Procedure 82 Radioulnar Ligament Reconstruction for Chronic Distal Radioulnar Joint Instability
![]() See Video 60: Reconstruction for Chronic Volar Subluxation of the Ulna
See Video 60: Reconstruction for Chronic Volar Subluxation of the Ulna
See Video 61: Distal Radioulnar Joint Ligament Reconstruction for Ligamentous Instability
Examination/Imaging
Clinical Examination
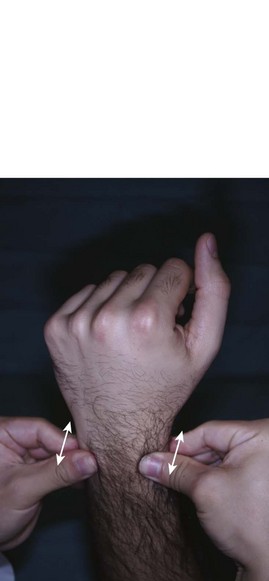
 DRU joint instability may coexist with other causes of ulnar-sided wrist pain. These include extensor carpi ulnaris (ECU) tendinitis, flexor carpi ulnaris (FCU) tendonitis, ECU subluxation, ulnar impaction syndrome, lunotriquetral (LT) instability, and pisotriquetral arthritis. It is important to consider these conditions before attributing the symptoms to DRU joint instability. The following clinical tests are suggestive of DRU joint instability:
DRU joint instability may coexist with other causes of ulnar-sided wrist pain. These include extensor carpi ulnaris (ECU) tendinitis, flexor carpi ulnaris (FCU) tendonitis, ECU subluxation, ulnar impaction syndrome, lunotriquetral (LT) instability, and pisotriquetral arthritis. It is important to consider these conditions before attributing the symptoms to DRU joint instability. The following clinical tests are suggestive of DRU joint instability:
 It is also important to rule out the presence of DRU joint arthritis because it represents a contraindication to ligament reconstruction. The following clinical test is useful in determining the presence of DRU joint arthritis.
It is also important to rule out the presence of DRU joint arthritis because it represents a contraindication to ligament reconstruction. The following clinical test is useful in determining the presence of DRU joint arthritis.
 The patient should be examined for the presence of the palmaris longus (PL) to be used as a tendon graft.
The patient should be examined for the presence of the palmaris longus (PL) to be used as a tendon graft.
Imaging
 A posteroanterior view radiograph may show widening of the DRU joint, and the lateral view demonstrates the ulnar head dorsal or volar to the radius (Fig. 82-4). A weighted lateral view (taken with patient holding 5 to 8 pounds of weight) can be used to demonstrate the instability that occurs only on loading (Fig. 82-5). Other indirect signs of instability include a basal ulnar styloid fracture (Fig. 82-6) and a displaced fleck fracture from the fovea.
A posteroanterior view radiograph may show widening of the DRU joint, and the lateral view demonstrates the ulnar head dorsal or volar to the radius (Fig. 82-4). A weighted lateral view (taken with patient holding 5 to 8 pounds of weight) can be used to demonstrate the instability that occurs only on loading (Fig. 82-5). Other indirect signs of instability include a basal ulnar styloid fracture (Fig. 82-6) and a displaced fleck fracture from the fovea.
 A computed tomography (CT) scan is useful in determining subtle degrees of DRU joint instability. CT scans of both wrists in identical forearm positions should be done. It is also useful in ruling out DRU joint arthritis and in assessing the comptenecy of the sigmoid notch, especially in patients with joint instability following distal radius fractures.
A computed tomography (CT) scan is useful in determining subtle degrees of DRU joint instability. CT scans of both wrists in identical forearm positions should be done. It is also useful in ruling out DRU joint arthritis and in assessing the comptenecy of the sigmoid notch, especially in patients with joint instability following distal radius fractures.
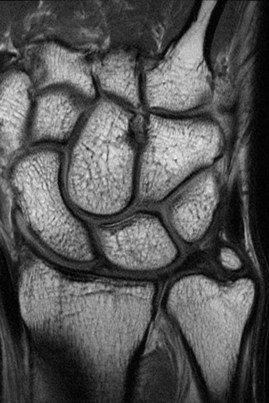
 Magnetic resonance imaging (Fig. 82-7) and arthroscopy are useful in assessment of the triangular fibrocartilage complex (TFCC) and in ruling out other causes of ulnar-sided wrist pain.
Magnetic resonance imaging (Fig. 82-7) and arthroscopy are useful in assessment of the triangular fibrocartilage complex (TFCC) and in ruling out other causes of ulnar-sided wrist pain.
Pearls
To ensure that the lateral radiograph is adequate, the index, long, and ring metacarpals; the proximal pole of the scaphoid on the lunate; and the radial styloid in the center of the lunate should all be superimposed on one another. Additionally, the palmar surface of the pisiform should be visible midway between the palmar surfaces of the distal pole of the scaphoid and the capitate (Fig. 82-8).
Surgical Anatomy
 The DRU joint is formed by the sigmoid notch of the radius and the ulnar head. It is the distal pivot for pronosupination. This joint is stabilized predominantly by ligaments, the fibrocartilaginous lips at the rim of the sigmoid notch, and the shape of the sigmoid notch in the coronal plane.
The DRU joint is formed by the sigmoid notch of the radius and the ulnar head. It is the distal pivot for pronosupination. This joint is stabilized predominantly by ligaments, the fibrocartilaginous lips at the rim of the sigmoid notch, and the shape of the sigmoid notch in the coronal plane.
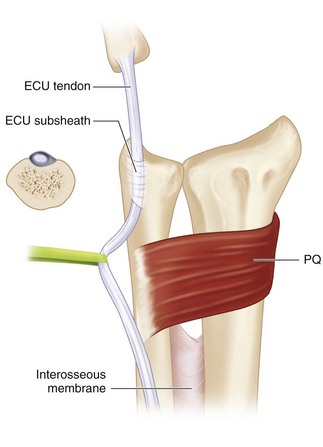
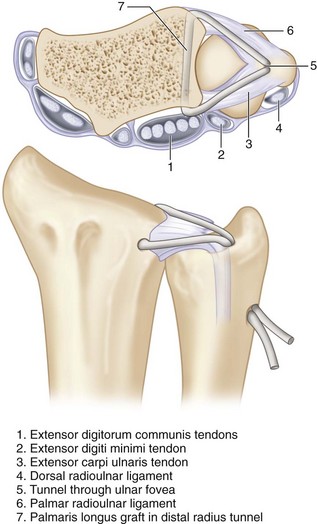
 The stabilizers of the DRU joint include the TFCC, pronator quadratus (PQ), ECU, and interosseous membrane (Fig. 82-9).
The stabilizers of the DRU joint include the TFCC, pronator quadratus (PQ), ECU, and interosseous membrane (Fig. 82-9).
 The TFCC refers to all the soft tissues that span and support the DRU joint and ulnocarpal joints. The TFCC includes the triangular fibrocartilage (TFC, or articular disk), meniscus homologue, palmar and dorsal radioulnar ligaments, ulnar collateral ligament, ulnotriquetral ligament, ulnolunate ligament, ECU subsheath, and prestyloid recess.
The TFCC refers to all the soft tissues that span and support the DRU joint and ulnocarpal joints. The TFCC includes the triangular fibrocartilage (TFC, or articular disk), meniscus homologue, palmar and dorsal radioulnar ligaments, ulnar collateral ligament, ulnotriquetral ligament, ulnolunate ligament, ECU subsheath, and prestyloid recess.
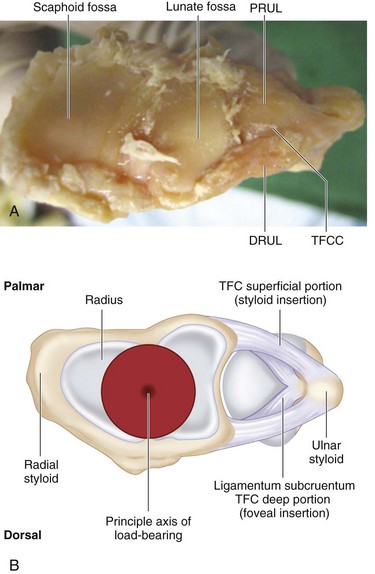
 The palmar and dorsal radiolulnar ligaments are the main stabilizers of the DRU joint. These ligaments extend from the palmar and dorsal distal margins of the sigmoid notch and converge in a triangular configuration to attach to the ulna. Each radioulnar ligament divides in the coronal plane into a deep limb that inserts into the fovea and a superficial limb that inserts into the midportion of the ulnar styloid (Fig. 82-10).
The palmar and dorsal radiolulnar ligaments are the main stabilizers of the DRU joint. These ligaments extend from the palmar and dorsal distal margins of the sigmoid notch and converge in a triangular configuration to attach to the ulna. Each radioulnar ligament divides in the coronal plane into a deep limb that inserts into the fovea and a superficial limb that inserts into the midportion of the ulnar styloid (Fig. 82-10).
Positioning
 The patient is positioned supine with the affected extremity on a hand table. The procedure is performed under tourniquet control.
The patient is positioned supine with the affected extremity on a hand table. The procedure is performed under tourniquet control.
 The arm is strapped to the arm board using a soft roll and secured with tape. The forearm is held vertical and in neutral alignment using “Chinese finger traps” similar to the position used in wrist arthroscopy. This position is maintained by a traction tower using a 5-lb weight (Fig. 82-11)
The arm is strapped to the arm board using a soft roll and secured with tape. The forearm is held vertical and in neutral alignment using “Chinese finger traps” similar to the position used in wrist arthroscopy. This position is maintained by a traction tower using a 5-lb weight (Fig. 82-11)
 Intraoperative fluoroscopy will be required, and the table should be placed such that the C-arm can be positioned with ease.
Intraoperative fluoroscopy will be required, and the table should be placed such that the C-arm can be positioned with ease.
Exposures
 A Y-shaped incision centered over the ulnar head is made on the ulnar border of the distal forearm. The vertical limb extends 5 cm proximal to the ulnar head along the ulnar border of the forearm. The volar limb extends to the pisiform, and the dorsal limb extends to the Lister tubercle (Fig. 82-12).
A Y-shaped incision centered over the ulnar head is made on the ulnar border of the distal forearm. The vertical limb extends 5 cm proximal to the ulnar head along the ulnar border of the forearm. The volar limb extends to the pisiform, and the dorsal limb extends to the Lister tubercle (Fig. 82-12).
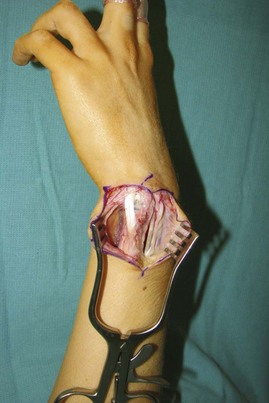
 Three skin flaps (distal, volar, and dorsal) are raised in a plane superficial to the tendons and extensor retinaculum (Fig. 82-13).
Three skin flaps (distal, volar, and dorsal) are raised in a plane superficial to the tendons and extensor retinaculum (Fig. 82-13).
Procedure
Step 1: Development of Volar Plane
 The FCU and the ulnar neurovascular bundle are identified. A plane is developed deep to these structures to expose the ulnar styloid, palmar surface of the ulnar head, and palmar rim of the sigmoid fossa (Fig. 82-14)
The FCU and the ulnar neurovascular bundle are identified. A plane is developed deep to these structures to expose the ulnar styloid, palmar surface of the ulnar head, and palmar rim of the sigmoid fossa (Fig. 82-14)
 The capsular tissue immediately radial to the ulnar styloid is divided, and subperiosteal dissection is done to expose the palmar surface of the ulnar fovea.
The capsular tissue immediately radial to the ulnar styloid is divided, and subperiosteal dissection is done to expose the palmar surface of the ulnar fovea.
Step 1 Pearls
The articular surface of the sigmoid notch and ulnar head are examined for arthritic changes. Ligament reconstruction can be performed only if there is no evidence of DRU joint arthritis. If arthritis is present, a salvage procedure, such as the Sauve-Kapandji or Darrach procedure, or a hemiresection should be considered.
Step 2: Development of Dorsal Plane
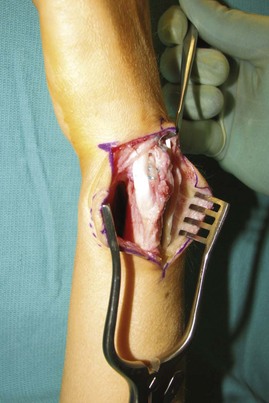
 The extensor retinaculum is divided longitudinally over the sixth compartment, and the ECU subsheath is identified. The sheath is divided along the ulnar border of the ECU, and the ECU is retracted ulnarly. This exposes the dorsal capsular tissues immediately radial to the ulnar styloid. The capsular tissue is divided longitudinally to expose the dorsal surface of the ulnar fovea (Fig. 82-15).
The extensor retinaculum is divided longitudinally over the sixth compartment, and the ECU subsheath is identified. The sheath is divided along the ulnar border of the ECU, and the ECU is retracted ulnarly. This exposes the dorsal capsular tissues immediately radial to the ulnar styloid. The capsular tissue is divided longitudinally to expose the dorsal surface of the ulnar fovea (Fig. 82-15).
 The extensor retinaculum is divided between the fourth and fifth compartments. The tendons are retracted, and the floor of this compartment is incised to expose the dorsal rim of the sigmoid notch.
The extensor retinaculum is divided between the fourth and fifth compartments. The tendons are retracted, and the floor of this compartment is incised to expose the dorsal rim of the sigmoid notch.
Step 3: Harvest of Palmaris Longus Tendon Graft
 A PL tendon graft is harvested by three separate 1-cm transverse incisions in the forearm (Fig. 82-16).
A PL tendon graft is harvested by three separate 1-cm transverse incisions in the forearm (Fig. 82-16).
Step 4: Creation of Bone Tunnel in the Radius
 A K-wire is passed about 1 cm from volar edge of the sigmoid fossa to a similar position on the dorsal edge of the sigmoid fossa. This is done under fluoroscopic guidance to ensure that the wire is not within the radiocarpal or the radioulnar joints.
A K-wire is passed about 1 cm from volar edge of the sigmoid fossa to a similar position on the dorsal edge of the sigmoid fossa. This is done under fluoroscopic guidance to ensure that the wire is not within the radiocarpal or the radioulnar joints.
 A 2.3- to 3-mm cannulated drill is passed over the K-wire to make a bone tunnel within the radius, and the K-wire is removed.
A 2.3- to 3-mm cannulated drill is passed over the K-wire to make a bone tunnel within the radius, and the K-wire is removed.
Step 4 Pearls
The tunnel should be made at a sufficient distance (1 cm) from both the distal and the ulnar articular surface of the radius to avoid a fracture of the bone during creation of the tunnel or passage of the tendon graft.
It is better to make the tunnel from volar to dorsal because the entry point can be controlled and inadvertent injury to the median nerve prevented.
Step 5: Passage of Tendon Graft
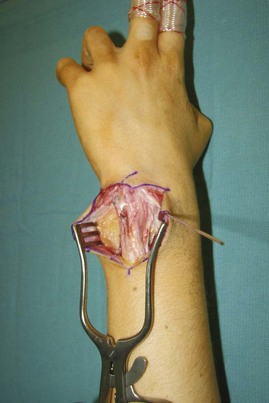
 A 25-gauge stainless steel wire loop is fashioned and passed from dorsum to the volar surface through the bone tunnel in the radius. One end of the PL tendon graft is fixed to the wire by twisting the loop. The wire is pulled back to bring the tendon out of the dorsal portion of the tunnel (Fig. 82-17).
A 25-gauge stainless steel wire loop is fashioned and passed from dorsum to the volar surface through the bone tunnel in the radius. One end of the PL tendon graft is fixed to the wire by twisting the loop. The wire is pulled back to bring the tendon out of the dorsal portion of the tunnel (Fig. 82-17).
 A pointed tendon passer is passed from the previously exposed dorsal surface of the fovea, through any remnants of the dorsal radioulnar ligament, deep to the extensor tendons to emerge at the dorsal portion of the tunnel in the distal radius. This grabs the tendon graft and brings it out at the fovea. Similarly, the tendon passer is passed from the palmar surface of the fovea, through any remnants of the palmar radioulnar ligament, deep to the flexor tendons to bring the palmar end of the tendon graft to the fovea.
A pointed tendon passer is passed from the previously exposed dorsal surface of the fovea, through any remnants of the dorsal radioulnar ligament, deep to the extensor tendons to emerge at the dorsal portion of the tunnel in the distal radius. This grabs the tendon graft and brings it out at the fovea. Similarly, the tendon passer is passed from the palmar surface of the fovea, through any remnants of the palmar radioulnar ligament, deep to the flexor tendons to bring the palmar end of the tendon graft to the fovea.
Step 5 Pearls
Moistening the tendon graft will prevent it from desiccating and make passage through the bone tunnels easier.
A hemostat should be attached to the free end of the tendon graft before pulling on the wire loop to pass the tendon through the bone tunnel in the radius. This will prevent the entire tendon from coming out through the bone tunnel.
Step 6: Creation of Bone Tunnel in Ulna
 A K-wire is passed obliquely from the fovea to exit at the ulnar border of the ulna about 1.5 cm proximal. The position of the wire is confirmed by intraoperative fluoroscopy. A 2.3- to 3-mm cannulated drill is passed over the above K-wire to make a bone tunnel within the ulna, and the K-wire is removed (Fig. 82-18).
A K-wire is passed obliquely from the fovea to exit at the ulnar border of the ulna about 1.5 cm proximal. The position of the wire is confirmed by intraoperative fluoroscopy. A 2.3- to 3-mm cannulated drill is passed over the above K-wire to make a bone tunnel within the ulna, and the K-wire is removed (Fig. 82-18).
 The ulnar tunnel needs to be wider compared with the distal radius tunnel because both ends of the tendon graft need to pass through it. If the diameter of the ulna seems narrow, the senior author prefers not to make a bone tunnel in the ulna to avoid the risk for a fracture. In such cases, the author anchors the ends of the tendon graft to the fovea and the ulna using bone anchors.
The ulnar tunnel needs to be wider compared with the distal radius tunnel because both ends of the tendon graft need to pass through it. If the diameter of the ulna seems narrow, the senior author prefers not to make a bone tunnel in the ulna to avoid the risk for a fracture. In such cases, the author anchors the ends of the tendon graft to the fovea and the ulna using bone anchors.
Step 7: Passage of Tendon Graft through Ulna
 Both ends of the tendon graft are passed through the bone tunnel in the ulna using a 25-gauge stainless steel wire loop as described previously. The wire loop is passed from outside-in to emerge at the fovea, both tendon ends are grasped, and the wire is pulled out to bring the tendon ends at ulnar border of the ulna.
Both ends of the tendon graft are passed through the bone tunnel in the ulna using a 25-gauge stainless steel wire loop as described previously. The wire loop is passed from outside-in to emerge at the fovea, both tendon ends are grasped, and the wire is pulled out to bring the tendon ends at ulnar border of the ulna.
 This step can be omitted, if a bone tunnel has been not been made in the ulna.
This step can be omitted, if a bone tunnel has been not been made in the ulna.
Step 8: Reduction and Pinning of DRU Joint
 The forearm is held in neutral rotation, the ulnar head is reduced into the sigmoid fossa, and the reduction is maintained with one or two 0.045-inch K-wires passed from the ulna to the radius about 4 to 5 cm proximal to the ulnar styloid.
The forearm is held in neutral rotation, the ulnar head is reduced into the sigmoid fossa, and the reduction is maintained with one or two 0.045-inch K-wires passed from the ulna to the radius about 4 to 5 cm proximal to the ulnar styloid.
 The position of the wires is confirmed by intraoperative fluoroscopy (Figs. 82-19 and 82-20).
The position of the wires is confirmed by intraoperative fluoroscopy (Figs. 82-19 and 82-20).
Step 9: Suture Fixation of Reconstructed Ligaments
 If both ends of the tendon graft are passed through a bone tunnel in the ulna, they are looped around the shaft of the ulna and sutured to each other, and a bone anchor placed proximal to the ulnar exit hole, as tightly as possible.
If both ends of the tendon graft are passed through a bone tunnel in the ulna, they are looped around the shaft of the ulna and sutured to each other, and a bone anchor placed proximal to the ulnar exit hole, as tightly as possible.
 If an ulnar bone tunnel has not been used, two or more bone anchors are passed at the fovea and on either side of the ulnar styloid. The tendon graft is looped around the shaft of the ulna and sutured to each other and to the bone anchors as tightly as possible (Fig. 82-21).
If an ulnar bone tunnel has not been used, two or more bone anchors are passed at the fovea and on either side of the ulnar styloid. The tendon graft is looped around the shaft of the ulna and sutured to each other and to the bone anchors as tightly as possible (Fig. 82-21).
Step 10: Closure
 The ECU sheath is reapproximated over the DRU joint, and the sheath is then closed using nonabsorbable, braided sutures.
The ECU sheath is reapproximated over the DRU joint, and the sheath is then closed using nonabsorbable, braided sutures.
 The extensor retinaculum is closed with absorbable suture. The tourniquet is released and hemostasis secured.
The extensor retinaculum is closed with absorbable suture. The tourniquet is released and hemostasis secured.
 The subcutaneous tissue and skin are closed in layers (Fig. 82-22).
The subcutaneous tissue and skin are closed in layers (Fig. 82-22).
 A sugar tong splint is provided to keep the forearm and wrist in neutral position.
A sugar tong splint is provided to keep the forearm and wrist in neutral position.
Postoperative Care and Expected Outcomes
 The wound is inspected 2 weeks after surgery, and all sutures are removed. A thermoplastic Muenster-type splint that keeps the forearm and wrist in neutral position is provided. The patient is allowed active finger motion only.
The wound is inspected 2 weeks after surgery, and all sutures are removed. A thermoplastic Muenster-type splint that keeps the forearm and wrist in neutral position is provided. The patient is allowed active finger motion only.
 At 6 weeks the K-wires are removed, and the patient is encouraged to start wrist flexion and extension exercises, but pronation and supination are restricted for another 2 weeks. The splint is discontinued after 8 weeks, and gentle pronation and supination range-of-motion and strengthening exercises are initiated.
At 6 weeks the K-wires are removed, and the patient is encouraged to start wrist flexion and extension exercises, but pronation and supination are restricted for another 2 weeks. The splint is discontinued after 8 weeks, and gentle pronation and supination range-of-motion and strengthening exercises are initiated.
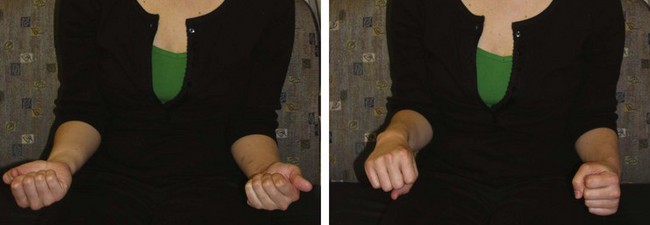
 Up to 80% to 90% of patients have reported resolution of pain and restoration of DRU joint stability after ligament reconstruction. However, an average of 10 to 20 degrees of pronation and supination range of motion is lost (Figs. 82-23 and 82-24).
Up to 80% to 90% of patients have reported resolution of pain and restoration of DRU joint stability after ligament reconstruction. However, an average of 10 to 20 degrees of pronation and supination range of motion is lost (Figs. 82-23 and 82-24).
Adams BD, Berger RA. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg [Am]. 2002;27:243-251.
Gofton WT, Gordon KD, Dunning CE, et al. Comparison of distal radioulnar joint reconstructions using an active joint motion simulator. J Hand Surg [Am]. 2005;30:733-742.
Teoh LC, Yam AKT. Anatomic reconstruction of the distal radioulnar ligaments: long-term results. J Hand Surg [Br]. 2005;30:185-193.