CASE 81

History: A 34-year-old man with chronic diarrhea presents acutely unwell with abdominal distention, fever, rectal bleeding, and passage of clots.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in the figures? (Choose all that apply.)
2. What measurement is used to indicate the seriousness of toxic megacolon?
3. What is the pathogenesis for the development of toxic megacolon?
A. Severe electrolyte imbalance
B. Failure of cholinergic neurotransmission
C. Transmural inflammation damaging the ganglion cells
D. Dilation due to mechanical failure of downstream passage of colonic contents
4. Which of the following correctly describes the thumbprinting sign?
A. Reticular mucosal pattern similar to the fine lines of a thumbprint or fingerprint
B. Thickened valvulae resembling fingers or thumbs standing close together
C. Lobules of edematous mucosa separated by lines of ulceration
D. Lobulated thickening of haustral folds
ANSWERS
CASE 81
Toxic Megacolon
1. A, B, D, and E
2. D
3. C
4. D
References
Imbriaco M, Balthazar EJ. Toxic megacolon: role of CT in evaluation and detection of complications. Clin Imaging. 2001;25(5):349–354.
Sheikh RA, Yasmeen S, Prindiville T. Toxic megacolon: a review. JK Practitioner. 2003;10:176–178.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 312.
Comment
Toxic megacolon is a relatively uncommon complication of colitis but is one of the most life-threatening. Its incidence varies, but it probably affects less than 10% of ulcerative colitis patients. It has also been described in Crohn’s disease, pseudomembranous colitis, ischemia, and infectious colitis (particularly in AIDS patients).
Toxic megacolon occurs when there is severe transmural inflammation extending into the muscularis propria. There is accompanying vasculitis of the arterioles and destruction of the ganglion cells in the myenteric plexuses. Inflammation can extend all the way to the serosa, producing peritoneal inflammation and clinical changes of peritonitis, even without perforation. The bowel wall becomes quite thin because the mucosa and submucosa are often sloughed as a result of the inflammation. An associated loss of muscle tone is caused by the inflammation of the muscle layers and the destruction of ganglion cells. Adding to this problem are the effects of the narcotic drugs and steroids that may be given to the patient for treatment, as well as possible electrolyte disturbances. These problems all lead to an atony of the bowel, with subsequent dilation.
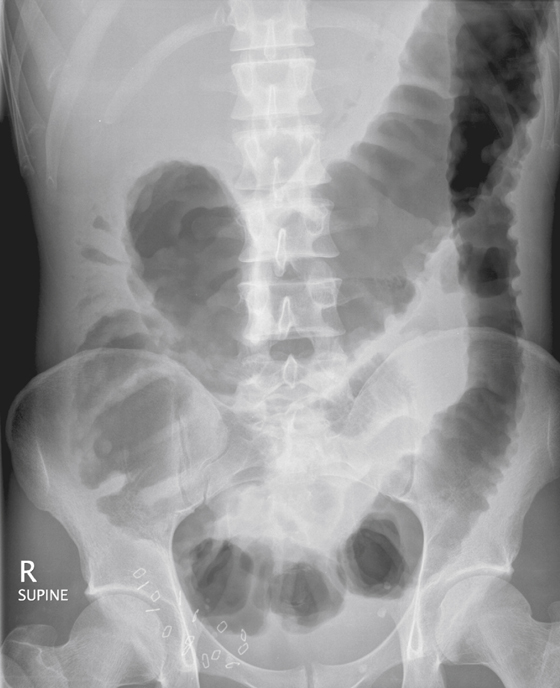
Some authors have stated that a transverse colon exceeding 8 cm is an indication of impending megacolon. The transverse colon usually dilates the most because it is in the least dependent portion of the colon, and air accumulates in it. However, other parts of the colon may be involved as well. It may be better to disregard measurements because a large colon may be present without severe disease, and perforation can occur without significant dilation.
Perforation is the most serious complication, with an associated high mortality rate. Often it is clinically occult because the high-dose steroids used to treat toxic megacolon mask the symptoms of peritonitis, which accompanies the perforation. The diagnosis can be made only on plain abdominal radiographs or CT scans (see figures). Patients who are successfully medically treated for toxic megacolon still do poorly in the future and are often at risk for recurrence or require colectomy at a later date.







