CHAPTER 78
Shin Splints
Definition
“Shin splints” is best thought of as a clinical syndrome defined in terms of pain and discomfort in the anterior portion of the leg from repetitive activity on hard surfaces or from forcible, excessive use of the foot flexors. The diagnosis should be limited to musculoskeletal inflammations, excluding stress fractures, diet-related diseases [1], and ischemic disorders [2], although it may coexist with such disorders.
Shin splints most commonly occur in athletes who have sudden increases or changes in their training activity. This disorder occurs in runners and in athletes who participate in high-impact court or field sports as well as in gymnasts and particularly ballet dancers, alone or in conjunction with other overuse syndromes [3], but it has also been well documented and studied in military personnel [4–6]. The etiology of shin splints is not clearly defined, but it is likely to be multifactorial with biomechanical abnormalities of the foot and ankle, poor footwear and shock absorption, hard playing surfaces, and training errors. Other contributing factors may include weakness of anterior and posterior compartment musculature, inadequate warm-up, leg length discrepancy, tibial torsion, excessive femoral anteversion, and increased Q angle [7,8], as is seen in women.
One prospective study [6] in military cadets looked at seven anatomic variables and identified greater internal and external hip range of motion and lower mean calf girth to be associated with a higher incidence of exertional medial tibial pain in men. It also showed a high rate of injury among women, but no intrinsic factor was specifically identified. Nutritional and endocrine factors are more likely to play an etiologic role in stress reactions. In school-age athletes and adults who participate in seasonal sports, shin splints can occur when they resume their sport or start a new land-based sport (e.g., high-school or college athletes who go from playing basketball to cross-country or track).
It is important for the clinician to differentiate shin splints, a fairly benign condition, from acute compartment syndrome (a potential emergency) and from the different types of stress fractures that can occur in this region. The anterior lower leg is especially predisposed to compartment syndrome because of its high vulnerability to injury and its relatively limited compartment compliance [9]. It is most common to study these diagnoses together because many may coexist and symptoms overlap. Further discussion of these other diagnoses may be found in their respective chapters. Tibial periostitis has been described as an initial manifestation of polyarteritis nodosa [10]. Primary adamantinoma [11], a rare low-grade primary bone tumor, and hydatid bone disease [12] have also been reported in this region.
Symptoms
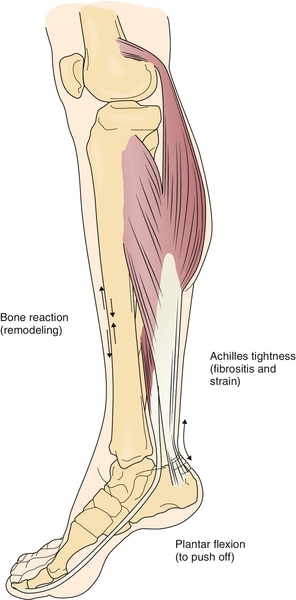
Patients presenting with shin splints usually complain of a dull and aching pain near the junction of the mid and distal thirds of the posteromedial or anterior tibia (Fig. 78.1). Clinicians should be aware of the wide differential diagnosis of pain in this region; not all anterior tibial pains are shin splints. Symptoms are commonly bilateral, occur with exercise, and are relieved with rest [13]. Initially the pain may ease with continued running and recur after prolonged activity. Those with more severe shin splints may have persistent pain with normal walking, with activities of daily living, or at rest.
Physical Examination
Physical examination typically reveals generalized tenderness along the medial tibia. Mild swelling may be present. Resisted plantar flexion, toe flexion, or toe raises may aggravate symptoms, and pain-inhibitory weakness may be evident. Striking a 128-Hz tuning fork and placing it on the tibia may reproduce the pain associated with stress fractures. Patients with stress fractures will usually have point tenderness over the bone at the site of stress fracture. Lower extremity idiopathic osteonecrosis is most common in the fifth decade of life at the medial tibial plateau [14], whereas those with shin splints will have more widespread tenderness to palpation that is more distal than these other pathologic processes. However, longitudinal tibial stress reactions may share a common anatomic pain distribution, and one study [15] showed tibial stress reactions in this same distal-third region.
The lower extremity examination focuses on static and dynamic components of the kinetic chain to uncover signs of coexisting lower extremity issues that may be contributing factors. These include forefoot pronation, pes cavus, pes planus, and excessive heel valgus or varus. Comparatively tight or weak lower extremity muscle groups should be noted for later rehabilitation goals. In particular, relative ankle plantar flexion, dorsiflexion, inversion, and eversion strength should be examined. Careful review of systems should be negative for fever, chills, night sweats, unintentional weight loss, and loss of bowel or bladder control. The neurologic portion of the examination, including sensation and muscle stretch reflexes, should be normal.
Functional Limitations
In early stages of shin splints, activity limitations occur most often during running or participation in ballistic activities. When symptoms are more severe, they may occur with walking or at rest, thus causing further functional limitations. Athletes may be unable to participate in their sport, and attempts to cross-train into other sports may result in worsening of symptoms.
Diagnostic Studies
Plain radiographs are typically normal early in the disease process but may be of use in ruling out more ominous disease, especially if symptoms are manifested unilaterally. Later, there may be evidence of periosteal thickening. Radionuclide bone scanning helps differentiate shin splints from stress fracture. Diffuse radioisotopic uptake along the medial or posteromedial tibia on the delayed phase is the pattern usually seen with shin splints. A focal defined area of uptake in all phases is more consistent with a stress fracture [16]. Fat-suppressed magnetic resonance imaging may also be useful for discrimination between stress fracture and shin splints before plain radiography shows detectable periosteal reaction [17]. Exertional compartment syndrome is uncommon, but if clinical suspicion is high, compartment pressure measurements must be done to rule it out. Magnetic resonance imaging of the lumbar spine may be indicated if lumbar radiculopathy is in the differential diagnosis or lumbar spinal stenosis is suspected in older athletes or younger athletes with a congenitally narrow spinal canal. Electrodiagnostic studies should be essentially normal, but membrane irritability manifested as positive sharp waves or fibrillations may be seen in any inflamed muscle. Nerve conductions should be normal in the absence of any concomitant nerve entrapment as may be seen in compartment syndrome.
Treatment
Initial
As with many overuse syndromes, relative rest—that is, participation only in those activities that can be done without pain—is the key to initial management. If reducing mileage, court time, or studio time or just reducing intensity allows the athlete to remain pain free, continuation of the activity may be acceptable. In general, however, even in mild cases, the athlete should avoid repetitive lower extremity stress for at least 1 to 2 weeks. In more serious cases, athletes may need to stop running entirely for a longer time. If walking is painful, crutches are indicated. A variety of commercially available off-the-shelf braces may decrease pain associated with weight bearing. Wearing of an elastic compression bandage may prevent additional swelling when compartment syndrome has been ruled out as compression may worsen vascular symptoms.
Stretching and ice or ice massage to the involved areas can be helpful. Nonsteroidal anti-inflammatory drugs can reduce inflammation and help manage pain. Analgesics can be taken for pain, but caution should be used to not enable further overtraining. Whirlpool, phonophoresis, iontophoresis, and therapeutic ultrasound are traditionally attempted and may have a role in symptomatic management or inflammatory phase reduction. Electrical stimulation should probably be considered contraindicated in this diagnosis, in which the pathoetiology points to excessive muscle contraction and a reactive periostitis in the first place.
In addressing malalignments of the lower extremities, orthoses, such as longitudinal arch supports with or without a medial heel wedge, may be indicated in select patients. Although a review of the literature fails to yield any objective evidence for the widespread use of any of these interventions, the most encouraging evidence seems to be for the use of shock-absorbing insoles [4,18]. Custom orthotic inserts, in one study of healthy female runners, have been shown to decrease rearfoot eversion angle and velocity and internal inversion moment as well as to decrease ankle dynamics in the frontal and sagittal planes. Whereas the particular relevance to shin splints is unclear, the ability to affect these measurements seems promising [19].
Rehabilitation
In individuals who continue to have pain despite initial conservative treatment, physical therapy may be indicated to decrease pain and further educate the patient about the disorder. Although pathophysiologically distinct from chronic exertional compartment syndrome, shin splints were once thought to be a form of chronic exertional compartment syndrome and vice versa [20], and the two entities are seldom discussed outside the context of each other. Ice, passive modalities (except electrical stimulation), and nonsteroidal anti-inflammatory drugs before exercise may help in enabling the rehabilitation program.
Once the symptoms have diminished, the rehabilitation program focuses on improving muscle strength, flexibility, and endurance and preventing recurrence of injury [21]. “Writing” the alphabet with the great toe moves the ankle through full range of motion in all planes and may be started early.
The primary muscles thought to be involved in shin splints are the flexor digitorum longus and the soleus. Others have implicated the tibialis posterior, but its attachment is more posterior than the area of typical shin splint symptoms, and it actually attaches to the interosseous membrane more than to the medial tibia [22]. The deep crural fascia also attaches to the posteromedial tibia. Long-term rehabilitation for shin splints involves improvement of the flexibility, strength, and endurance of the involved muscles and avoidance of contributing factors. Anterior compartment stretching exercises, Achilles tendon stretching, and overall lower extremity flexibility exercises are important. Eccentric strengthening of antagonistic muscle groups is also useful. Pain can be a guide in the advancement of the rehabilitation program.
Athletes should have full range of motion that is symmetric to the uninvolved side and have nearly full strength before returning to their prior activity or to competition. Plyometrics should be avoided until a high level of strength, endurance, and flexibility has been attained. Cardiovascular fitness should be maintained if possible through lower impact activities, such as stationary biking, swimming, or water running. Return to previous activity level should be a gradual process, individualized, and based on the athlete’s response to increasing intensity of training. Proper footwear for the sport is thought to be essential. Running shoes lose more than 60% of their shock absorption after 250 miles of use [7]. Orthotic devices are often necessary in those individuals with foot abnormalities such as pes planus. More specifically, custom orthotics or shoe inserts can help align and stabilize the foot and ankle, taking stress off the lower leg. A plyometric program of strengthening and conditioning has been suggested as early as the third phase of rehabilitation [23], but return to sport outcomes have not been reported.
Procedures
There is no proven benefit noted in the literature to support any injection-based procedure, such as local exogenous glucocorticoid injection. Limited empirical opinions exist on a role for sclerotherapeutic solutions. Great care must be taken in ensuring the correct diagnosis, as potentially disastrous results may occur in dealing with a coexistent compartment syndrome. Theoretically, a palliative role may exist for either in chronic recalcitrant cases with functional decline. Compartment pressure measurement has no absolute contraindications and can be performed with relative simplicity [24]. Avoidance of areas with overlying cellulitis is recommended. The procedure itself carries some risk of infection, but this can usually be avoided with appropriate technical practices.
Surgery
Surgery is rarely indicated but involves a posteromedial fasciotomy with release of the fascial bridge of the medial soleus and the fascia of the deep posterior compartment, with periosteal cauterization [16]. Surgery is effective in relieving pain, but it frequently leaves the patient with persistent strength deficits, and full return to sports is not always achieved [25].
Potential Disease Complications
If shin splints are not treated and biomechanical malalignments are not addressed, stress fractures and potentially true fractures may occur. This would result in further morbidity and more time lost from the desired physical activity as well as potential function decline. Any chronic tendinopathy can theoretically lead to weakening of the tendon and subsequent rupture [26].
Potential Treatment Complications
Complications involving the gastrointestinal and renal systems may result from treatment with nonsteroidal anti-inflammatory drugs. Fasciotomy may result in residual weakness. Overly aggressive rehabilitation or rehabilitation of the incorrect diagnosis may progress the injury, cause secondary injury, or delay diagnosis of more ominous disease. The author has experience with a case of severe reflex sympathetic dystrophy and peripheral nerve injury after sclerotherapy.







