Procedure 79 External Fixation of Comminuted Intra-articular Distal Radius Fractures
Indications
 Unstable unreducible extra-articular distal radius fractures
Unstable unreducible extra-articular distal radius fractures
 Displaced intra-articular distal radius fractures that can be reduced by closed or percutaneous means
Displaced intra-articular distal radius fractures that can be reduced by closed or percutaneous means
 Highly comminuted distal radius fractures that are reduced openly and fixed with plates or pins that require unloading of the carpus to allow healing
Highly comminuted distal radius fractures that are reduced openly and fixed with plates or pins that require unloading of the carpus to allow healing
Examination/Imaging
Imaging
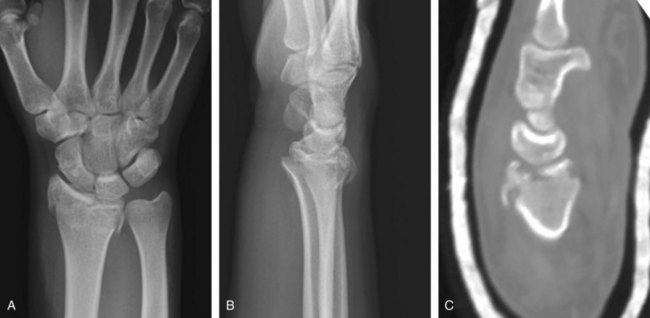
 Anteroposterior and lateral images of the wrist should be taken; these will demonstrate the nature of the fracture (Fig. 79-1).
Anteroposterior and lateral images of the wrist should be taken; these will demonstrate the nature of the fracture (Fig. 79-1).
 If there is significant intra-articular comminution, a computed tomography scan will provide more information on the location and displacement of the fracture fragments (Fig. 79-2).
If there is significant intra-articular comminution, a computed tomography scan will provide more information on the location and displacement of the fracture fragments (Fig. 79-2).
Surgical Anatomy
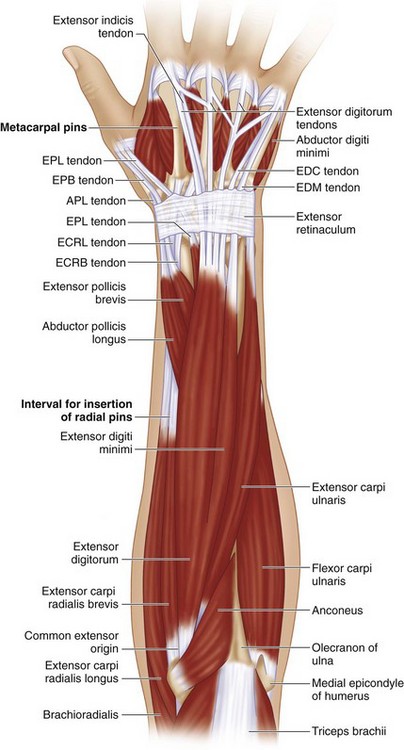
 The external fixator is placed dorsoradially across the wrist. The distal pins are placed in the second metacarpal, the proximal pins are placed in the radial shaft about a hand’s breadth proximal to the radial styloid. This position is just proximal to the “outrigger” muscles—abductor pollicis longus (APL) and extensor pollicis brevis (EPB)—as they cross the radial shaft (Fig. 79-3).
The external fixator is placed dorsoradially across the wrist. The distal pins are placed in the second metacarpal, the proximal pins are placed in the radial shaft about a hand’s breadth proximal to the radial styloid. This position is just proximal to the “outrigger” muscles—abductor pollicis longus (APL) and extensor pollicis brevis (EPB)—as they cross the radial shaft (Fig. 79-3).
Exposures
 The first pin of the external fixator is placed in the radial shaft, and the second pin is placed in the second metacarpal. After alignment of the wrist is established, the external fixation bar slides over these two pins. The remaining pins for the metacarpal and the radius can be inserted by marking the appropriate position on the arm to permit smooth fitting of all the pin slots on the external fixator.
The first pin of the external fixator is placed in the radial shaft, and the second pin is placed in the second metacarpal. After alignment of the wrist is established, the external fixation bar slides over these two pins. The remaining pins for the metacarpal and the radius can be inserted by marking the appropriate position on the arm to permit smooth fitting of all the pin slots on the external fixator.
 The radial shaft pins are placed through a 3-cm incision on the “bare area” of the radius, proximal to the first compartment tendons in a dorsoradial position. The deep interval is between the extensor carpi radialis longus (ECRL) and the brachioradialis (BR) tendons. The radius should be directly visualized as the pins are placed into the bone (Fig. 79-4)
The radial shaft pins are placed through a 3-cm incision on the “bare area” of the radius, proximal to the first compartment tendons in a dorsoradial position. The deep interval is between the extensor carpi radialis longus (ECRL) and the brachioradialis (BR) tendons. The radius should be directly visualized as the pins are placed into the bone (Fig. 79-4)
 The superficial radial nerve (SRN) needs to be visualized and protected in the proximal exposure (Fig. 79-5).
The superficial radial nerve (SRN) needs to be visualized and protected in the proximal exposure (Fig. 79-5).
 The second metacarpal pins are placed on the dorsoradial aspect. The extensor tendons and first dorsal interosseus (FDI) muscle need to be retracted and protected (Fig. 79-6).
The second metacarpal pins are placed on the dorsoradial aspect. The extensor tendons and first dorsal interosseus (FDI) muscle need to be retracted and protected (Fig. 79-6).
Procedure
Step 1
 The pins for the external fixator are placed in a dorsoradial position, about 45 degrees from radial midlateral. This position prevents the fixator from obstructing postoperative radiographs and allows the thumb full range of motion (ROM), particularly extension (Fig. 79-7).
The pins for the external fixator are placed in a dorsoradial position, about 45 degrees from radial midlateral. This position prevents the fixator from obstructing postoperative radiographs and allows the thumb full range of motion (ROM), particularly extension (Fig. 79-7).
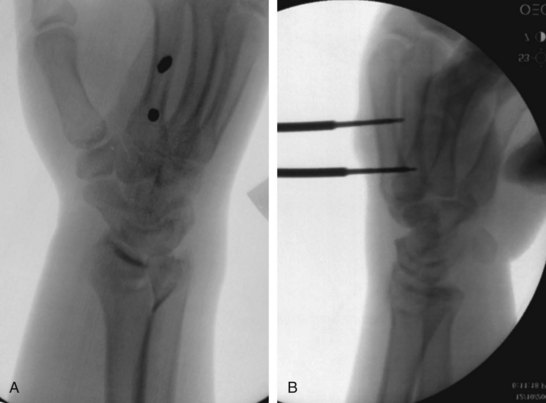
 The position of the pins should be confirmed by fluoroscopy to be within the respective bone and of appropriate length. The images should be saved for documentation of the case (Fig. 79-8).
The position of the pins should be confirmed by fluoroscopy to be within the respective bone and of appropriate length. The images should be saved for documentation of the case (Fig. 79-8).
 The incisions that were used for pin placement are then closed with interrupted 3-0 nylon sutures. This closure should not be overly tight because the skin tension may change after distraction of the fixator.
The incisions that were used for pin placement are then closed with interrupted 3-0 nylon sutures. This closure should not be overly tight because the skin tension may change after distraction of the fixator.
Step 2
 The fixator bar is placed across the fractures and attached to the half-pins through clamps.
The fixator bar is placed across the fractures and attached to the half-pins through clamps.
 Distraction and ulnar deviation are imparted to the fracture to induce a provisional reduction. A single 0.062-inch K-wire may be placed percutaneously dorsally to assist in holding the reduction (Fig. 79-9).
Distraction and ulnar deviation are imparted to the fracture to induce a provisional reduction. A single 0.062-inch K-wire may be placed percutaneously dorsally to assist in holding the reduction (Fig. 79-9).
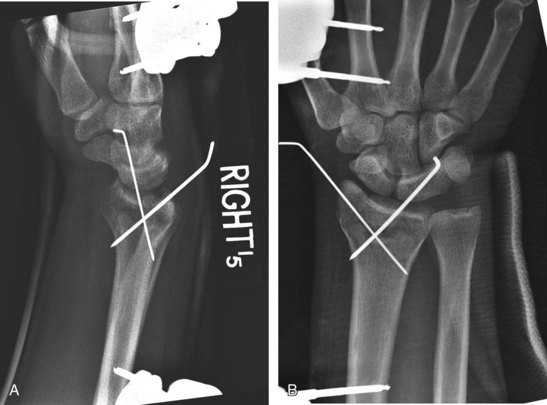
 A second K-wire can be placed through the radial styloid to stabilize the fracture fragments. The distal radius alignment should be checked with anteroposterior and lateral images to ensure that the joint surface is congruent, has no step-off, and possesses the proper inclination and tilt (Fig. 79-10).
A second K-wire can be placed through the radial styloid to stabilize the fracture fragments. The distal radius alignment should be checked with anteroposterior and lateral images to ensure that the joint surface is congruent, has no step-off, and possesses the proper inclination and tilt (Fig. 79-10).
 The frame should be tightened and ensured to be stable and not impede finger motion.
The frame should be tightened and ensured to be stable and not impede finger motion.
 At the close of the procedure, the fingers should have full passive flexion and extension, and the hand should not be placed in excessive flexion or ulnar deviation.
At the close of the procedure, the fingers should have full passive flexion and extension, and the hand should not be placed in excessive flexion or ulnar deviation.
Step 2 Pearls
The frame should not be overdistracted, which may induce carpal stiffness or the inability to allow finger flexion owing to tightening of the finger extensors.
After the distal radius is stabilized, the distal ulna is checked for stability. If the distal radioulnar joint is unstable, the distal ulna is reduced and pinned to the radius. Alternatively the triangular fibrocartilage complex may be repaired, or a large ulnar styloid fracture fixed.
Postoperative Care and Expected Outcomes
 The dressings are removed after 7 to 10 days, and the pin sites and wounds are evaluated.
The dressings are removed after 7 to 10 days, and the pin sites and wounds are evaluated.
 The pin sites are dressed for the first 3 weeks. If there is any discharge, half-strength peroxide is used to clean them daily.
The pin sites are dressed for the first 3 weeks. If there is any discharge, half-strength peroxide is used to clean them daily.
 The percutaneous pins may be removed in the office after 3 to 4 weeks. The external fixator is left in place, and finger ROM is encouraged (Fig. 79-11).
The percutaneous pins may be removed in the office after 3 to 4 weeks. The external fixator is left in place, and finger ROM is encouraged (Fig. 79-11).
 After the sutures are removed, the incisions are dry, and the percutaneous pins are removed, the patients may shower with the fixator in place.
After the sutures are removed, the incisions are dry, and the percutaneous pins are removed, the patients may shower with the fixator in place.
 The fixator is removed in the office after 4 to 6 weeks, and the pin sites are dressed sterilely.
The fixator is removed in the office after 4 to 6 weeks, and the pin sites are dressed sterilely.
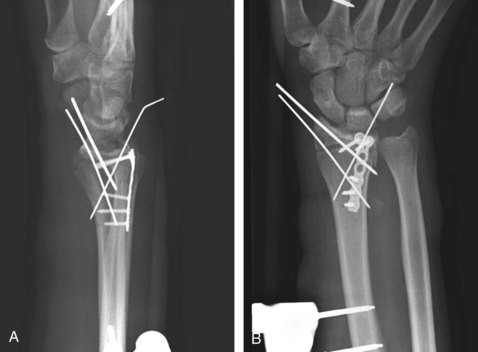
 Final radiographs should demonstrate a healed fracture with an anatomic articular surface and a reduced carpus (Fig. 79-12).
Final radiographs should demonstrate a healed fracture with an anatomic articular surface and a reduced carpus (Fig. 79-12).
Pearls
In a comminuted fracture, the reduction achieved with external fixation and percutaneous pins alone may be inadequate (Fig. 79-13).
Persistent articular displacement (die-punch fragment) can be reduced through a limited open approach and fixation with small plates (Fig. 79-14).
The fixator is left in place to unload the joint until early fracture healing.
Capo JT, Rossy W, Henry P, et al. External fixation of distal radius fractures: effect of distraction and duration. J Hand Surg [Am]. 2009;34:1605-1611.
Kreder HJ, Hanel DP, Agel J, et al. Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular fractures of the distal radius: a randomized, controlled trial. J Bone Joint Surg [Br]. 2005;87:829-836.
Leung F, Tu YK, Chew WY, Chow SP. Comparison of external and percutaneous pin fixation with plate fixation for intra-articular distal radial fractures: a randomized study. J Bone Joint Surg [Am]. 2008;90:16-22.
Margaliot Z, Haase SC, Kotsis SV, et al. A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures. J Hand Surg [Am]. 2005;30:1185-1199.
Wei DH, Raizman NM, Bottino CJ, et al. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate: a prospective randomized trial. J Bone Joint Surg [Am]. 2009;91:1568-1577.