nerve (AIN). The needle is inserted; when resistance of the interosseous membrane is felt, the needle is withdrawn slightly, and the medication is injected to anesthetize the PIN. Next, the needle is advanced just through the membrane, and another injection is performed to anesthetize the AIN. Blocking the AIN and PIN helps indicate whether partial denervation will be beneficial (Fig. 85-2A).
Injection of 1 mL of bupivacaine (Marcaine) 0.5% approximately 1 cm ulnar and 3 cm proximal to the Lister tubercle has been shown to reliably deliver medication to both the posterior interosseous nerve (PIN) and the anterior interosseous nerve (AIN). The needle is inserted; when resistance of the interosseous membrane is felt, the needle is withdrawn slightly, and the medication is injected to anesthetize the PIN. Next, the needle is advanced just through the membrane, and another injection is performed to anesthetize the AIN. Blocking the AIN and PIN helps indicate whether partial denervation will be beneficial (Fig. 85-2A).
 If complete denervation is planned, 1 mL of bupivacaine 0.5% is injected around the remaining nerves, including the palmar branch of the median nerve, branches of the radial nerve, the dorsal cutaneous branch of the ulnar nerve, and the recurrent intermetacarpal branches (Fig. 85-2B to D).
If complete denervation is planned, 1 mL of bupivacaine 0.5% is injected around the remaining nerves, including the palmar branch of the median nerve, branches of the radial nerve, the dorsal cutaneous branch of the ulnar nerve, and the recurrent intermetacarpal branches (Fig. 85-2B to D).
 After injection, pain is expected to be diminished considerably, and work output should at least double.
After injection, pain is expected to be diminished considerably, and work output should at least double.
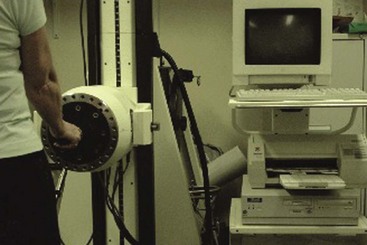
 A Baltimore Therapeutic Equipment (BTE) Work Simulator (Fig. 85-3) can be used to assess work function before and after bupivacaine injection. Functional assessment provides the most accurate prediction of success following wrist denervation and provides the patient with a good idea of what to expect after surgery.
A Baltimore Therapeutic Equipment (BTE) Work Simulator (Fig. 85-3) can be used to assess work function before and after bupivacaine injection. Functional assessment provides the most accurate prediction of success following wrist denervation and provides the patient with a good idea of what to expect after surgery.
Exposures
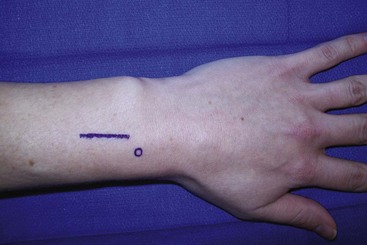
 For partial denervation (PIN and AIN), a single longitudinal or transverse dorsal incision is used. Beginning about 2 cm proximal to the ulnar head, a 2- to 3-cm incision is made over the interval between the distal radius and ulna. The deep antebrachial fascia is incised longitudinally, exposing the extensor pollicis longus (third compartment) and extensor digitorum communis (fourth compartment) (Fig. 85-4).
For partial denervation (PIN and AIN), a single longitudinal or transverse dorsal incision is used. Beginning about 2 cm proximal to the ulnar head, a 2- to 3-cm incision is made over the interval between the distal radius and ulna. The deep antebrachial fascia is incised longitudinally, exposing the extensor pollicis longus (third compartment) and extensor digitorum communis (fourth compartment) (Fig. 85-4).
 Full denervation can be done through four incisions. Incision 1: A transverse incision is made 3 to 5 cm proximal from the wrist on the dorsal forearm (Fig. 85-5). If a more distal incision is used, some articular branches from the PIN may not be completely eliminated. The extensor retinaculum over the fourth compartment is partially incised, and the finger extensor tendons are retracted ulnarly. The PIN is visualized on the radial floor of the fourth extensor compartment and isolated. The interosseous membrane is incised next, and branches of the AIN are visualized. Incision 2: A dorsal ulnar incision (see Fig. 85-5) is made over the wrist at the level of the ulnar head with dissection down to the extensor retinaculum. In the skin flap, the dorsal branch of the ulnar nerve is isolated. Incision 3: Through a volar radial incision centered over the radial artery at the level of the wrist and distal forearm, a plane is developed under the radial vessels, the palmar cutaneous branch of the median nerve, and the radial nerve (Fig. 85-6). Incision 4: A transverse incision is made over the dorsal base of the metacarpals and then through fascia to expose recurrent intermetacarpal branches (see Figs. 85-5 and 85-6).
Full denervation can be done through four incisions. Incision 1: A transverse incision is made 3 to 5 cm proximal from the wrist on the dorsal forearm (Fig. 85-5). If a more distal incision is used, some articular branches from the PIN may not be completely eliminated. The extensor retinaculum over the fourth compartment is partially incised, and the finger extensor tendons are retracted ulnarly. The PIN is visualized on the radial floor of the fourth extensor compartment and isolated. The interosseous membrane is incised next, and branches of the AIN are visualized. Incision 2: A dorsal ulnar incision (see Fig. 85-5) is made over the wrist at the level of the ulnar head with dissection down to the extensor retinaculum. In the skin flap, the dorsal branch of the ulnar nerve is isolated. Incision 3: Through a volar radial incision centered over the radial artery at the level of the wrist and distal forearm, a plane is developed under the radial vessels, the palmar cutaneous branch of the median nerve, and the radial nerve (Fig. 85-6). Incision 4: A transverse incision is made over the dorsal base of the metacarpals and then through fascia to expose recurrent intermetacarpal branches (see Figs. 85-5 and 85-6).
Pitfalls
The AIN and PIN are accompanied by the anterior and posterior interosseous arteries, respectively. Care must be taken to identify and protect these arteries during exposure to avoid injury and postoperative bleeding.
There is controversy regarding the merits of full denervation versus partial denervation. There is some evidence in the literature that suggests the results of partial denervation may deteriorate over time. However, we prefer partial denervation because it is simple, does not require multiple incisions, and has been shown to be effective in multiple reports.
Procedure
Step 1: Partial Denervation
 The extensor pollicis longus (EPL) is retracted radially, and the radial border of the fourth compartment is visualized by partially incising the retinaculum proximally. The digital extensor tendons are retracted ulnarly. The PIN and its vessels are visualized on the radial floor of the fourth dorsal compartment.
The extensor pollicis longus (EPL) is retracted radially, and the radial border of the fourth compartment is visualized by partially incising the retinaculum proximally. The digital extensor tendons are retracted ulnarly. The PIN and its vessels are visualized on the radial floor of the fourth dorsal compartment.
 The PIN is identified and dissected free using a longitudinal spreading technique. A 1- to 2-cm segment of nerve is resected sharply (Fig. 85-7).
The PIN is identified and dissected free using a longitudinal spreading technique. A 1- to 2-cm segment of nerve is resected sharply (Fig. 85-7).
 The interosseous membrane is visible beneath the PIN. The interosseous membrane is carefully incised longitudinally to expose the AIN. The AIN is identified and dissected free using a longitudinal spreading technique. A 1- to 2-cm segment of nerve is resected sharply as far distally as possible (Figs. 85-8 and 85-9).
The interosseous membrane is visible beneath the PIN. The interosseous membrane is carefully incised longitudinally to expose the AIN. The AIN is identified and dissected free using a longitudinal spreading technique. A 1- to 2-cm segment of nerve is resected sharply as far distally as possible (Figs. 85-8 and 85-9).
Step 2: Full Denervation: Incision 2
 PIN and AIN denervations are first performed through incision 1 as described previously.
PIN and AIN denervations are first performed through incision 1 as described previously.
 The plane between the extensor retinaculum and the subcutaneous fat is developed. The articular perforating fibers of the dorsal branch of the ulnar sensory nerve are isolated, cauterized, and resected (Fig. 85-10).
The plane between the extensor retinaculum and the subcutaneous fat is developed. The articular perforating fibers of the dorsal branch of the ulnar sensory nerve are isolated, cauterized, and resected (Fig. 85-10).
 Often, the excision of these perforating articular branches is accomplished blindly with dissection of the layer between the ulnar sensory nerve and the fascia. The index finger can be used as a blunt dissector, creating a “controlled degloving” of the skin over the dorsum of the wrist and the base of the ulnar head.
Often, the excision of these perforating articular branches is accomplished blindly with dissection of the layer between the ulnar sensory nerve and the fascia. The index finger can be used as a blunt dissector, creating a “controlled degloving” of the skin over the dorsum of the wrist and the base of the ulnar head.
Step 3: Full Denervation: Incision 3
 The radial artery carries sympathetic pain fibers to the wrist joint. A plane is developed deep to the artery and veins, and a segment of periarterial tissue is resected. Sympathetic branches from the artery to the wrist joint are divided (Fig. 85-11).
The radial artery carries sympathetic pain fibers to the wrist joint. A plane is developed deep to the artery and veins, and a segment of periarterial tissue is resected. Sympathetic branches from the artery to the wrist joint are divided (Fig. 85-11).
 A plane is created deep to the palmar cutaneous branch of the median nerve volarly, and the radial sensory nerve dorsally that will meet the plane from incision 2. Again, the index finger can be used to develop these planes (Fig. 85-12).
A plane is created deep to the palmar cutaneous branch of the median nerve volarly, and the radial sensory nerve dorsally that will meet the plane from incision 2. Again, the index finger can be used to develop these planes (Fig. 85-12).
Postoperative Care and Expected Outcomes
Buck-Gramcko D. Denervation of the wrist joint. J Hand Surg [Am]. 1977;2:54-61.
Ferres A, Suso S, Foucher G. Wrist denervation: surgical considerations. J Hand Surg [Br]. 1995;20:769-772.
Grafe MW, Kim PD, Rosenwasser MP, Strauch RJ. Wrist denervation and the anterior interosseous nerve: anatomic considerations. J Hand Surg [Am]. 2005;30:1221-1225.
Lin DL, Lenhart MK, Farber GL. Anatomy of the anterior interosseous innervation of the pronator quadratus: evaluation of structures at risk in the single dorsal incision of wrist denervation technique. J Hand Surg [Am]. 2006;31:904-907.
Weinstein LP, Berger RA. Analgesic benefit, functional outcome, and patient satisfaction after partial wrist denervation. J Hand Surg [Am]. 2002;27:833-839.