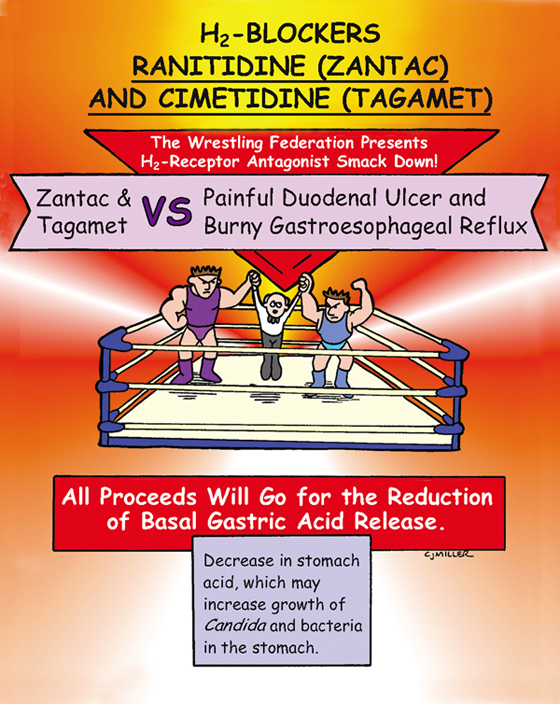
H2-Blockers
ACTIONS
Histamine H2-antagonists inhibit histamine action on H2-receptors, which are found on the gastric parietal cells. This action reduces the secretion of gastric acid, as well as hydrogen ion concentration.
USES
• Prevention and treatment of gastric and duodenal ulcers
• Heartburn, acid indigestion, and gastroesophageal reflux disease
CONTRAINDICATIONS AND PRECAUTIONS
• Hepatic and renal dysfunction
• Caution in older adult patients
SIDE EFFECTS
• Older adults: **confusion,** agitation
• Cimetidine: May bind with androgens to cause gynecomastia and impotence.
NURSING IMPLICATIONS
1. *Oral medications may be taken without regard to meals.*
2. ‡Teach patient to avoid alcohol.‡
3. ‡Smoking may decrease effectiveness.‡
4. ‡Teach patient the signs of gastric bleeding and to notify health care provider if any occur.‡
5. ‡Teach patient to notify health care provider for any indication of respiratory problems.‡
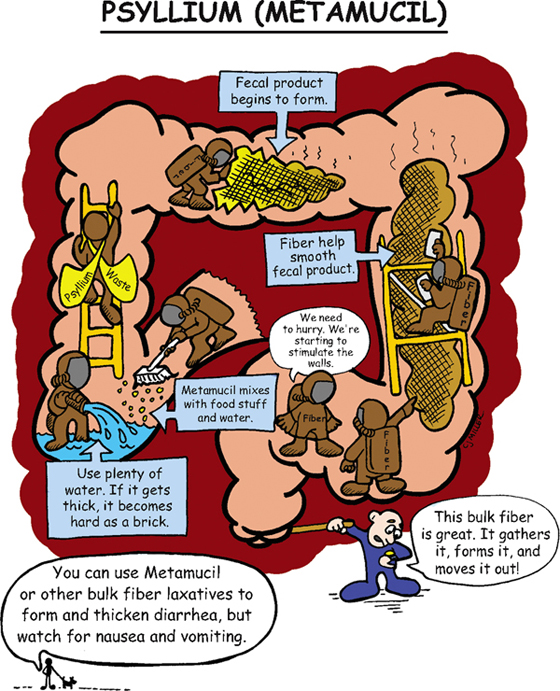
Psyllium (Metamucil)
CLASSIFICATION
Bulk-forming laxative
ACTIONS
Acts similar to dietary fiber. This medication is not digested or absorbed. After ingestion, it will swell to form a viscous solution or gel, softening the fecal mass and increasing the bulk. A fecal mass stretches the intestinal wall to stimulate peristalsis and passage of a soft-formed stool in 1 to 3 days.
USES
• Prevents constipation and straining after myocardial infarction or rectal surgery.
CONTRAINDICATIONS
• Bowel obstruction or undiagnosed acute abdominal pain
PRECAUTIONS
• Intestinal adhesions, ulcers
SIDE EFFECTS
• Impaction and obstruction if not given with adequate liquids
NURSING IMPLICATIONS
1. *Mix powder with at least 8 ounces of water; mix at the bedside immediately before administration.*
2. ‡Instruct patient to drink at least 8 ounces of water after each dose and drink at least 6 to 8 glasses of water each day to facilitate peristalsis and to prevent obstruction.‡
3. Bowel movement should occur in 12 to 36 hours.
4. *Administer at least 2 hours before or after medications.*
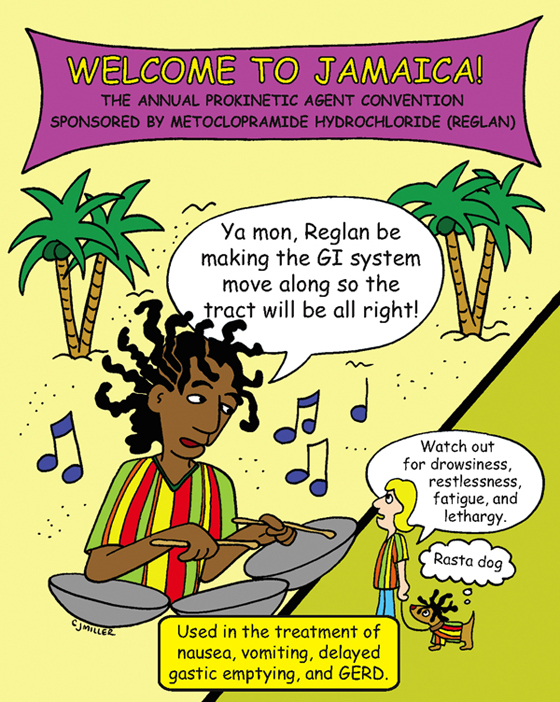
Metoclopramide Hydrochloride (Reglan)
CLASSIFICATION
Peristaltic stimulant, antiemetic
ACTIONS
Suppresses emesis by blocking dopamine receptors in the chemoreceptor trigger zone; increases tone and accelerates intestinal transit and gastric emptying by enhancing action of acetylcholine.
USES
• Provides antiemetic properties for suppressing nausea and vomiting associated with cancer therapy and postoperatively.
• Suppresses gastroparesis in patients with diabetes.
• Suppresses gastroesophageal reflux.
CONTRAINDICATIONS
• Gastrointestinal obstruction or perforation; gastrointestinal hemorrhage
• Concurrent use with medications that produce extrapyramidal reactions
PRECAUTIONS
• Impaired renal function, congestive heart failure, cirrhosis
SIDE EFFECTS
• **Drowsiness, restlessness, fatigue, lethargy**
• Dizziness, headache, insomnia, dry mouth
• †Extrapyramidal symptoms (toxic)†
NURSING IMPLICATIONS
1. Assess status of hydration.
2. *Monitor for anxiety, restlessness, extrapyramidal symptoms.*
3. Monitor pattern of bowel response.
4. Monitor for therapeutic response.
5. *To prevent nausea, administer 30 minutes before chemotherapy; give 30 minutes before meals and at bedtime for gastroparesis.*
6. Monitor renal function, blood pressure, and heart rate.
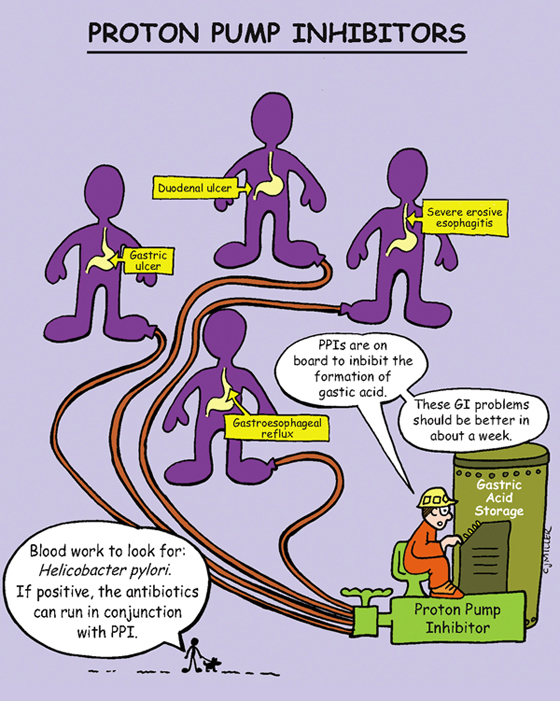
Proton Pump Inhibitors
EXAMPLES
ACTIONS
Suppress the secretion of gastric acid by combining with an enzyme on the gastric parietal cells; block the final common pathway for gastric acid formation; decrease hydrogen ion transport into the gastric lumen.
USES
• Short-term (4 to 8 weeks): Duodenal ulcers associated with Helicobacter pylori, gastric ulcers, erosive gastritis, and gastroesophageal reflux disease
• Long-term: Hypersecretory conditions (Zollinger-Ellison syndrome)
CONTRAINDICATIONS AND PRECAUTIONS
• Long-term use may predispose patient to the risk of developing gastric cancer.
• Long-term therapy may predispose patient to the risk of osteoporosis and fractures.
SIDE EFFECTS
NURSING IMPLICATIONS
1. ‡Instruct patient to avoid opening, chewing, or crushing capsules.‡
2. ‡Instruct patient to return for follow-up if symptoms are unresolved after 4 to 8 weeks of therapy.‡
3. ‡Should be taken before meals.‡
4. *Notice that the generic names end in “zole.”*
5. ‡Encourage patients to maintain adequate intake of calcium and vitamin D.‡
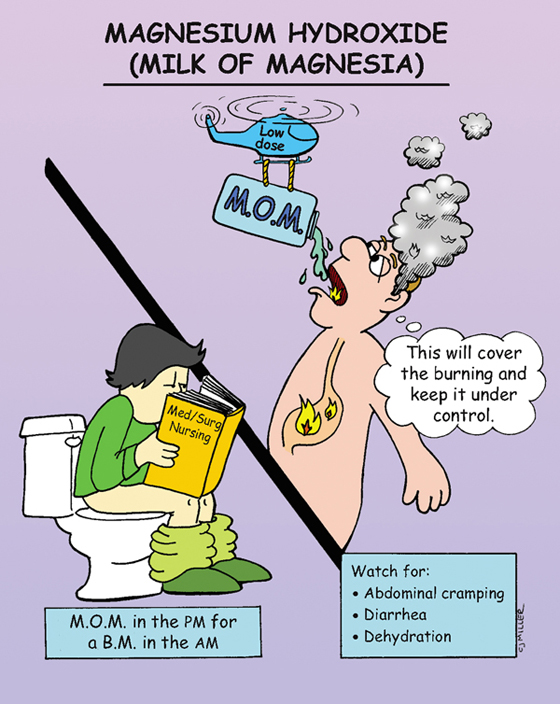
Magnesium Hydroxide (Milk of Magnesia)
CLASSIFICATION
Osmotic laxative, magnesium compound
ACTIONS
Draws water into the intestine by osmotic action on the surrounding tissue. The increase in fluid in the intestine will dilute the stool, stretch the bowel, and increase peristalsis.
USES
• Cleanse the gastrointestinal tract
• Flush ingested toxins out the gastrointestinal tract
CONTRAINDICATIONS
PRECAUTIONS
SIDE EFFECTS
• Abdominal cramping, diarrhea, dehydration
NURSING IMPLICATIONS
1. *Give with at least 8 ounces of water.*
2. *Will generally act within 6 to 12 hours.*
3. Monitor bowel movement, hydration status, and electrolytes level.
4. ‡Laxative abuse (laxative taken every day) decreases the defecatory reflex, leading to laxative dependence.‡
5. ‡Teach patient to eat foods high in fiber (brans, fruits) and increase fluid intake.‡
6. *Is commonly given with aluminum hydroxide.*
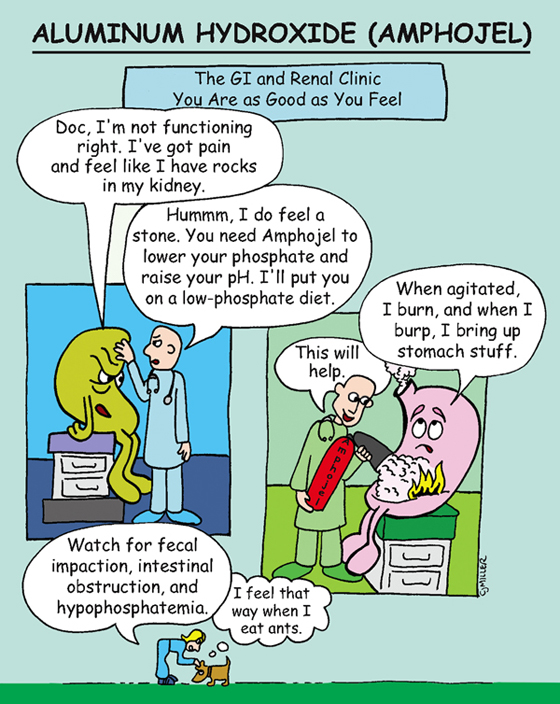
Aluminum Hydroxide (Amphojel)
CLASSIFICATION
Phosphate-binding antacid, aluminum compound
ACTIONS
Reduces acid concentration and pepsin activity by raising pH of gastric secretions. Binds with phosphate and helps prevent hyperphosphatemia. Decrease in serum phosphorous may precipitate an increase in serum calcium.
USES
• Relieves hyperacidity related to gastritis and reflux.
• Treats gastric and duodenal ulcers.
• May be used to treat hyperphosphatemia in renal insufficiency.
• Is most frequently used in combination with magnesium hydroxide.
CONTRAINDICATIONS AND PRECAUTIONS
• Dehydration or fluid restriction or both.
• Renal disease or cardiac disease or both.
• Undiagnosed abdominal pain, intestinal obstruction, chronic constipation, diarrhea.
• *May decrease excretion of anticholinergics; may decrease absorption of iron preparations, isoniazid, ketoconazole, quinolones, tetracyclines, warfarin, and digoxin.*
• Do not use in children under 6 years of age.
• *Because of its high sodium content, use with caution when combining with magnesium.*
SIDE EFFECTS
• **Constipation, abdominal cramps,** hypophosphatemia
NURSING IMPLICATIONS
1. *Monitor serum calcium, phosphate, magnesium and sodium levels.*
2. *Monitor for bone disease and neurologic impairment associated with magnesium toxicity.*
3. *Do not administer antacids to patients with a cardiac presentation who complain of dyspepsia; discomfort may be referred anginal pain.*
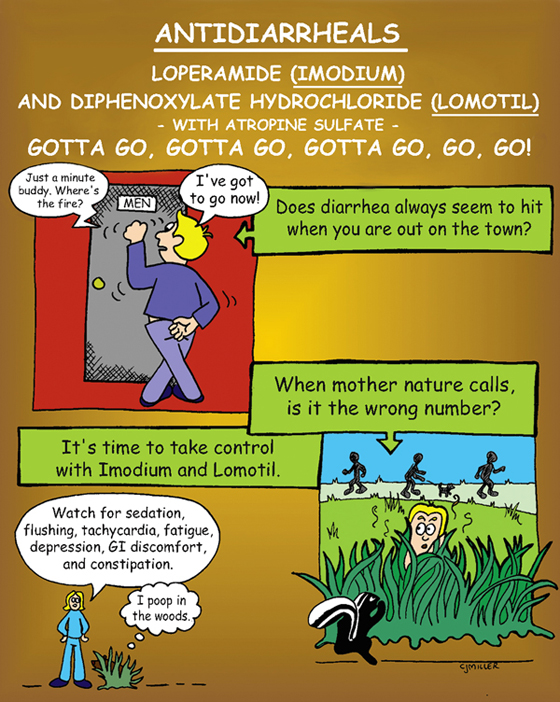
Antidiarrheals Loperamide (Imodium) and Diphenoxylate Hydrochloride (Lomotil)
ACTIONS
Direct effect on intestinal motility; slows intestinal transient and allows for increased absorption of water and fluids.
USES
• Symptomatic relief of acute nonspecific diarrhea
• Chronic diarrhea associated with inflammatory bowel disease
CONTRAINDICATIONS AND PRECAUTIONS
• Dehydration with electrolyte depletion
• Diarrhea from colitis or from infectious organism
• *Imodium not used for children under 6 years of age; Lomotil not used for children under 2 years of age*
SIDE EFFECTS
• **Drowsiness, dizziness, abdominal discomfort**
NURSING IMPLICATIONS
1. *Encourage adequate fluid intake; monitor hydration status.*
2. *Check bowel sounds for peristalsis; discontinue and report abdominal pain and distention.*
3. Do not give in the presence of bloody diarrhea or temperature of >101° F.
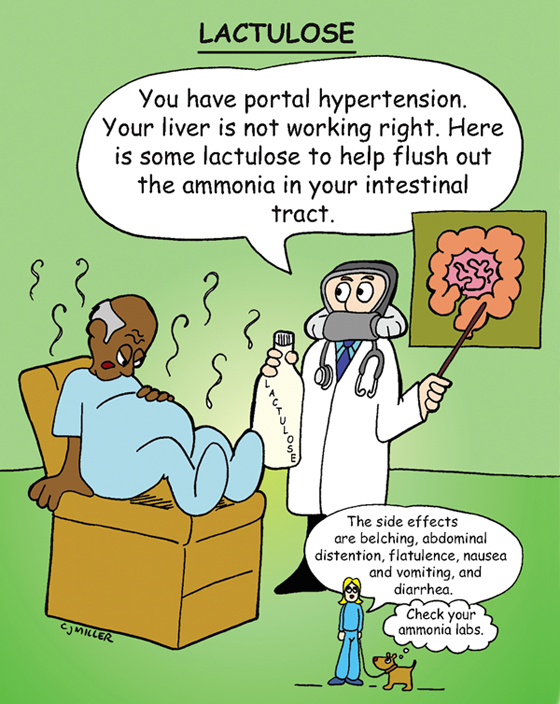
Lactulose
CLASSIFICATION
Hyperosmotic laxative and ammonia detoxicant
ACTIONS
Pulls ammonia into the colon from the intestines; promotes increased peristalsis, bowel evacuation (expelling ammonia from colon).
USES
• Treats portal systemic (hepatic) encephalopathy
• Treats constipation not responding to bulk laxatives
CONTRAINDICATIONS
• Undiagnosed abdominal pain, nausea and vomiting
PRECAUTIONS
• Diabetes mellitus (dehydration)
SIDE EFFECTS
• **Abdominal cramping, flatulence**
NURSING IMPLICATIONS
1. *Encourage increased fluid intake and high-fiber diet.*
2. Monitor bowel activity; may receive dose even with loose stools.
3. *Monitor serum ammonia and electrolyte level.*
4. *May be given by mouth (PO) or by enema:*
• *PO: Mix with fruit juice, water, or milk to improve flavor.*
• *Rectally: Use rectal balloon catheter; need to retain enema for 30 to 60 minutes.*
Sodium Polystyrene Sulfonate (Kayexalate)
CLASSIFICATION
Cation exchange resin
ACTIONS
Ion exchange releases sodium for potassium. Removes potassium from the blood into the intestine to be excreted.
USES
CONTRAINDICATIONS
• Hypernatremia, intestinal obstruction or perforation
PRECAUTIONS
• Use with caution in patients with sodium restriction (congestive heart failure, hypertension, edema).
SIDE EFFECTS
• Anorexia, nausea and vomiting, **constipation, fecal impaction**
NURSING IMPLICATIONS
1. Kayexalate does not correct hyperkalemia immediately (may take hours to days).
2. *If given orally, it usually is given with 20 to 100 ml of sorbitol doses to facilitate passage of resin through the intestinal tract, which helps prevent constipation.*
3. *If given by enema, a cleansing enema may be given before and after administering the enema with medication. Sorbitol 100 ml may be added to the enema solution. After the medication is given, flush with 50 to 100 ml of fluid and clamp. Retain for several hours if possible.*
4. *Draw potassium levels every 24 hours.*
5. *Monitor daily bowel activity and stool consistency (fecal impaction may occur, especially in older adult patients).*
6. *Monitor patient’s electrolytes level and electrocardiogram.*