CASE 8
TC is a 9-year-old child with recurrent necrotic infections on the legs and arms. Discussion with the parents to determine anomalies since birth revealed that TC’s umbilical cord had persisted much longer than that of his siblings. As well, TC’s wounds healed more slowly and left noticeable scars. Both parents emphasized that they were well and that no members of the extended family had presented with similar history. Swabs reveal repeated bacterial infections. A complete blood cell count with differential showed a normal number of leukocytes, although the numbers were slightly elevated. Serology showed no deficit in immunoglobulins, complement, or numbers and function of B and T cells. B cell function was based on antibody titers to childhood immunization, whereas T cell function was based on cytokine secretion by polyclonally stimulated T cells. What might be going on, and what would you do about it?
QUESTIONS FOR GROUP DISCUSSION
RECOMMENDED APPROACH
Implications/Analysis of Clinical History
We need to determine why this child has prominent lesions on the skin. These areas represent places where our natural skin defense barrier is being constantly challenged by mechanical means, yet most people do not get these infections! The prevalence of bacterial infections points to defects in B cells, phagocytes, or complement. However, the lack of systemic (blood-borne) disease, such as respiratory tract infections with Pseudomonas aeruginosa or Streptococcus pneumoniae suggests this is unlikely to be a defect in the functional activity of B cells or phagocytes. The lack of viral infections suggests that this is not likely a T cell or NK cell disorder.
Implications/Analysis of Laboratory Investigation
A complete blood cell count (CBC) is a test that determines the quantity and proportion of various components in blood and includes measures of white blood cells (leukocytes), white blood cell differential, red blood cell, platelet, hemoglobin, and hematocrit (ratio of the volume of red blood cells to the volume of whole blood). A simple blood cell count measures the total white blood cell count, whereas the CBC gives, as well, a white blood cell differential that provides information regarding percentages of granulocytes, monocytes, lymphocytes, basophils, and eosinophils in the sample. A normal white blood cell count is very age dependent!!! (See Appendix.)
TC’s high normal white blood cell count and differential, with normal serum immunoglobulins, normal antibody titers to childhood immunization, and normal cytokine production by T cells should suggest that this is not likely to be a simple B cell and/or T cell disorder. Therefore, it is reasonable to conclude that TC’s infections are not due to defects in adaptive immunity. All of the information here points toward possible defects in the innate defense mechanisms. Because the CBC/differential was normal, a deficiency in any cell population of the innate immune system can be ruled out. Normal complement CH50 and AH50 tests, which measure the overall activity of the classical and alternative pathways, respectively, ruled out complement defects (see Case 11). Results of all these laboratory tests suggest the defect does not lie in a component of any effector mechanism per se.
Additional Laboratory Tests
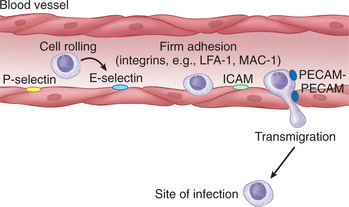
One would certainly run some tests to make sure an unusual presentation of chronic granulomatous disease (CGD) (see Case 6) or other enzymatic defect that leads to defective macrophage resistance is not missed. CGD, associated with defects in NADPH oxidase, affects all the phagocytes in the body, wherever they might be, and so a CGD defect generally presents with frequent common multiple-site infections (e.g., the lung, upper respiratory tract). Although one might consider toll-like receptor (TLR) defects (see Case 7) or subtle nucleotide oligomerization (NOD) protein defects (see Case 9), the clinical presentations are not consistent with mutations in either of these proteins. Rather, laboratory results are consistent with the hypothesis that this child has normal effector cells that would combat infection appropriately if they were able to reach the site of infection. The defect sounds most likely to be one of altered cell migration, with the relevant effector cells not getting to the site of action. For leukocytes to leave the circulation and enter tissues at the site of infection, a number of adhesive interactions must take place between the leukocytes and the activated vascular endothelium (Fig. 8-1). A prominent molecule on leukocytes is CD18, which is known to be a component of several cell surface adhesion molecules (β2 integrins). CD18 flow cytometric analysis revealed that TC’s leukocytes did not express detectable CD18.
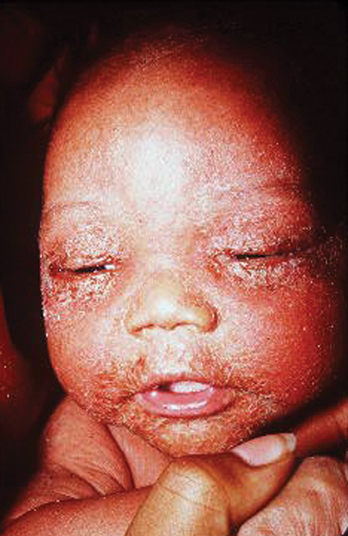
ETIOLOGY: LEUKOCYTE ADHESION DEFICIENCY-1
LAD-1 is an autosomal recessive disorder characterized by repeated bouts of skin associated bacterial infections that heal very slowly (Fig. 8-2). Skin infections result in necrotic sores, without evidence for pus. (Pus is the detritus of dead white blood cells, lymph, and the remains of dead bacteria that collects at the site of infection.) In addition to the skin, common sites of infection are the oral mucosa (e.g., gingivitis) and the respiratory tract. LAD-1 is suspected when there is a delay in umbilical cord separation.
OTHER DEFECTS IN CELL TRAFFICKING
LAD-2: Defects in Carbohydrates (Selectin Counter Molecules)
Carbohydrates present on circulating leukocytes are the counter molecules/ligands for E-selectin and P-selectin. P-selectin is the first selectin to be expressed on the endothelium during an inflammatory response because histamine (released from mast cells) triggers its translocation from the cytosol to the cell surface. Defects in fucose metabolism result in a deficiency of particular carbohydrates on the leukocyte cell surface. Because these carbohydrates are ligands for the E-selectin and P-selectin, cell rolling that should slow the leukocytes at the site of inflammation does not occur.