Procedure 8 Acute Repair of Zone 2 Flexor Tendon Injury
![]() See Video 5: Acute Repair of Zone 2 Flexor Tendon Injury
See Video 5: Acute Repair of Zone 2 Flexor Tendon Injury
Figure 8-7 is adapted from Tang JB. Flexor tendon repair in zone 2C. J Hand Surg [Br]. 1994;19:72-75, with permission from Elsevier. Figure 8-18 is adapted from Strickland JW. Development of flexor tendon surgery: twenty-five years of progress. J Hand Surg [Am]. 2000;25:214-235, with permission from Elsevier.
Indications
 Acute repair of zone 2 flexor tendon injuries is indicated when there is a clean-cut injury with the following findings:
Acute repair of zone 2 flexor tendon injuries is indicated when there is a clean-cut injury with the following findings:
 A tendon defect of up to 1 cm can be repaired by end-to-end suturing. Greater losses (up to 2 to 3 cm) may need an intramuscular tendon lengthening via forearm incisions, and larger tendon gaps will need tendon grafting.
A tendon defect of up to 1 cm can be repaired by end-to-end suturing. Greater losses (up to 2 to 3 cm) may need an intramuscular tendon lengthening via forearm incisions, and larger tendon gaps will need tendon grafting.
Examination/Imaging
Clinical Examination
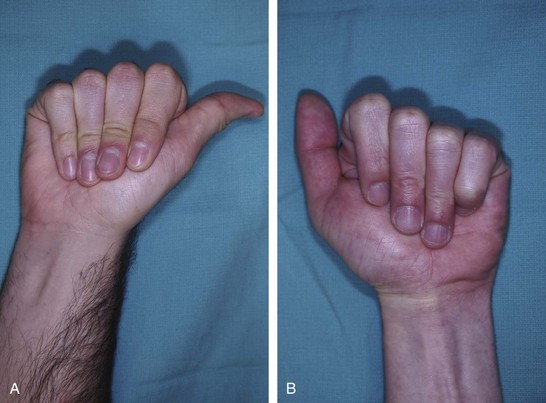
 Patients present with loss of active distal interphalangeal (DIP) and proximal interphalangeal (PIP) joint flexion if both FDP and FDS are divided, or loss of only DIP joint flexion if only FDP has been injured. On inspection, the normal finger cascade is lost with the affected digit in an extended position.
Patients present with loss of active distal interphalangeal (DIP) and proximal interphalangeal (PIP) joint flexion if both FDP and FDS are divided, or loss of only DIP joint flexion if only FDP has been injured. On inspection, the normal finger cascade is lost with the affected digit in an extended position.
 The function of the FDP is determined by asking the patient to actively flex the DIP joint of the involved finger.
The function of the FDP is determined by asking the patient to actively flex the DIP joint of the involved finger.
 Testing for FDS injury is more complex compared with the FDP because the PIP joint is flexed both by the FDS and by the FDP. Therefore, one needs to check the function of the FDS while blocking the action of the FDP.
Testing for FDS injury is more complex compared with the FDP because the PIP joint is flexed both by the FDS and by the FDP. Therefore, one needs to check the function of the FDS while blocking the action of the FDP.
 A partial tendon laceration should be suspected in patients in whom active motion is associated with pain or triggering.
A partial tendon laceration should be suspected in patients in whom active motion is associated with pain or triggering.
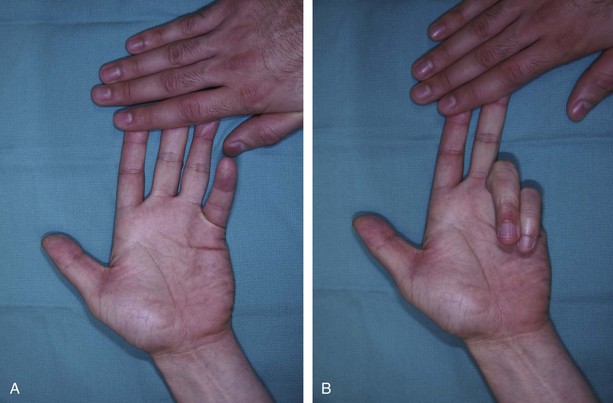
 In patients who cannot cooperate (e.g., children or comatose or intoxicated patients), one can look for passive movement of the fingers resulting from the wrist tenodesis effect or by squeezing the forearm muscles (Fig. 8-5). The same maneuvers can be used when trying to differentiate between tendon injury and inability to move as a result of nerve palsy.
In patients who cannot cooperate (e.g., children or comatose or intoxicated patients), one can look for passive movement of the fingers resulting from the wrist tenodesis effect or by squeezing the forearm muscles (Fig. 8-5). The same maneuvers can be used when trying to differentiate between tendon injury and inability to move as a result of nerve palsy.
 It is important to examine the patient for presence of concomitant injuries to the digital arteries and nerves.
It is important to examine the patient for presence of concomitant injuries to the digital arteries and nerves.
Imaging
 Preoperative imaging studies are not typically necessary, but anteroposterior and lateral x-rays may help identify associated bony injury. When a patient presents with unstable or intra-articular fractures, rigid fixation of the fracture is performed so that judicious tendon mobilization can be performed after tendon repair.
Preoperative imaging studies are not typically necessary, but anteroposterior and lateral x-rays may help identify associated bony injury. When a patient presents with unstable or intra-articular fractures, rigid fixation of the fracture is performed so that judicious tendon mobilization can be performed after tendon repair.
Surgical Anatomy
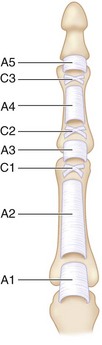
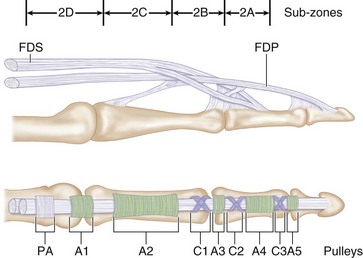
 Zone 2 contains both the FDS and FDP tendons and extends from the proximal edge of the A1 pulley in the palm to the insertion of the FDS over the middle phalanx. It includes four annular pulleys (A1, A2, A3, and A4) and two cruciate pulleys (C1 and C2) (Fig. 8-6).
Zone 2 contains both the FDS and FDP tendons and extends from the proximal edge of the A1 pulley in the palm to the insertion of the FDS over the middle phalanx. It includes four annular pulleys (A1, A2, A3, and A4) and two cruciate pulleys (C1 and C2) (Fig. 8-6).
 Zone 2 was subdivided by Tang (1994) into four subzones (Fig. 8-7).
Zone 2 was subdivided by Tang (1994) into four subzones (Fig. 8-7).
 The blood supply to the tendons in this region comes from the vincular system and enters the tendon on the dorsal surface. It is recommended that core sutures be passed in the palmar portion of the tendon.
The blood supply to the tendons in this region comes from the vincular system and enters the tendon on the dorsal surface. It is recommended that core sutures be passed in the palmar portion of the tendon.
Exposures
 Bruner incisions or midaxial incisions (by incorporating the transverse lacerations) are designed from the DIP joint to the base of the finger (Fig. 8-8).
Bruner incisions or midaxial incisions (by incorporating the transverse lacerations) are designed from the DIP joint to the base of the finger (Fig. 8-8).
 Thick skin flaps are raised in a plane superficial to the tendon sheath to expose the tendon sheath (Fig. 8-9).
Thick skin flaps are raised in a plane superficial to the tendon sheath to expose the tendon sheath (Fig. 8-9).
Pearls
If the incision needs to be extended to the distal palm, one must avoid placing the incision in the web space to prevent a scar contracture that limits finger extension.
Knowing the mechanism of injury helps in determining the location of the distal cut end of the tendon, and the incision can be planned accordingly. If injury occurred in flexion, the distal cut end will migrate distal to the skin laceration with the finger held in extension. The skin incision will need to be extended distally. If injury occurred in extension, the distal cut end will be at the same level as the skin laceration. Retraction of the proximal cut end depends on the level of injury in relation to the vincular attachment. In zone 2A and 2B injuries, the proximal end may get caught at the A2 pulley. In zone 2C and 2D injuries, the tendon retracts to the distal palm, where the FDP is restricted by the lumbrical muscle attached to the radial side of the FDP.
Procedure
Step 1: Exposure of Divided Tendons
 The excursion of FDP within zone 2 is approximately 2 cm. To allow this excursion, we divide varying portions of the A2, A3, and A4 pulleys and the flexor sheath, depending on the location of the distal cut end of the tendon with the finger in extension (Fig. 8-10). Selective and limited division of the pulleys allows free movement of the repaired tendon while avoiding clinically significant bowstringing.
The excursion of FDP within zone 2 is approximately 2 cm. To allow this excursion, we divide varying portions of the A2, A3, and A4 pulleys and the flexor sheath, depending on the location of the distal cut end of the tendon with the finger in extension (Fig. 8-10). Selective and limited division of the pulleys allows free movement of the repaired tendon while avoiding clinically significant bowstringing.
Step 2: Retrieval of Proximal Tendon End
 This can be challenging when the tendon has retracted into the palm. The following maneuvers are used in sequence:
This can be challenging when the tendon has retracted into the palm. The following maneuvers are used in sequence:
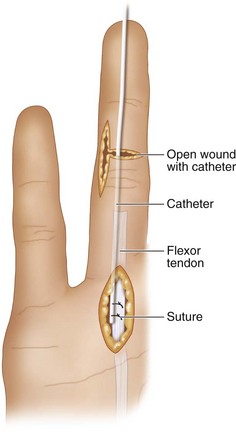
 If both these maneuvers do not work, the method described by Sourmelis and McGrouther should be tried. A chevron incision is made in the distal palm proximal to the A1 pulley. The flexor tendons are identified. If they are still within the A1/A2 pulley, they are not disturbed. A 5/6 French pediatric feeding tube is passed from retrograde through the flexor sheath to emerge at the proximal incision. The feeding tube is sutured to the palmar surface of the flexor tendon without withdrawing the tendons from the fibrous flexor sheath. If the tendon ends have retracted proximal to the A1 pulley, the feeding tube is sutured to the end of the tendons. Using a combination of pulling the feeding tube at the distal incision and pushing the flexor tendon at the proximal incision, the tendon ends are delivered into laceration (Fig. 8-11).
If both these maneuvers do not work, the method described by Sourmelis and McGrouther should be tried. A chevron incision is made in the distal palm proximal to the A1 pulley. The flexor tendons are identified. If they are still within the A1/A2 pulley, they are not disturbed. A 5/6 French pediatric feeding tube is passed from retrograde through the flexor sheath to emerge at the proximal incision. The feeding tube is sutured to the palmar surface of the flexor tendon without withdrawing the tendons from the fibrous flexor sheath. If the tendon ends have retracted proximal to the A1 pulley, the feeding tube is sutured to the end of the tendons. Using a combination of pulling the feeding tube at the distal incision and pushing the flexor tendon at the proximal incision, the tendon ends are delivered into laceration (Fig. 8-11).
 After retrieval to the site of repair, the tendon should be secured in place with a hypodermic needle to prevent it from retracting proximally and to allow a tension-free repair.
After retrieval to the site of repair, the tendon should be secured in place with a hypodermic needle to prevent it from retracting proximally and to allow a tension-free repair.
Step 3: Tendon Repair
 The tendon ends are gently débrided of frayed ends while retaining their length.
The tendon ends are gently débrided of frayed ends while retaining their length.
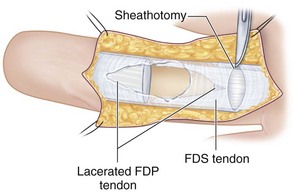
 The FDS is repaired before the FDP. An attempt is made to repair both slips of the FDS (Fig. 8-12). This may be difficult, especially in zone 2C, where the A2 pulley is narrowest. In such circumstances, repair of one slip is appropriate. Because of the flatness of the FDS at zone 2, its repair is a simple horizontal mattress suture repair of each slip of the FDS.
The FDS is repaired before the FDP. An attempt is made to repair both slips of the FDS (Fig. 8-12). This may be difficult, especially in zone 2C, where the A2 pulley is narrowest. In such circumstances, repair of one slip is appropriate. Because of the flatness of the FDS at zone 2, its repair is a simple horizontal mattress suture repair of each slip of the FDS.
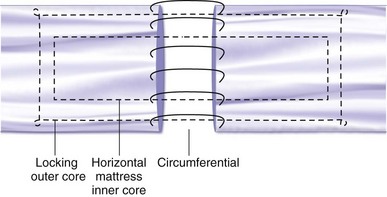
 Many methods of tendon repair have been described for the FDP. We use a 6-0 Prolene suture epitendinous repair combined with a 3-0 Ethibond modified double-Kessler core suture (Fig. 8-13).
Many methods of tendon repair have been described for the FDP. We use a 6-0 Prolene suture epitendinous repair combined with a 3-0 Ethibond modified double-Kessler core suture (Fig. 8-13).
 First the epitendinous repair of the dorsal half of the tendon is carried out. Sutures bites are taken at 1- to 2-mm intervals approximately 1 to 2 mm from the edge of the tendon. This is a continuous suture repair, and the loops are locked.
First the epitendinous repair of the dorsal half of the tendon is carried out. Sutures bites are taken at 1- to 2-mm intervals approximately 1 to 2 mm from the edge of the tendon. This is a continuous suture repair, and the loops are locked.
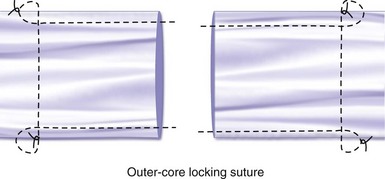
 Next a modified Kessler core suture is placed in the standard manner (Fig. 8-14). The transverse portion of the suture is locked. It is important to remember that 3-0 Ethibond is a braided suture and does not glide well within the tendon substance. One should therefore pull the required length of the suture through the tendon at first pass. A minimum of 0.7 cm, and most commonly 1 to 1.2 cm, of the tendon is grasped by the longitudinal portion of the suture loop before making the transverse portion.
Next a modified Kessler core suture is placed in the standard manner (Fig. 8-14). The transverse portion of the suture is locked. It is important to remember that 3-0 Ethibond is a braided suture and does not glide well within the tendon substance. One should therefore pull the required length of the suture through the tendon at first pass. A minimum of 0.7 cm, and most commonly 1 to 1.2 cm, of the tendon is grasped by the longitudinal portion of the suture loop before making the transverse portion.
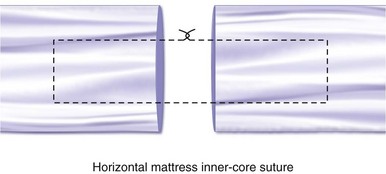
 A horizontal mattress suture is placed within the previous suture repair using 4-0 Ethibond. Approximately 0.5 to 0.6 cm of the tendon is grapsed by the longitudinal portion of the suture loop before making the transverse portion (Fig. 8-15).
A horizontal mattress suture is placed within the previous suture repair using 4-0 Ethibond. Approximately 0.5 to 0.6 cm of the tendon is grapsed by the longitudinal portion of the suture loop before making the transverse portion (Fig. 8-15).
 The palmar half of the epitendonous repair is now completed (Fig. 8-16).
The palmar half of the epitendonous repair is now completed (Fig. 8-16).
Step 3 Pearls
If the FDS is lacerated at the Camper chiasm, direct mattress repair to the radial and ulnar tendon ends can be performed using 4-0 or 5-0 braided suture.
After tendon repair, the finger should be placed through gentle range of motion to ensure adequate tendon gliding through the pulley system. If the pulleys are restricting free motion, they should be vented by divided them at one edge.
Step 3 Pitfalls
If a gap is noted during passive mobilization, the repair needs to be done again or strengthened. The gap will heal by scarring, which will be weak and can rupture easily.
It is crucial to orient the FDS and FDP correctly during repair because the tendons may twist in the sheath. Additionally, the lacerated FDP may migrate outside the FDS chiasm, and it should be gently passed through the chiasm. If the vincula is still intact, it must be carefully preserved during the repair.
Postoperative Care and Expected Outcomes
 The patient is splinted in 30 degrees of wrist flexion and 60 degrees of metaphalangeal (MP) flexion and with the fingers in slight flexion.
The patient is splinted in 30 degrees of wrist flexion and 60 degrees of metaphalangeal (MP) flexion and with the fingers in slight flexion.
 It is critical for the surgeon and therapist to maintain direct communication during the postoperative period.
It is critical for the surgeon and therapist to maintain direct communication during the postoperative period.
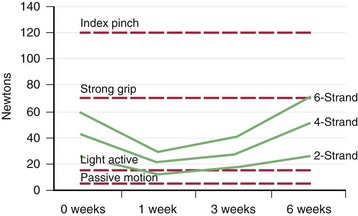
 Tendon repair strength declines for the first week after surgery, plateaus for 1 week, and then slowly begins to get stronger. In this initial phase of healing, all strength across the repair is due to the suture and will increase predictably with increasing strand count. During tendon healing, the force applied to the repair should always be below the repair strength, or rupture may occur. Following this logic, and explicitly described later for a four-strand core-suture repair, passive exercises always remain below rupture threshold and are used for the initial 4 weeks following surgery. At 4 weeks, active exercises are safely started. Strengthening is not started until 8 weeks (Fig. 8-18).
Tendon repair strength declines for the first week after surgery, plateaus for 1 week, and then slowly begins to get stronger. In this initial phase of healing, all strength across the repair is due to the suture and will increase predictably with increasing strand count. During tendon healing, the force applied to the repair should always be below the repair strength, or rupture may occur. Following this logic, and explicitly described later for a four-strand core-suture repair, passive exercises always remain below rupture threshold and are used for the initial 4 weeks following surgery. At 4 weeks, active exercises are safely started. Strengthening is not started until 8 weeks (Fig. 8-18).
 Indiana Early Active Mobilization, or the Tenodesis Program, is initiated on postoperative day 3. This involves both passive exercises using a Modified Duran Program and place-and-hold exercises.
Indiana Early Active Mobilization, or the Tenodesis Program, is initiated on postoperative day 3. This involves both passive exercises using a Modified Duran Program and place-and-hold exercises.
 At 4 weeks, the tenodesis splint is discontinued, but the place-and-hold exercises continue. Additional active exercises are started, consisting of making a fist while the wrist is in neutral position. Active wrist flexion and extension are allowed. The Modified Duran Program is continued within the DBS.
At 4 weeks, the tenodesis splint is discontinued, but the place-and-hold exercises continue. Additional active exercises are started, consisting of making a fist while the wrist is in neutral position. Active wrist flexion and extension are allowed. The Modified Duran Program is continued within the DBS.
 At 5 weeks, active extension is allowed.
At 5 weeks, active extension is allowed.
 At 6 weeks, the DBS is discontinued, and the involved finger is buddy-taped to the adjacent finger. An extension splint is worn at night.
At 6 weeks, the DBS is discontinued, and the involved finger is buddy-taped to the adjacent finger. An extension splint is worn at night.
 At 8 weeks, progressive strengthening is started.
At 8 weeks, progressive strengthening is started.
 At 10 to 12 weeks, the patient may return to all activities but should not perform heavy lifting until 16 weeks.
At 10 to 12 weeks, the patient may return to all activities but should not perform heavy lifting until 16 weeks.
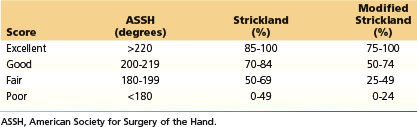
 Based on the Total Active Motion (TAM) evaluation system proposed by Kleinert and Verdan, and advocated by the American Society for Surgery of the Hand, most patients should regain good to excellent function after primary repair of flexor tendons (Table 8-1). TAM is calculated by the following formula:
Based on the Total Active Motion (TAM) evaluation system proposed by Kleinert and Verdan, and advocated by the American Society for Surgery of the Hand, most patients should regain good to excellent function after primary repair of flexor tendons (Table 8-1). TAM is calculated by the following formula:
Kitis PT, Buker N, Kara IG. Comparison of two methods of controlled mobilisation of repaired flexor tendons in zone 2. Scand J Plast Reconstr Surg Hand Surg. 2009;43:160-165.
Tang JB. Flexor tendon repair in zone 2C. J Hand Surg [Br]. 1994;1:72-75.
Tang JB. Indications, methods, postoperative motion and outcome evaluation of primary flexor tendon repairs in zone 2. J Hand Surg [Br]. 2007;32:118-129.
Thien TB, Becker JH, Theis JC. Rehabilitation after surgery for flexor tendon injuries in the hand. Cochrane Database Syst Rev. 2004;4:CD003979.