Procedure 84 Sauve-Kapandji Arthrodesis for Distal Radioulnar Joint Arthritis
![]() See Video 63: Shelf Arthroplasty for Rheumatoid DRUJ Arthritis
See Video 63: Shelf Arthroplasty for Rheumatoid DRUJ Arthritis
Indications
 Arthritis of the distal radioulnar (DRU) joint in young (<45 years of age) active patients with stable radiocarpal ligaments. This procedure maintains the ulnocarpal buttress and retains the triangular fibrocartilage complex (TFCC) to provide a more physiologic pattern of force transmission from the hand to the forearm and offers improved strength and function.
Arthritis of the distal radioulnar (DRU) joint in young (<45 years of age) active patients with stable radiocarpal ligaments. This procedure maintains the ulnocarpal buttress and retains the triangular fibrocartilage complex (TFCC) to provide a more physiologic pattern of force transmission from the hand to the forearm and offers improved strength and function.
 Malunited distal radius fractures with DRU joint arthritis.
Malunited distal radius fractures with DRU joint arthritis.
 Early presentation of rheumatoid arthritis with intact wrist ligaments.
Early presentation of rheumatoid arthritis with intact wrist ligaments.
 Chronic DRU joint instability without arthritis.
Chronic DRU joint instability without arthritis.
 In the setting of radiocarpal instability, the Sauve-Kapandji procedure can be performed to stabilize the ulnar wrist, which may obviate the immediate need for a partial or total wrist fusion.
In the setting of radiocarpal instability, the Sauve-Kapandji procedure can be performed to stabilize the ulnar wrist, which may obviate the immediate need for a partial or total wrist fusion.
Examination/Imaging
Clinical Examination
 Differentiating DRU joint arthritis and ulnocarpal impaction syndrome is important in treating degenerative conditions of the ulnar wrist. Both can present with pain and swelling, decreased grip strength, and stiffness. Moreover, both may coexist and require treatment to relieve symptoms. This distinction should be made in order to proceed with the appropriate surgery.
Differentiating DRU joint arthritis and ulnocarpal impaction syndrome is important in treating degenerative conditions of the ulnar wrist. Both can present with pain and swelling, decreased grip strength, and stiffness. Moreover, both may coexist and require treatment to relieve symptoms. This distinction should be made in order to proceed with the appropriate surgery.
 Visible subluxation of the DRU joint indicating instability due to ligamentous laxity or injury.
Visible subluxation of the DRU joint indicating instability due to ligamentous laxity or injury.
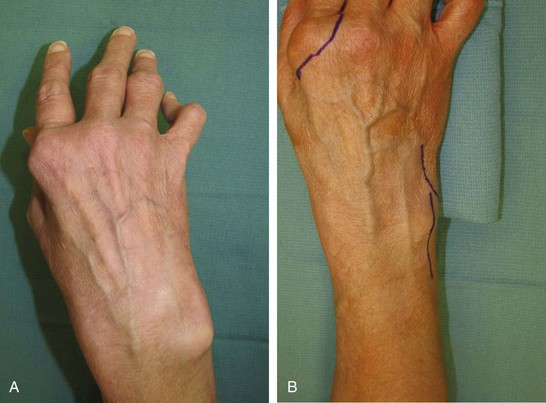
Imaging
 Posteroanterior, oblique, and lateral radiographs of the wrist are useful to identify signs of degenerative arthritis. Findings include joint space narrowing, volar subluxation of the radius, and osteophyte formation along the proximal margin of the ulnar head, typically sparing the sigmoid notch (Fig. 84-1A and B).
Posteroanterior, oblique, and lateral radiographs of the wrist are useful to identify signs of degenerative arthritis. Findings include joint space narrowing, volar subluxation of the radius, and osteophyte formation along the proximal margin of the ulnar head, typically sparing the sigmoid notch (Fig. 84-1A and B).
 Assess for ulnar carpus translation present preoperatively because this may indicate a need for a wrist-stabilizing procedure such as a radiolunate, radioscapholunate, or total wrist arthrodesis.
Assess for ulnar carpus translation present preoperatively because this may indicate a need for a wrist-stabilizing procedure such as a radiolunate, radioscapholunate, or total wrist arthrodesis.
 Computed tomography (CT) or magnetic resonance imaging (MRI) of the DRU joint will better define the articular surface and joint congruity.
Computed tomography (CT) or magnetic resonance imaging (MRI) of the DRU joint will better define the articular surface and joint congruity.
Surgical Anatomy
 DRU joint fit can be affected by changes in the position of the sigmoid notch. A common cause of poor fit of the DRU joint is injuries affecting the length of the radius relative to the ulna. Although the shape of this joint and the relative bone length are variable, joint congruency is required for normal function. Clear changes in congruency are usually evident on plain radiographs, but CT or MRI can give better anatomic definition of the bone and joint shape, in addition to the TFCC attachment to the ulnar head fovea.
DRU joint fit can be affected by changes in the position of the sigmoid notch. A common cause of poor fit of the DRU joint is injuries affecting the length of the radius relative to the ulna. Although the shape of this joint and the relative bone length are variable, joint congruency is required for normal function. Clear changes in congruency are usually evident on plain radiographs, but CT or MRI can give better anatomic definition of the bone and joint shape, in addition to the TFCC attachment to the ulnar head fovea.
 The dorsal branch of the ulnar nerve is at risk during incision. Along the ulnar head lies the stabilizing sheath of the extensor carpi ulnaris (ECU) tendon. This sheath must be opened, and the ECU tendon must be displaced when repairing the TFCC.
The dorsal branch of the ulnar nerve is at risk during incision. Along the ulnar head lies the stabilizing sheath of the extensor carpi ulnaris (ECU) tendon. This sheath must be opened, and the ECU tendon must be displaced when repairing the TFCC.
Exposures
 A dorsal midline incision with a zigzag at the wrist is used for wide exposure to the level of the extensor retinaculum (Fig. 84-2A and B).
A dorsal midline incision with a zigzag at the wrist is used for wide exposure to the level of the extensor retinaculum (Fig. 84-2A and B).
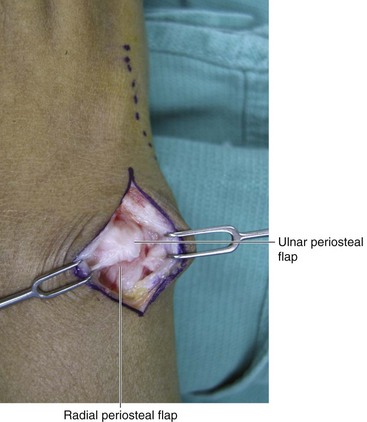
 Approach the ulna between the extensor digiti minimi (EDM) and ECU and incise the periosteum to raise radial and ulnar periosteal flaps for later closure (Fig. 84-3).
Approach the ulna between the extensor digiti minimi (EDM) and ECU and incise the periosteum to raise radial and ulnar periosteal flaps for later closure (Fig. 84-3).
Procedure
Step 1
 A 1-cm segment of ulna bone is removed proximal to the sigmoid notch. The cartilage is removed from the DRU joint bone surfaces with a 3-mm bur until punctate bleeding is seen. A temporary K-wire is placed to stabilize the distal ulna to the radius, and angular positioning is checked by fluoroscopy.
A 1-cm segment of ulna bone is removed proximal to the sigmoid notch. The cartilage is removed from the DRU joint bone surfaces with a 3-mm bur until punctate bleeding is seen. A temporary K-wire is placed to stabilize the distal ulna to the radius, and angular positioning is checked by fluoroscopy.
Step 1 Pearls
Obtain the best possible fit of the DRU joint.
Preoperative ulnar positive variance should be corrected at the time of the arthrodesis.
Some surgeons argue that it is not necessary to prepare the joint in any patient with rheumatoid arthritis because it will likely fuse with immobilization alone. However, the authors recommend visualization and surface preparation of the DRU joint in all cases to ensure fusion.
Step 2
 The resected bone is morselized and used as bone graft around the compressed DRU joint. Placement of bone graft within the DRU joint is avoided by the senior author because it will impede reduction and possibly slow healing by increasing the distance between bone surfaces.
The resected bone is morselized and used as bone graft around the compressed DRU joint. Placement of bone graft within the DRU joint is avoided by the senior author because it will impede reduction and possibly slow healing by increasing the distance between bone surfaces.
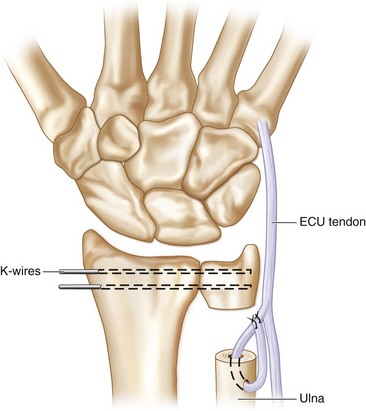
 Stabilization by K-wires is certainly acceptable, but the senior author prefers to use a compression screw to provide more rigid fixation. A 3.5-mm cannulated screw, or a headless screw, is used for internal fixation that is placed over the K-wire. If necessary, a temporary K-wire is placed percutaneously to prevent rotation of the distal ulna fragment. This K-wire can be removed in clinic 3 weeks after the operation.
Stabilization by K-wires is certainly acceptable, but the senior author prefers to use a compression screw to provide more rigid fixation. A 3.5-mm cannulated screw, or a headless screw, is used for internal fixation that is placed over the K-wire. If necessary, a temporary K-wire is placed percutaneously to prevent rotation of the distal ulna fragment. This K-wire can be removed in clinic 3 weeks after the operation.
Step 3
 The goal of the Sauve-Kapandji arthrodesis is to regain painless and stable forearm rotation. The new fibrous pseudarthrosis at the junction between the two ulnar sections can be unstable. During the operation, the position of the two ulnar stumps should be assessed during rotation in a pushing-pulling manner. If the ends are unstable because of soft tissue attenuation, the senior author prefers the ulnar half of the ECU as a tenodesis:
The goal of the Sauve-Kapandji arthrodesis is to regain painless and stable forearm rotation. The new fibrous pseudarthrosis at the junction between the two ulnar sections can be unstable. During the operation, the position of the two ulnar stumps should be assessed during rotation in a pushing-pulling manner. If the ends are unstable because of soft tissue attenuation, the senior author prefers the ulnar half of the ECU as a tenodesis:
 Drill a hole in the dorsal cortex of the distal ulna stump using a 3-mm bur.
Drill a hole in the dorsal cortex of the distal ulna stump using a 3-mm bur.
 The distally based ulnar half of the ECU is woven from inside the ulnar canal and out the hole dorsally and sutured to itself, stabilizing the proximal ulnar stump (Fig. 84-4).
The distally based ulnar half of the ECU is woven from inside the ulnar canal and out the hole dorsally and sutured to itself, stabilizing the proximal ulnar stump (Fig. 84-4).
Procedure
Modified Sauve-Kapandji Procedure
Step 1
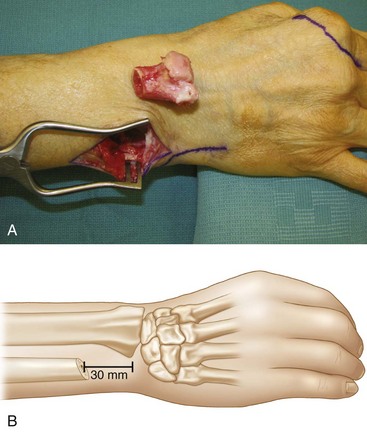
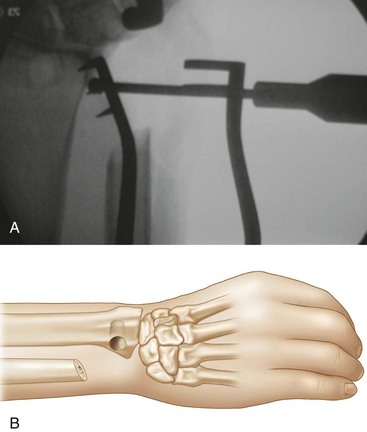
 The senior author prefers the shelf arthroplasty procedure proposed by Fujita and colleagues when there is poor bone quality in the distal part of the ulna. In such situations a routine Sauve-Kapandji procedure would provide insufficient osseous support for the ulnar aspect of the carpus. An oblique osteotomy is made 30 mm proximal to the end of the ulna (Fig. 84-5A and B). The distal ulna is removed and turned 90 degrees with the proximal bone facing the sigmoid notch.
The senior author prefers the shelf arthroplasty procedure proposed by Fujita and colleagues when there is poor bone quality in the distal part of the ulna. In such situations a routine Sauve-Kapandji procedure would provide insufficient osseous support for the ulnar aspect of the carpus. An oblique osteotomy is made 30 mm proximal to the end of the ulna (Fig. 84-5A and B). The distal ulna is removed and turned 90 degrees with the proximal bone facing the sigmoid notch.
Step 2
 A slot is made with a bur over the sigmoid notch to fit the ulna (Fig. 84-6A and B). This ensures greater bone contact to enhance fusion, particularly in situations in which the distal ulna bone quality is poor. It also theoretically gives better ulna-sided support to the ulnar wrist, analogous to a bookshelf construct.
A slot is made with a bur over the sigmoid notch to fit the ulna (Fig. 84-6A and B). This ensures greater bone contact to enhance fusion, particularly in situations in which the distal ulna bone quality is poor. It also theoretically gives better ulna-sided support to the ulnar wrist, analogous to a bookshelf construct.
Step 3
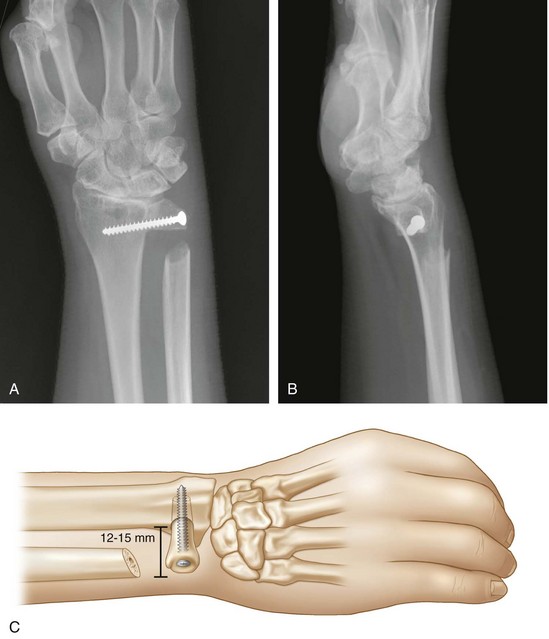
 The proximal end of the cut distal ulna is inserted into the slot in the sigmoid notch for a press fit. A headless screw is placed through the distal ulna and into the radius to provide rigid fixation (Fig. 84-7A to C). Contouring of the head of the distal ulna is necessary to avoid a large bump over the ulnar wrist.
The proximal end of the cut distal ulna is inserted into the slot in the sigmoid notch for a press fit. A headless screw is placed through the distal ulna and into the radius to provide rigid fixation (Fig. 84-7A to C). Contouring of the head of the distal ulna is necessary to avoid a large bump over the ulnar wrist.
Postoperative Care and Expected Outcomes
 Postoperative positioning and early exercises
Postoperative positioning and early exercises
 Intermediate exercises (6 to 8 weeks after surgery)
Intermediate exercises (6 to 8 weeks after surgery)
Fujita S, Masada K, Takeuchi E, et al. Modified Sauve-Kapandji procedure for disorders of the distal radioulnar joint in patients with rheumatoid arthritis. J Bone Joint Surg [Am]. 2006;88:24-28.
Kobayashi A, Futami T, Tadano I, et al. Radiographic comparative evaluation of the Sauve-Kapandji procedure and the Darrach procedure for rheumatoid wrist reconstruction. Mod Rheumatol. 2005;15:187-190.