CASE 84

History: A 20-year-old woman presents with several days of watery diarrhea and cramping abdominal pain.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in the figures? (Choose all that apply.)
2. What is the predisposing factor for the development of pseudomembranous colitis?
3. What is the treatment for pseudomembranous colitis?
A. Clostridium botulinum antitoxin
B. Change the antibiotic regimen
4. Which of the following statements about the pseudomembranous colitis is true?
A. The colitis is due to a toxin produced by Clostridium perfringens.
B. 20% or more of patients carry Clostridium species without symptoms.
C. The disease causes a pancolitis from cecum to rectum.
D. The disease does not extend to the small bowel.
ANSWERS
CASE 84
Pseudomembranous Colitis
1. A, B, C, and E
2. A
3. B
4. B
References
Kawamoto S, Horton KM, Fishman EK. Pseudomembranous colitis: spectrum of imaging findings with clinical and pathologic correlation. Radiographics. 1999;19:887–897.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 313.
Comment
Pseudomembranous colitis is commonly encountered. It actually represents an infection with the bacillus Clostridium difficile, although the relationship is variable. C. difficile can be found in many healthy patients (20% of the population), in whom it does not produce extensive colonization. Under certain circumstances (e.g., during the course of antibiotic therapy or chemotherapy), an overgrowth of this bacterium can develop, which is why this condition is often called antibiotic-associated colitis. However, many episodes of diarrhea associated with antibiotic use are not caused by C. difficile infection; probably only the most severe cases are caused by this bacterium. The relationship is even more difficult to establish in that the onset of symptoms can occur anywhere from a few days to 8 weeks after antibiotics have been initiated, although typically it takes less than 2 weeks.
C. difficile produces several endotoxins, some of which are detectable with laboratory assays. These toxins produce an inflammatory and necrotic change in the mucosa, with subsequent loss of fluid through the wall of the bowel. On sigmoidoscopy there are small raised yellowish plaques, cellular debris, and mucus, hence the term pseudomembranous colitis. The inflammatory process can involve the whole colon, but in a substantial number of patients the rectum is spared or only segments of the colon are involved.
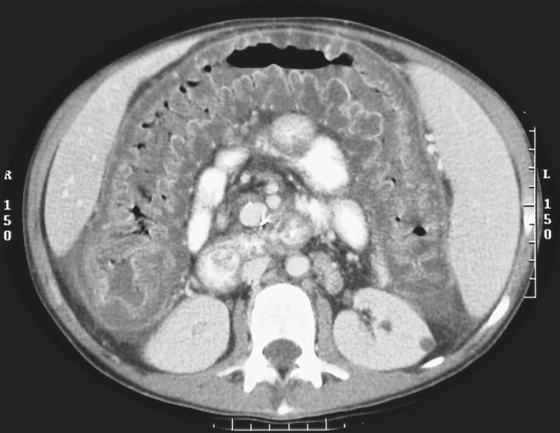
Radiologically, in severe cases the abnormalities may be apparent on plain abdominal images. The findings include thickening of the haustral folds, thickening of the bowel wall, and a shaggy appearance of the mucosa. The changes can mimic ischemia. Barium studies are usually not indicated but show the thickened folds and irregular margins to the barium. Toxic megacolon can occur in patients with this condition. CT is probably the best modality for evaluating severe cases because the thickened bowel is readily apparent and the study does not precipitate any complications (see figures). Treatment is discontinuation of the antibiotics, sometimes use of vancomycin, and supportive therapy.







