Procedure 83 Darrach Procedure
![]() See Video 62: Darrach Procedure
See Video 62: Darrach Procedure
Indications
 Older, sedentary patients with posttraumatic distal radioulnar (DRU) joint arthritis, rheumatoid arthritis, and osteoarthritis without preexisting radiocarpal instability.
Older, sedentary patients with posttraumatic distal radioulnar (DRU) joint arthritis, rheumatoid arthritis, and osteoarthritis without preexisting radiocarpal instability.
 Destruction of the triangular fibrocartilage complex with caput ulna syndrome and painful pronation and supination of the DRU joint.
Destruction of the triangular fibrocartilage complex with caput ulna syndrome and painful pronation and supination of the DRU joint.
 The Darrach procedure (distal ulna head excision) is preferred in patients with no ulnar translation of the carpus and low chance of translation in the future.
The Darrach procedure (distal ulna head excision) is preferred in patients with no ulnar translation of the carpus and low chance of translation in the future.
 In the setting of radiocarpal instability, the Darrach procedure can be performed concomitantly with a partial or total wrist fusion.
In the setting of radiocarpal instability, the Darrach procedure can be performed concomitantly with a partial or total wrist fusion.
Examination/Imaging
Clinical Examination
 Evaluate active and passive wrist and DRU joint motion and compare with the opposite side. The affected wrist should be taken through full wrist motions of flexion-extension, pronation-supination, and radioulnar deviation with axial loading to assess stability and pain.
Evaluate active and passive wrist and DRU joint motion and compare with the opposite side. The affected wrist should be taken through full wrist motions of flexion-extension, pronation-supination, and radioulnar deviation with axial loading to assess stability and pain.
 Painful crepitus with pronation and supination indicate DRU joint arthritis that can be accentuated with manual compression of the joint.
Painful crepitus with pronation and supination indicate DRU joint arthritis that can be accentuated with manual compression of the joint.
 Dorsal wrist swelling can indicate extensor tendon synovitis. Palpation of the inflamed wrist is painful, and wrist mobility may be limited.
Dorsal wrist swelling can indicate extensor tendon synovitis. Palpation of the inflamed wrist is painful, and wrist mobility may be limited.
 Caput ulna syndrome is diagnosed as dorsal prominence of the ulnar head with accompanying ulnopalmar subluxation and supination of the carpus. The DRU joint will be swollen and painful on palpation. There may be painful limitation of pronation and supination.
Caput ulna syndrome is diagnosed as dorsal prominence of the ulnar head with accompanying ulnopalmar subluxation and supination of the carpus. The DRU joint will be swollen and painful on palpation. There may be painful limitation of pronation and supination.
 ECU subluxation and tendonitis should be distinguished from DRU joint arthritis by noting ECU subluxation with supination and ulnar deviation.
ECU subluxation and tendonitis should be distinguished from DRU joint arthritis by noting ECU subluxation with supination and ulnar deviation.
 Lunotriquetral (LT) instability from ligamentous tears should be distinguished from DRU joint arthritis by performing the LT shear test. The lunate is stabilized between the examiner’s thumb and index finger, and the triquetrum is sheared against the lunate in a dorsopalmar direction with the examiner’s other hand.
Lunotriquetral (LT) instability from ligamentous tears should be distinguished from DRU joint arthritis by performing the LT shear test. The lunate is stabilized between the examiner’s thumb and index finger, and the triquetrum is sheared against the lunate in a dorsopalmar direction with the examiner’s other hand.
 The prominent caput ulna can cause extensor tendon ruptures, primarily at the fourth and fifth extensor compartments.
The prominent caput ulna can cause extensor tendon ruptures, primarily at the fourth and fifth extensor compartments.
Imaging
 Standard three views of the wrist are useful to assess extent of arthritis and wrist stability. Changes associated with arthritis include osteophytes, joint space narrowing, erosive changes, cystic lesions, and disuse osteopenia (Fig. 83-1).
Standard three views of the wrist are useful to assess extent of arthritis and wrist stability. Changes associated with arthritis include osteophytes, joint space narrowing, erosive changes, cystic lesions, and disuse osteopenia (Fig. 83-1).
 For differentiation of extensor tendon from joint synovitis, ultrasonography is the diagnostic tool of choice.
For differentiation of extensor tendon from joint synovitis, ultrasonography is the diagnostic tool of choice.
 Computed tomography and magnetic resonance imaging are typically not necessary in the evaluation of the DRU joint in rheumatoid arthritis.
Computed tomography and magnetic resonance imaging are typically not necessary in the evaluation of the DRU joint in rheumatoid arthritis.
Surgical Anatomy
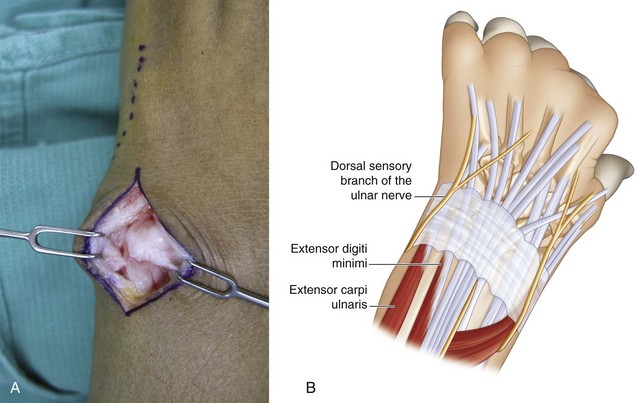
 The dorsal sensory branch of the ulnar nerve lies in the subcutaneous tissue of the dorsal ulnar wrist.
The dorsal sensory branch of the ulnar nerve lies in the subcutaneous tissue of the dorsal ulnar wrist.
 In the presence of caput ulna syndrome, the sixth dorsal compartment with the ECU is subluxed palmarly. The fifth dorsal compartment with the extensor digiti minimi (EDM) crosses the ulnar head.
In the presence of caput ulna syndrome, the sixth dorsal compartment with the ECU is subluxed palmarly. The fifth dorsal compartment with the extensor digiti minimi (EDM) crosses the ulnar head.
 The pronator quadratus originates at the distal radius and inserts on the distal ulna and is an important dynamic stabilizer of the distal ulna. The distal ulna should be excised to the level of the sigmoid notch to preserve the attachments of the pronator quadratus on the distal ulna.
The pronator quadratus originates at the distal radius and inserts on the distal ulna and is an important dynamic stabilizer of the distal ulna. The distal ulna should be excised to the level of the sigmoid notch to preserve the attachments of the pronator quadratus on the distal ulna.
Exposures
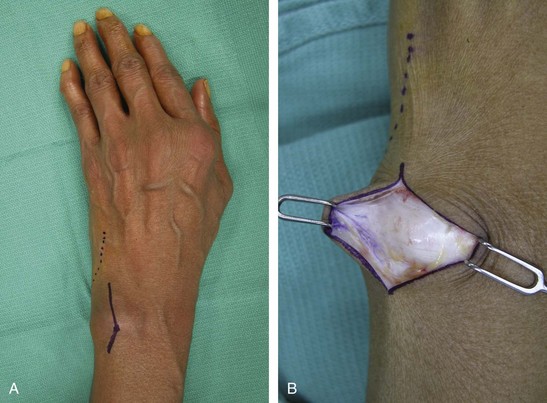
 A dorsal longitudinal incision over the distal ulna with a zigzag at the wrist is used for wide exposure to the level of the extensor retinaculum (Fig. 83-2A and B).
A dorsal longitudinal incision over the distal ulna with a zigzag at the wrist is used for wide exposure to the level of the extensor retinaculum (Fig. 83-2A and B).
 Approach the ulna between the EDM and ECU and incise the periosteum to raise radial and ulnar periosteal flaps for later closure (Fig. 83-3A and B).
Approach the ulna between the EDM and ECU and incise the periosteum to raise radial and ulnar periosteal flaps for later closure (Fig. 83-3A and B).
Procedure
Step 1
Step 2
Step 3
 The dorsal wrist capsule is imbricated with 2-0 or 3-0 braided permanent horizontal mattress sutures with the wrist fully supinated, taking care to note that the ulna is not dorsally prominent in this position (Fig. 83-6). If the distal ulna stump is unstable with pronation-supination, an ulna-stabilizing procedure can be performed using a distally based ulnar half ECU tenodesis to correct prominence of the ulnar stump. This is performed as follows:
The dorsal wrist capsule is imbricated with 2-0 or 3-0 braided permanent horizontal mattress sutures with the wrist fully supinated, taking care to note that the ulna is not dorsally prominent in this position (Fig. 83-6). If the distal ulna stump is unstable with pronation-supination, an ulna-stabilizing procedure can be performed using a distally based ulnar half ECU tenodesis to correct prominence of the ulnar stump. This is performed as follows:
 The tourniquet is released, and all bleeding points are cauterized.
The tourniquet is released, and all bleeding points are cauterized.
 The skin is closed with 3-0 absorbable monofilament dermal sutures and 4-0 absorbable monofilament running subcuticular suture.
The skin is closed with 3-0 absorbable monofilament dermal sutures and 4-0 absorbable monofilament running subcuticular suture.
Postoperative Care and Expected Outcomes
 The wrist is immobilized in a sugar tong splint with the forearm fully supinated for 4 weeks, keeping the fingers free for movement.
The wrist is immobilized in a sugar tong splint with the forearm fully supinated for 4 weeks, keeping the fingers free for movement.
 Gentle active range of motion is begun at 4 weeks. If an ulnar stump–stabilizing procedure has been performed, pronation and supination should be limited until 6 weeks postoperatively.
Gentle active range of motion is begun at 4 weeks. If an ulnar stump–stabilizing procedure has been performed, pronation and supination should be limited until 6 weeks postoperatively.
 The patient should be expected to return to full activities as tolerated at 6 to 8 weeks.
The patient should be expected to return to full activities as tolerated at 6 to 8 weeks.
De Witte PB, Wijffels M, Jupiter JB, Ring D. The Darrach procedure for post-traumatic reconstruction. Acta Orthop Belg. 2009;75:316-322.
George MS, Kiefhaber TR, Stern PJ. The Sauve-Kapandji procedure and the Darrach procedure for distal radio-ulnar joint dysfunction after Colles’ fracture. J Hand Surg [Br]. 2004;29:608-613.
Minami A, Iwasaki N, Ishikawa J, et al. Treatments of osteoarthritis of the distal radioulnar joint: long-term results of three procedures. Hand Surg. 2005;10:243-248.