CHAPTER 80
Total Knee Replacement
Definition
Arthroplasty involves the reconstruction by natural modification or artificial replacement of a diseased, damaged, or ankylosed joint. The knee joint functions as a complex hinge, allowing flexion, extension, rotation, and gliding. The knee joint itself is made up of three compartments, lateral, medial, and patellofemoral. Disease processes that cause damage to the cartilage of any or all of the three compartments may lead to the need for total knee arthroplasty (TKA). Examples of these diseases include osteoarthritis (idiopathic or traumatic), inflammatory arthritis (e.g., rheumatoid, psoriatic), avascular necrosis, tumors, and congenital abnormalities. The principal diagnoses most commonly associated with total knee replacement procedures are osteoarthrosis and allied disorders (90.9%), followed by rheumatoid arthritis and other inflammatory polyarthropathies (3.4%) [1].
TKA is a procedure that is widely performed for advanced arthropathies of the knee; it consistently alleviates pain, improves function, and enhances quality of life [2]. As the elderly population in the United States grows and indications for the procedure broaden, it is projected that an increasing number of patients will undergo TKA. The most common age group for total knee replacements is 65 to 84 years. Women in this age range are more likely to undergo TKA than are their male counterparts.
Approximately 700,000 TKAs are performed annually in the United States. With the aging of the U.S. population, this number is projected to increase to more than 3 million yearly by 2030 [3]. Younger and more active patients are electing to proceed with TKA.
TKA consists of resection of abnormal articular surfaces of the knee with resurfacing predominantly using metal and polyethylene components. The surgical use of a total condylar prosthesis (replaces all three compartments of the knee) dates to the early 1970s. There are three basic types of TKA: totally constrained, semiconstrained, and totally unconstrained. The amount of constraint built into an artificial joint reflects the amount of stability the hardware provides. As such, a totally constrained joint has the femoral portion physically attached to the tibial component and requires no ligamentous or soft tissue support. The semiconstrained TKA has two separate components that glide on each other, but the physical characteristics of the tibial component prevent excessive femoral glide. The totally unconstrained device relies completely on the body’s ligaments and soft tissues to maintain the stability of the joint. The semiconstrained and totally unconstrained knee implants are most often used. In general, the totally unconstrained implants afford the most normal range of motion and gait.
In unicompartmental knee arthroplasty, only the joint surfaces on one side of the knee (usually the medial compartment) are replaced. Unicompartmental knee arthroplasty provides better relief than does a tibial osteotomy and greater range of motion than does a TKA as well as improved ambulation velocity. More recently, the concept of minimally invasive TKA has evolved from the procedures and investigations of unicompartmental knee arthroplasty. The distinctive features include decreased skin incision length, inferior and superior patellar capsular releases (necessary to gain exposure of the entire joint and to mobilize the patella), lack of patellar eversion (reducing risk of permanent dysfunction of the quadriceps muscle), and no tibiofemoral joint dislocation (minimizing capsular damage and postoperative pain).
The need for longer lasting TKAs continues, given the more active and anticipated longer living patient population. Efforts to design a better, longer lasting knee are focusing on alternative bearings and surfaces to reduce osteolysis. Areas being studied include the use of cross-linked ultrahigh-molecular-weight polyethylene inserts, alternative metal and ceramic bearing surfaces, and different mobile bearing designs. The goals of new designs are to minimize wear debris and to decrease risk of loosening and implant failure. The most important determinant of TKA long-lasting success remains a well-balanced, well-aligned, and well-fixed implantation procedure [4].
The increasing use of TKA has raised several public and clinical policy issues, including apparent racial and ethnic disparities in TKA use [5], broadening indications for TKA to include younger and older patients, and evidence that outcomes are better when TKA is performed in higher volume centers [6]. These issues were partially addressed in the Agency for Healthcare Research and Quality report [7]. That report concluded that there is no evidence that age, gender, or obesity is a strong predictor of functional outcomes. Patients with rheumatoid arthritis show more improvement than those with osteoarthritis, but this may be related to their poorer functional scores at the time of treatment and hence the potential for more improvement. The underlying indication, though, is consistent across all these groups, namely, that advanced osteoarthrosis of the knee compromises functional activities as the patient’s knee pain becomes recalcitrant and unresponsive to conservative therapeutic interventions. Absolute contraindications to TKA include knee sepsis or other source of ongoing infection, extensor mechanism dysfunction, severe vascular disease, recurvatum deformity due to muscle weakness, and presence of a well-functioning knee arthrodesis. Relative contraindications may include neuropathic joint, morbid obesity, past history of osteomyelitis around the knee, and skin conditions such as psoriasis within the field of surgery [8].
Symptoms
Refractory knee pain is the most common symptom among patients who undergo TKA. Stiffness, deformity, and instability are symptoms also commonly seen in advanced osteoarthrosis or inflammatory polyarthropathy. In the postoperative period, acute surgical pain is most intense during the first 2 weeks. Disruption and inflammation of the periarticular soft tissues are manifested as a soft tissue stiffness pattern that differs in the severity of limitation of range of motion from the preoperative rigid stiffness of advanced arthrosis. Joint proprioception impairment may give rise to a sense of mild knee instability in the postoperative period. Uncommonly, debris may generate a sense of cracking, popping, or locking.
Physical Examination
Physical examination should include palpation of the knee to evaluate for effusion and joint line tenderness, which may indicate meniscal disease. Gait pattern should be documented with attention to the possible presence of knee thrust (abnormal medial or lateral movement of the knee), which may indicate ligamentous instability. Preoperative knee range of motion should be recorded to assess the extensor mechanism. Because of the importance of preserving the medial and lateral collateral ligaments during a total knee replacement, preoperative assessment of the stability of these ligaments is indicated. The skin over both legs should be assessed for signs of vascular disease or infection. The lower back and hip should be examined to rule out referred pain to the knee [9].
Functional Limitations
Osteoarthritis of the knee can result in pain or stiffness that can affect a person’s functional ability to rise from a chair, to walk, or to use stairs. Table 80.1 depicts the required knee range of motion for specific functional mobility tasks. In an otherwise healthy patient population, osteoarthritis may impede participation in recreational or sporting activities, such as golf or tennis. The preoperative profile of a patient at risk for poor postoperative locomotor recovery is a woman with a high body mass index, many comorbidities, high intensity of knee pain, restriction in flexion amplitude, deficits in knee strength, and poor preoperative locomotor ability as measured by the 6-minute gait test. In addition, the preoperative gait power profiles, on the nonsurgical side, are characterized by low concentric push-off work by the plantar flexors and low concentric action of the hip flexors during early swing [10]. Postoperative pain scores and their associated psychological profiles ostensibly affect functional outcomes also [11].
Table 80.1
Required Knee Range of Motion
| Activity of Daily Living | Extension-Flexion |
| Walking in stance phase | 15-40 degrees |
| Walking in swing phase | 15-70 degrees |
| Stair climbing step over step | 0-83 degrees |
| Standing up from a chair | 0-93 degrees |
| Standing up from a toilet | 0-105 degrees |
| Stooping to lift an object | 0-117 degrees |
| Tying a shoelace | 0-106 degrees |
Modified from Kaplan RJ. Total knee replacement. In Frontera WR, ed. Essentials of Physical Medicine and Rehabilitation, 2nd ed. Philadelphia, WB Saunders, 2008.
Subsequent studies have further identified factors associated with a suboptimal postoperative functional outcome. Patients who have marked functional limitation, severe pain, low mental health score, and other comorbid conditions before TKA are more likely to have a worse outcome at 1 year and 2 years postoperatively [12]. One consistent finding is that preoperative joint function is a predictor of function at 6 months after TKA. Those patients who had lower preoperative functional status related to knee arthritis functioned at a lower level at 6 months than did patients with a higher preoperative functional status [13]. Studies have focused on quadriceps strength as a significant contributing factor. Functional measures underwent an expected decline early after TKA, but recovery was more rapid than anticipated and long-term outcomes were better than previously reported in the literature in patients with higher baseline quadriceps strength. The high correlation between quadriceps strength and functional performance suggests that emphasis on postoperative quadriceps strengthening is important to enhance the potential benefits of TKA [14]. However, preoperative quadriceps strength training has not been proved to enhance long-term functional outcome after TKA [15,16].
Diagnostic Studies
Plain radiographs of the knee remain the mainstay of diagnosis and preoperative planning. Three basic views include standing anteroposterior view (assesses medial and lateral joint space narrowing during normal leading of the joint), lateral view (assesses the patellofemoral joint and the position of the patella), and tangential patella or sunrise view (assesses the patellofemoral joint space) [9]. Magnetic resonance imaging is more sensitive than plain radiography in assessing cartilage but still may underestimate the amount of damage. Magnetic resonance imaging may also be used to evaluate meniscal or ligament disease [17].
In addition to the standard preoperative screening for surgical clearance, consideration should be given to radiographic evaluation of the cervical spine in rheumatoid arthritis patients. Rheumatoid arthritis patients are at increased risk for atlantodental instability and therefore may be at increased risk for spinal cord impingement as a result of perioperative manipulations with surgery and general anesthesia [18].
Rheumatoid arthritis patients are thought to be at 2.6-fold greater risk of infections than osteoarthritis patients are. Therefore, rheumatoid arthritis patients should be screened for potential sources of infections, including urinary tract infections, skin infections, and dental infections, before TKA. [19]
Treatment
Initial
Medical therapeutic interventions address the following.
Prophylaxis for Deep Venous Thrombosis and Pulmonary Embolism
Warfarin, a vitamin K antagonist, can be started preoperatively or postoperatively to prevent deep venous thrombosis (DVT) and pulmonary embolism (PE). The anticoagulant effects of vitamin K antagonists are not achieved until the third or fourth day of treatment. Thus, postoperative initiation of warfarin may not prevent small thrombi from forming. Nevertheless, warfarin does appear to effectively inhibit the extension of small thrombi, thereby preventing clinically significant DVT or PE. Because of its delayed reaction and its similar bleeding rates to low-molecular-weight heparin, warfarin tends to be the preferred thromboprophylactic medication by United States orthopedic surgeons [20].
New oral antithrombotic agents that inhibit either activated factor X or activated factor XI (thrombin) are now approved for use in the United States. Rivaroxaban inhibits activated factor X. The RECORD3 study demonstrated the superiority of a 10-mg once-daily oral dose of rivaroxaban over 40-mg subcutaneous daily dosing of enoxaparin in reducing the incidence of symptomatic venous thromboembolism (VTE) after total knee replacement [21]. The RECORD4 study compared rivaroxaban 10 mg orally daily with enoxaparin 30 mg subcutaneously twice daily. No statistically significant difference was shown in the incidence of major or symptomatic VTE [22].
Dabigatran etexilate is a direct thrombin inhibitor. It is active against both free and clot-bound thrombi. The RE-MOBILIZE trial compared dabigatran with enoxaparin (30 mg subcutaneously twice daily). Data for major VTE or death and major bleeding events were comparable [23]. Low-molecular-weight heparins are used in VTE prophylaxis after TKA. They have an advantage in that they can be given subcutaneously once or twice daily with constant dosing without the need for daily laboratory monitoring. They also carry a significantly reduced risk for heparin-induced thrombocytopenia compared with unfractionated heparin.
Intermittent pneumatic compression prevents venous thrombosis by increasing venous blood flow in the deep veins of the legs and by reducing plasminogen activator inhibitor [24]. Intermittent pneumatic compression is contraindicated in patients with evidence of leg ischemia due to peripheral vascular disease. The optimal use of intermittent pneumatic compression, which includes initiation in the operating room or recovery room, is an alternative option for VTE prophylaxis for patients at a high risk for bleeding. Aspirin is thought to be highly effective in reducing major arterial thrombotic events, but the benefit in reducing VTE is less clear. The 2008 American College of Chest Physicians anticoagulation guidelines recommended against use of aspirin alone as prophylaxis for VTE for any medical or surgical patient group [25]. The 2012 American College of Chest Physicians guidelines, however, have included aspirin as a recommended agent for thrombosis prophylaxis in patients undergoing TKA. This recommendation was not unanimously supported by the entire panel [26].
For patients undergoing total knee replacement, UpToDate recommends extending thrombosis prophylaxis beyond 10 days and up to 35 days after surgery [20].
Postoperative Care
During the first 48 to 72 hours, patients often receive controlled analgesia therapy administered through the intravenous or epidural route. Some anesthesiologists use a perioperative femoral nerve block. Subsequently, patients are given oral opioids. Controlled-release and short-acting opioids may be used. Depending on the clinician’s and patient’s preferences, fixed or rescue dose opioid medications are selected. The opioids can be titrated to achieve balance of analgesia versus emerging side effects [27–30].
Dry, sterile gauze dressings are applied as long as drainage is present. Staples and sutures can safely be removed 10 to 14 days after surgery [31,32]. Knee immobilizers may be used postoperatively to maintain knee extension and to avoid flexion contracture. Range of motion exercises supervised by a physical therapist should be initiated as soon as possible. Properly fitting, thigh-high elastic compression stockings, a continuous passive motion (CPM) machine, and possibly local cryotherapy are used to manage swelling [33–36].
The overall blood lost after unilateral TKA has been estimated at 2.2 units. Blood loss is greater for uncemented than for cemented prostheses. Patients are often advised before surgery to donate 1 to 3 units of packed red blood cells for autotransfusion, although this practice has recently been questioned [37]. In addition, postoperative blood collection and reinfusion through the surgical drain have been shown to be effective in reducing the need for bank blood and have a low morbidity rate with current techniques. Some patients are advised to commence a course of recombinant erythropoietin in conjunction with iron supplementation before surgery [38]. If the patient is receiving oral anticoagulation therapy, bridging therapy with a low-molecular-weight heparin compound may be considered by the patient’s primary care physician or medical consultant [39]. If the perioperative red blood cell count reveals a macrocytic anemia, vitamin B12 and folic acid levels should be obtained. If the anemia is microcytic, serum iron level, total iron-binding capacity, or transferrin concentration should be determined along with a reticulocyte count.
Rehabilitation
Because preoperative function is a strong overall predictor of postoperative function for patients undergoing TKA, researchers are examining the potential role of prehabilitation (presurgical rehabilitation) in improving patient outcomes. Programs may include strength and flexibility training as well as nutritional counseling and education. Outcomes being studied include mobility, pain, self-care function, health-related quality of life, and self-efficacy (defined as the perception of one’s ability to perform a task successfully). Although prehabilitation programs can have a positive effect on strength, function, and psychological health before surgery, it remains to be determined whether there is any significant long-term postoperative benefit [16,40].
The focus of postoperative rehabilitation should be joint range of motion, quadriceps strengthening, and training in gait and activities of daily living.
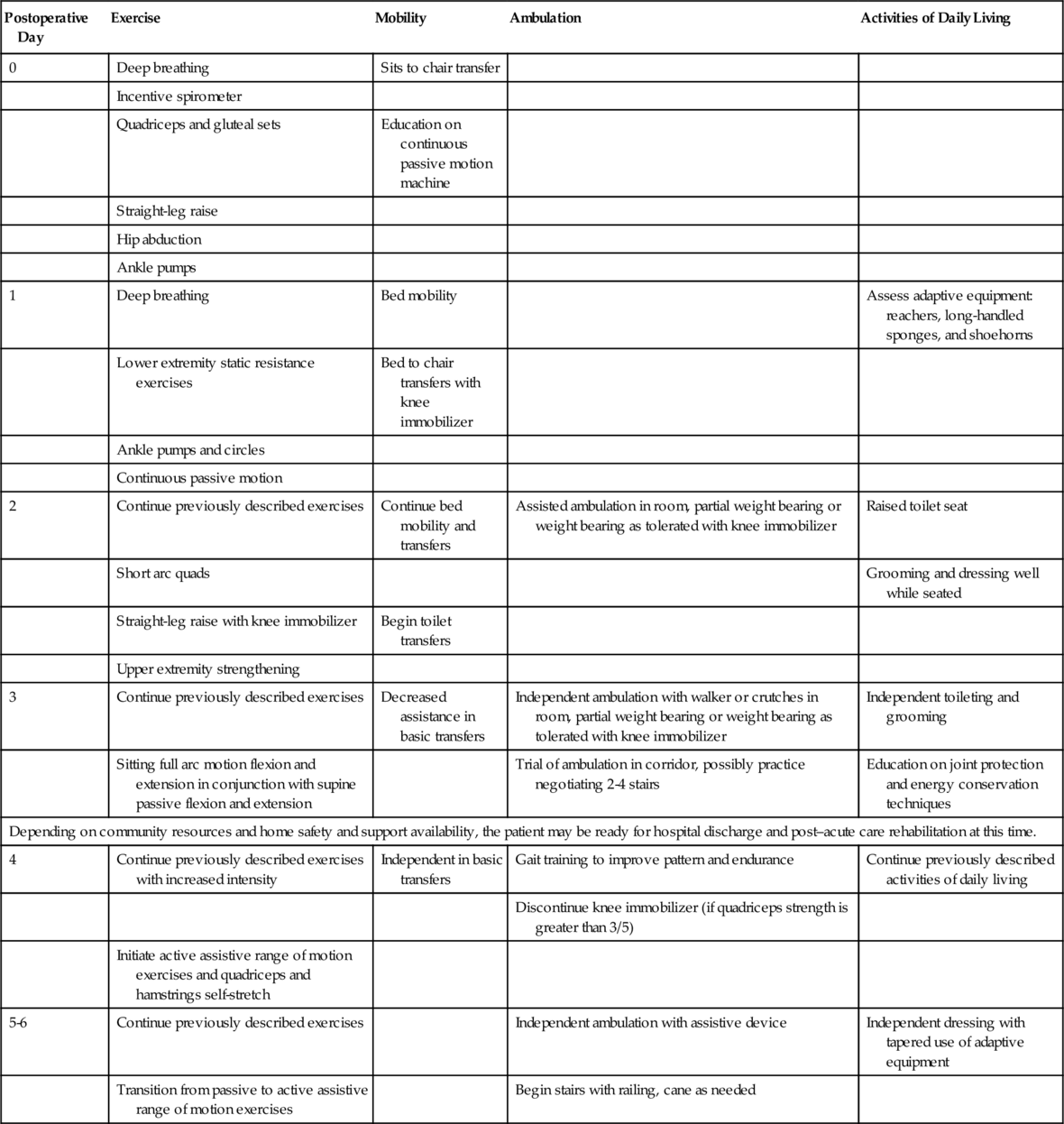
Rehabilitation programs that use clinical pathways enhance the efficiency of postoperative rehabilitation for the patient with TKA. The rehabilitation program can be conceptualized as occurring in stages or phases. The first stage commences in the immediate postoperative period. The final stage concludes when the patient returns to the community and pursues optimal independent functional living. See Table 80.2 for an example of a clinical pathway that addresses the schedule of progression during the first phase.
CPM devices may be used, but there is uncertainty whether the cost and inconvenience justify any significant clinical benefits. A 2010 meta-analysis review of 20 random trials comparing routine postoperative physical therapy and care with CPM to routine postoperative physical therapy and care without CPM showed only a small increase in range of motion (2-3 degrees) in the CPM group [41]. There is no evidence that short-term CPM application versus long-term CPM application influences outcome. There is no substantial evidence that CPM influences the degree of swelling, risk of VTE, or incidence of wound infection or incision site complications [42]. In the immediate postoperative period, the inhibited quadriceps and hamstrings may not adequately stabilize the knee. The patient may require a knee immobilizer for transfers and walking. The patient will often require a two-handed assistive device (e.g., walker or axillary crutches) for gait training initially. Adaptive equipment for bathing and dressing (e.g., tub or shower seat, grab bars, dressing sticks, sock aid) is generally necessary. Some patients may not have sufficient range of motion during the first week postoperatively to negotiate stairs. The motor reactions normalize by the third week; therefore, patients may return to driving activities if they can perform car transfers independently and can tolerate sitting for prolonged periods [43].
During the second stage of TKA rehabilitation (weeks 1 to 4), the patient progresses to low-resistance dynamic exercise for the involved lower extremity. This can be carried out with a stationary bicycle. Some patients may prefer aquatic-based exercise regimens during this period. Patients should be independent in ambulating with a two-handed or single-handed device if they are fully weight bearing on level surfaces up to 500 feet. They should be supervised in negotiating stairs. Electrical stimulation of the quadriceps can be considered for patients who have inhibited recruitment [44]. Soft tissue mobilization can be introduced to facilitate patellar glide. During this period, the patient should be independent in all basic activities of daily living. During the last 10 years, there has been a significant temporal shift in expediting home and outpatient (clinic) TKA rehabilitation. In this regard, there are no reproducible and enforceable guidelines that may be uniformly applied [45–47].
During the third stage of TKA rehabilitation (weeks 4 to 8), the available range of motion should reach 0 to 115 degrees. Patients are able to advance their dynamic resistance exercise regimens and more freely pursue both open and closed kinetic chain and dynamic balance exercises. Patients advance to a single-handed device or no device for ambulation and at different speeds and on different terrain. They should be independent in negotiating stairs. Patients advance to independence in instrumental activities of daily living.
In the final stage (weeks 8 to 12), patients may return to their preoperative exercise regimens and recreation activities and kneeling. Most patients who participated in sports before surgery are able to return to low-impact sport activities and exercise regimens. Patients are able to return to sedentary, light, and medium work categories. Patients who are on sick leave for more than 6 months preoperatively are less likely to return to work. There is published evidence that the degree of physical activity does not contribute to premature revision TKA [48]. However, younger patients may be at risk for earlier revision TKA, depending on their degree of physical activity [49]. Contact sports are advised against, and caution should be exercised with high-impact aerobic activities [50–54].
Procedures
Manipulation
Some patients with unsatisfactory gains in knee range of motion may be candidates for manipulation. The role of manipulation for the patient with a TKA contracture remains controversial. Outcome studies are divided as to whether functional outcomes and quality of life are enhanced as a result of manipulation. When an orthopedic surgeon performs the procedure, it is carried out in an operating room with the use of general or epidural anesthesia. The goal is to overcome articular lesions with minimal force after quadriceps resistance is eliminated. Manipulation is most commonly performed during the second or third postoperative week if the range of motion of the involved knee is less than 75 degrees [55,56].
Arthrocentesis
Aspiration of the knee for aerobic and anaerobic cultures and sensitivities is the most reliable method for diagnosis of infection. Strict sterile technique must be used throughout the aspiration procedure [57].
Surgery
The most common materials presently used in replacement joints are cobalt-chromium and titanium on ultrahigh-molecular- weight polyethylene. In total knee arthroplasties, cobalt-chromium is commonly used on femoral weight-bearing surfaces because of its superior strength. Total knee arthroplasties can be stabilized with or without cement. In some cases, hybrid total knee arthroplasties are used.
There are three major surgical approaches for the standard TKA: the medial parapatellar retinacular approach, the midvastus approach, and the subvastus approach [58]. The medial parapatellar retinacular approach compromises the quadriceps tendon in its medial third, and this gives rise to more postoperative patellofemoral complications. The midvastus approach does not compromise the extensor mechanism of the knee joint. The subvastus approach also preserves the integrity of the extensor mechanism but does not expose the knee as well as the other two approaches do. The type of arthrotomy used will influence postoperative management. After a standard anteromedial arthrotomy between the vastus medialis and rectus tendons with eversion of the patella, active and passive range of motion may begin immediately. Protected ambulation with crutches or a walker is recommended for 4 to 6 weeks to allow healing of the arthrotomy repair and recovery of quadriceps strength. Although recovery after the subvastus approach may be more rapid than after the standard anteromedial approach, protected weight bearing with ambulatory aids for 3 to 6 weeks is still recommended to allow soft tissue healing. In the patient with limited preoperative range of motion, either tibial tubercle osteotomy or a V-Y quadricepsplasty needs to be performed. After tibial tubercle osteotomy, early range of motion and full weight bearing within 1 week of surgery is recommended. Variations of the conventional surgical exposures are also used in the minimally invasive TKA operative approaches [59].
Weight-bearing status depends on the details of the surgical reconstruction and whether the components were inserted with or without cement. For the otherwise uncomplicated primary cemented TKA, the patient can tolerate weight bearing within the confines of safety. Protected weight bearing can be performed only after the patient demonstrates adequate control of the limb to prevent falling. The time to weight bearing after total arthroplasty depends on the use of cement or cementless fixation and whether large structural bone grafting was required. In cemented total knees, no differences in the incidence of radiolucent lines have been observed between immediate weight bearing and protected weight bearing for 12 weeks. Although weight bearing after cementless fixation might increase micromotion, many surgeons allow early weight bearing [60].
The tibial and femoral components presently in use have a life expectancy of 10 to 20 years. This life span depends on the surgical technique, the components used, the bone stock, and the level of physical activity after TKA. Revision TKA is a surgical procedure that the patient with TKA may encounter several years after the original surgery [61].
Potential Disease Complications
Potential disease complications of conditions involving the knee, such as osteoarthritis, rheumatoid arthritis, and osteonecrosis of the femoral epicondyle or tibial condyle, include intractable pain, swelling, stiffness, contracture, and valgus or varus deformity. It is recommended that TKA not be significantly delayed once it is clinically indicated. Otherwise, the delay may allow the development of soft tissue contractures and excessive muscle atrophy, which could reduce the chances of a good postoperative recovery [62].
Potential Treatment Complications
The development of DVT with the subsequent risk for fatal PE is understandably the most feared complication of TKA. Without prophylaxis, the incidence of DVT after TKA ranges from 40% to 88%, the incidence of asymptomatic PE ranges from 10% to 20%, and the incidence of symptomatic PE ranges from 0.5% to 3%, with mortality up to 2%. With prophylaxis, the incidence of symptomatic DVT and PE drops to less than 1% and 0.3%, respectively [63].
Patellofemoral complications are thought to be the most common reason for reoperation after TKA. Examples include patella instability, patella component loosening or failure, patella fracture, patella clunk syndrome, and rupture of the exterior mechanism. Patella clunk syndrome results from formation of fibrous tissue on the quadriceps tendon. The patient feels a clunk as the knee is actively extended from 60 to 30 degrees. This syndrome was more commonly seen with earlier designs of posterior cruciate substitution prostheses. With changes in component design, the incidence of patella clunk has decreased [64].
The most common neurologic complication is peroneal nerve palsy. Clinical presentation includes paresthesias and ankle dorsiflexion weakness. Incidence is less than 1%. Recovery is variable, with one study reporting up to 50% full recovery [8]. Arterial vascular injuries, the majority of which are thrombosis, are exceedingly rare.
Periprosthetic fractures may occur in the patella, around the femoral component and the tibial component. Osteoporosis and rheumatoid arthritis increase the risk for periprosthetic fractures. Femoral fractures are associated with notching of the anterior femur at time of surgery. Tibial fractures remain rare [64].
Arthrofibrosis (stiffness) is a postoperative limited range of motion that may result in decreased function. In general, 67 degrees of knee flexion is needed during the swing phase of gait, 83 degrees to ascend stairs, 100 degrees to descend stairs, 93 degrees to rise from a standard chair, and 105 degrees to rise from a low chair [65]. It remains unclear whether the use of continuous passive motion reduces the risk of arthrofibrosis.
Although infection is a serious complication, the overall infection rate for initial TKA is low at around 1% [66]. This is higher in patients with diabetes mellitus, advanced rheumatoid arthritis, revision TKA, or constrained prostheses. Deep infection can occur any time from days to months after surgery. Musculoskeletal infection usually is manifested as increase in pain with or without weight bearing, increase in swelling, and fever. Diagnosis is confirmed by joint fluid analysis, as described earlier. The patient typically requires at least a 6-week course of antibiotic treatment between the period of component removal and reimplantation. The most successful technique for treatment of the infected total knee replacement is a two-stage reimplantation of the TKA components. Infection must never be overlooked as a cause of implant loosening. Infection can occur early or late and can be manifested with or without signs of systemic toxicity. The symptoms are commonly the same as those seen with aseptic loosening. A progressive radiolucency between the prosthesis and its adjacent bone almost always is considered an infection until proved otherwise. Negative aspirate from the knee, normal sedimentation rate and C-reactive protein level, and normal gallium or indium scans cannot rule out infection of the prosthetic device. The patient should be advised that even in the presence of normal test results, infection of the prosthetic device may be discovered intraoperatively and necessitate the removal of the prosthetic device.
Metallosis is a rare but severe complication of knee replacement surgery. Metallic debris may be deposited in the periprosthetic soft tissues from abrasion of the metallic components. This metallic debris may induce a massive release of cytokines from inflammatory cells. This release may accelerate osteolysis and loosening of the prosthesis [67]. The inflammatory cells may also infiltrate the synovium, resulting in synovitis, which may be manifested as an acutely painful effusion [68]. In addition, the metallic debris may have a direct toxic effect on human marrow stroma–derived mesenchymal stem cells; it is hypothesized that decreased viability of these mesenchymal stem cells may reduce the amount of viable osteoprogenitor cells, which would be a factor in the development of poor periprosthetic bone quality. The reduction in bone quality increases the risk of implant stability, which eventually requires revision surgery [69]. Titanium components appear to have an increased association with metallosis in comparison to chromium-cobalt components [68].
The most common reason for total arthroplasty failure has been loosening of the implant. Factors associated with loosening include infection, implant constraint, failure to achieve neutral mechanical alignment, instability, and cement technique. The prodromal features of impending loosening and failure of the components are an increase in pain and swelling with or without angular deformity of the knee [70]. The radiographic features include a widening radiolucent zone between the implant and the adjacent bone and subsidence of the implant. Loosening may occur at the component-cement interface or bone-cement interface. Implant loosening can be attributed to mechanical and biologic factors. The mechanical factors include limb alignment, ligamentous balance, and preservation of a contracted posterior cruciate ligament. Implant loosening can occur early or late. Early implant loosening usually occurs within the first 2 years and represents a mechanical failure of the interlock of the implant and host to bone. This early implant loosening is more appropriately called fixation failure and is often secondary to errors in judgment at the time of surgery or to problems with the technical aspects of the surgical procedure. Extremity malalignment, soft tissue imbalance, and poor cement technique individually or in combination contribute to loosening. Biologic factors are largely responsible for the phenomenon of late loosening. Late loosening of total knee implants is often secondary to the host biologic response to the implant’s debris that weakens the mechanical bond of implant to bone established during surgery. Mechanical factors may contribute to late loosening, but they do not alone explain the loss of a fixation device that has been stable for many years. The volume of particles generated from the articulation is influenced by the patient’s weight and activity level, duration of implantation, polyethylene thickness, and contact stresses. Wear may be accelerated by malalignment, instability, and ligament imbalance, resulting in increased volume of particulate released into the joint [71]. Aseptic loosening that will lead to failure of the prosthesis occurs in 5% to 10% of patients at around 10 to 15 years after surgery. Once a component becomes loose, it becomes mechanically unstable. This can lead to increased osteolyses. If the osteolyses becomes severe, revision surgery will be difficult [8]. Thirty-day mortality for TKA is around 0.6%, with no significant differences based on race or ethnicity [9].