Procedure 78 Dorsal Plate Fixation and Dorsal Distraction (Bridge) Plating for Distal Radius Fractures
Dorsal Plating of Distal Radius Fractures
Examination/Imaging
Clinical Examination
 Initial examination is usually performed in the emergency department and needs to include mechanism and time of injury, hand dominance, medical comorbidities that may alter treatment, and occupation.
Initial examination is usually performed in the emergency department and needs to include mechanism and time of injury, hand dominance, medical comorbidities that may alter treatment, and occupation.
 Assess whether the fracture is an open or closed injury.
Assess whether the fracture is an open or closed injury.
 Thorough musculoskeletal examination, especially the ipsilateral extremity, is necessary to rule out concomitant injuries.
Thorough musculoskeletal examination, especially the ipsilateral extremity, is necessary to rule out concomitant injuries.
 Identify any associated neurovascular and soft tissue injuries.
Identify any associated neurovascular and soft tissue injuries.
 Identify whether patient has any sign or symptoms of acute median or ulnar nerve injury.
Identify whether patient has any sign or symptoms of acute median or ulnar nerve injury.
Imaging
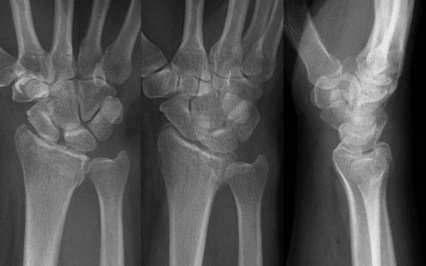
 Initial radiographic evaluation must include posteroanterior, lateral, and oblique views (Fig. 78-1).
Initial radiographic evaluation must include posteroanterior, lateral, and oblique views (Fig. 78-1).
 Assessment must include fracture angulation, displacement, radial shortening, comminution, intra-articular extension, and any ulnar-sided injuries.
Assessment must include fracture angulation, displacement, radial shortening, comminution, intra-articular extension, and any ulnar-sided injuries.
 Combined lesion of a radial styloid with a dorsal marginal or facet fracture (AO type B2.2) is common and can be misdiagnosed as a Colles fracture on lateral radiographs.
Combined lesion of a radial styloid with a dorsal marginal or facet fracture (AO type B2.2) is common and can be misdiagnosed as a Colles fracture on lateral radiographs.
 The lunate facet often has a coronal fracture line that separates this facet into dorsal and volar fragments.
The lunate facet often has a coronal fracture line that separates this facet into dorsal and volar fragments.
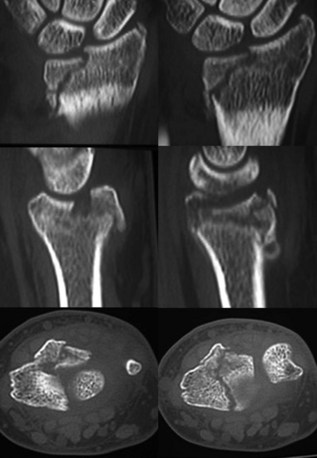
 Computed tomography scan provides excellent delineation of intra-articular extension as well as characterization of fracture comminution for preoperative planning (Fig. 78-2).
Computed tomography scan provides excellent delineation of intra-articular extension as well as characterization of fracture comminution for preoperative planning (Fig. 78-2).
 There is also typically subchondral collapse of the lunate facet that must be addressed to ensure articular reduction.
There is also typically subchondral collapse of the lunate facet that must be addressed to ensure articular reduction.
 Proximal injuries must be ruled out by physical examination and radiographs of the elbow.
Proximal injuries must be ruled out by physical examination and radiographs of the elbow.
Surgical Anatomy
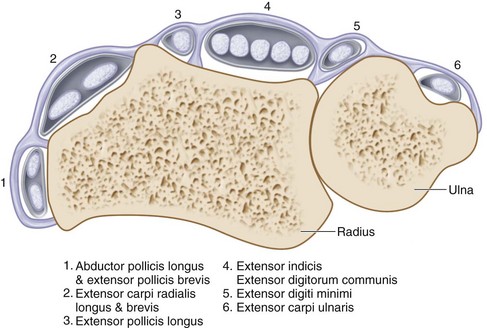
 Knowledge of the anatomic relationships of the extensor retinaculum, six dorsal extensor compartments, and convex dorsoradial cortex is essential for understanding surgical approaches as well as placement of implants on the dorsum of the radius (Fig. 78-3).
Knowledge of the anatomic relationships of the extensor retinaculum, six dorsal extensor compartments, and convex dorsoradial cortex is essential for understanding surgical approaches as well as placement of implants on the dorsum of the radius (Fig. 78-3).
 Extensor retinaculum prevents the extensor tendons from dorsal displacement (bowstringing) and divides the tendons into six extensor compartments by vertical septae.
Extensor retinaculum prevents the extensor tendons from dorsal displacement (bowstringing) and divides the tendons into six extensor compartments by vertical septae.
 The extensor pollicis longus (EPL) tendon, which lies in the third dorsal compartment, passes ulnar to the Lister tubercle and is mobilized during exposure of the dorsal distal radius.
The extensor pollicis longus (EPL) tendon, which lies in the third dorsal compartment, passes ulnar to the Lister tubercle and is mobilized during exposure of the dorsal distal radius.
 The extensor indicis proprius tendon and the extensor digitorum communis tendon lie in the fourth dorsal compartment and are elevated subperiosteally to minimize tendon contact with dorsally placed implants.
The extensor indicis proprius tendon and the extensor digitorum communis tendon lie in the fourth dorsal compartment and are elevated subperiosteally to minimize tendon contact with dorsally placed implants.
 Elevation of the second dorsal compartment, which contains the radial wrist extensors, puts the dorsal sensory branch of the radial nerve and the dorsal radial artery at risk, particularly if the dissection is extended distally.
Elevation of the second dorsal compartment, which contains the radial wrist extensors, puts the dorsal sensory branch of the radial nerve and the dorsal radial artery at risk, particularly if the dissection is extended distally.
 The terminal branch of the posterior interosseous nerve lies on the floor of the fourth dorsal compartment along its radial side; it can be sacrificed, if necessary, without clinical consequence.
The terminal branch of the posterior interosseous nerve lies on the floor of the fourth dorsal compartment along its radial side; it can be sacrificed, if necessary, without clinical consequence.
 The articular surface of the distal radius is biconcave and triangular, with the surface divided into two hyaline covered, concave facets for articulation with the scaphoid and lunate.
The articular surface of the distal radius is biconcave and triangular, with the surface divided into two hyaline covered, concave facets for articulation with the scaphoid and lunate.
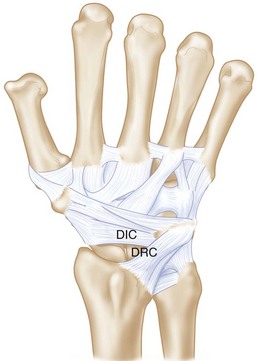
 There are two dorsal ligaments that are intimately associated with the dorsal capsule: the dorsal radiocarpal (DRC) (radiotriquetral) and dorsal intercarpal (DIC) (scaphotriquetral) ligaments (Fig. 78-4).
There are two dorsal ligaments that are intimately associated with the dorsal capsule: the dorsal radiocarpal (DRC) (radiotriquetral) and dorsal intercarpal (DIC) (scaphotriquetral) ligaments (Fig. 78-4).
Exposures
 The dorsal distal radius is approached through a straight, longitudinal incision in line with the third metacarpal and centered just ulnar to the Lister tubercle, between the third and fourth dorsal compartments (Fig. 78-5).
The dorsal distal radius is approached through a straight, longitudinal incision in line with the third metacarpal and centered just ulnar to the Lister tubercle, between the third and fourth dorsal compartments (Fig. 78-5).
 Care is taken to identify and avoid injury to the superficial branch of the radial nerve.
Care is taken to identify and avoid injury to the superficial branch of the radial nerve.
 Full-thickness flaps containing the skin, subcutaneous tissues, and superficial fascia are raised together to expose the extensor retinaculum and the third and fourth dorsal compartments.
Full-thickness flaps containing the skin, subcutaneous tissues, and superficial fascia are raised together to expose the extensor retinaculum and the third and fourth dorsal compartments.
 The third dorsal compartment is longitudinally incised to mobilize the EPL tendon (Fig. 78-6).
The third dorsal compartment is longitudinally incised to mobilize the EPL tendon (Fig. 78-6).
 After mobilizing the EPL, the retinaculum is divided between the septa of the third and fourth dorsal compartments.
After mobilizing the EPL, the retinaculum is divided between the septa of the third and fourth dorsal compartments.
 Using a periosteal elevator or sharp dissection, the fourth compartment is then elevated subperiosteally from the dorsum of the distal radius, keeping the deep surface of the compartment intact.
Using a periosteal elevator or sharp dissection, the fourth compartment is then elevated subperiosteally from the dorsum of the distal radius, keeping the deep surface of the compartment intact.
 The distal radius is exposed sharply by elevation of the periosteum.
The distal radius is exposed sharply by elevation of the periosteum.
 Exposure of the intermediate column requires dissection to continue in an ulnar direction to the distal radioulnar joint (DRUJ).
Exposure of the intermediate column requires dissection to continue in an ulnar direction to the distal radioulnar joint (DRUJ).
 A longitudinal capsulotomy may be needed to expose the distal radius articular surface, which requires detaching the dorsal capsular insertions on the distal nonarticular lunate.
A longitudinal capsulotomy may be needed to expose the distal radius articular surface, which requires detaching the dorsal capsular insertions on the distal nonarticular lunate.
Pearls
Large, longitudinal veins should be preserved if possible, but crossing veins may be divided.
Full-thickness flaps will contain the dorsal sensory branches of the ulnar and radial nerve and protect them.
Subperiosteal elevation of the fourth compartment minimizes implant contact with the extensor tendons.
Pitfalls
If the distal extension of the incision is past the base of the third metacarpal, the dorsal sensory branches of both the radial and ulnar nerves are at risk.
The EPL tendon is left above the retinaculum at closure to minimize the risk for tendon injury by ischemia or direct contact with an implant.
Care must be exercised not to enter the DRUJ. If the dorsal radioulnar ligament is divided during ulnar dissection, radioulnar instability can result.
The intercarpal ligaments must be protected during capsulotomy.
Procedure
Dorsal Plate Fixation for Distal Radius Fractures
Step 1: Reduction of Dorsally Angulated Fractures
 Once the proximal fracture lines and articular surface are exposed and assessed, all hematoma is evacuated.
Once the proximal fracture lines and articular surface are exposed and assessed, all hematoma is evacuated.
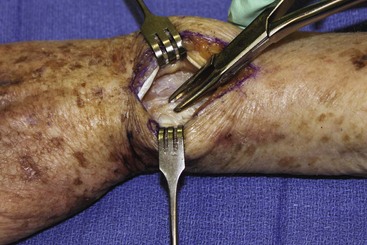
 Lister tubercle is removed with a rongeur or small osteotome (Fig. 78-7).
Lister tubercle is removed with a rongeur or small osteotome (Fig. 78-7).
 Reduction of the dorsal angulation can be performed with the use of narrow-angled Homan retractors along the proximal fragment.
Reduction of the dorsal angulation can be performed with the use of narrow-angled Homan retractors along the proximal fragment.
 With gentle traction and lifting of the bone retractors, reduction of the dorsal angulation can be achieved.
With gentle traction and lifting of the bone retractors, reduction of the dorsal angulation can be achieved.
 Provisional fixation with Kirschner wires (0.045-in.) can be used to hold the reduction and is checked fluoroscopically.
Provisional fixation with Kirschner wires (0.045-in.) can be used to hold the reduction and is checked fluoroscopically.
Step 2: Fixation of Dorsally Angulated Fractures
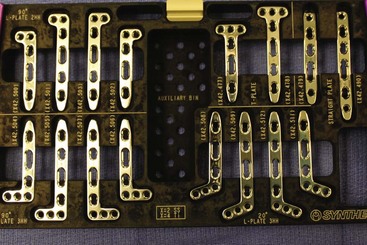
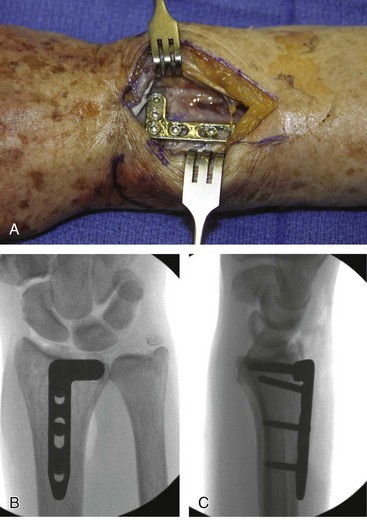
 After satisfactory reduction is performed, a 2.4-mm low-profile dorsal T-plate (Fig. 78-8) can be placed directly over the dorsal surface of the distal radius.
After satisfactory reduction is performed, a 2.4-mm low-profile dorsal T-plate (Fig. 78-8) can be placed directly over the dorsal surface of the distal radius.
 Preliminary fixation of the plate with a single, bicortical compression screw placed in the oblong hole of the plate will allow for proximal-distal adjustments in plate position as determined clinically and fluoroscopically.
Preliminary fixation of the plate with a single, bicortical compression screw placed in the oblong hole of the plate will allow for proximal-distal adjustments in plate position as determined clinically and fluoroscopically.
 It is important to provisionally bend the plate to fit the contour of the dorsal radial cortex so that the plate lies flush with the dorsal cortex.
It is important to provisionally bend the plate to fit the contour of the dorsal radial cortex so that the plate lies flush with the dorsal cortex.
 Although several options for plating are available, including locking and nonlocking plates, one must consider contouring a fixed-angle plate by threading a locking guide into the plate before contouring; this will avoid damage to the threads of the locking mechanism.
Although several options for plating are available, including locking and nonlocking plates, one must consider contouring a fixed-angle plate by threading a locking guide into the plate before contouring; this will avoid damage to the threads of the locking mechanism.
 The final placement is checked by fluoroscopy in anteroposterior and lateral views to confirm proper positioning of the plate.
The final placement is checked by fluoroscopy in anteroposterior and lateral views to confirm proper positioning of the plate.
 Three to five 2.7-mm screws are then placed bicortically along the distal row of the plate, using fluoroscopy to confirm placement.
Three to five 2.7-mm screws are then placed bicortically along the distal row of the plate, using fluoroscopy to confirm placement.
 Two additional proximal screws are then inserted bicortically, and final fluoroscopic assessment is performed.
Two additional proximal screws are then inserted bicortically, and final fluoroscopic assessment is performed.
Step 3: Reduction and Fixation of Dorsal Marginal Fractures
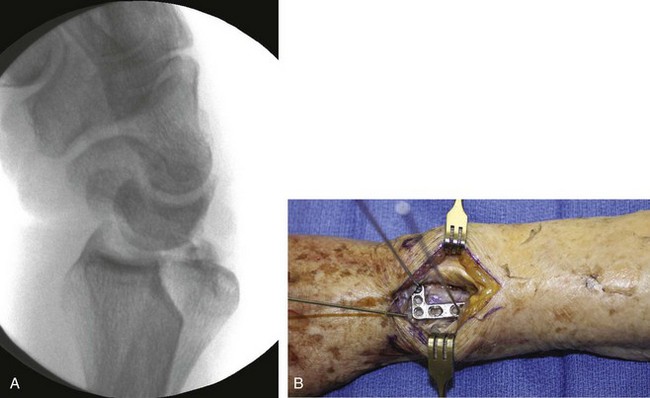
 It is important to assess carpal subluxation and initially restore the radial styloid fragment if present (Fig. 78-9A).
It is important to assess carpal subluxation and initially restore the radial styloid fragment if present (Fig. 78-9A).
 This reduction is usually accomplished with traction and ulnar deviation of the hand and wrist, and then provisional K-wire fixation (Figs. 78-9B and 78-10).
This reduction is usually accomplished with traction and ulnar deviation of the hand and wrist, and then provisional K-wire fixation (Figs. 78-9B and 78-10).
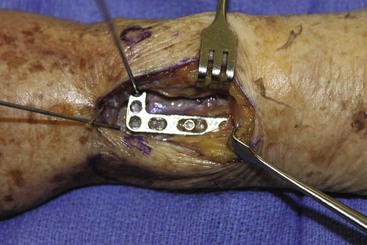
 Once the appropriate-sized 2.4-mm plate has been contoured, the locking screw guide is placed in the proximal screw hole and is used to hold and contour the plate.
Once the appropriate-sized 2.4-mm plate has been contoured, the locking screw guide is placed in the proximal screw hole and is used to hold and contour the plate.
 Preliminary fixation of the plate with a single, bicortical screw placed in the oblong hole will allow for proximal-distal plate adjustments as determined clinically and fluoroscopically (Fig. 78-11).
Preliminary fixation of the plate with a single, bicortical screw placed in the oblong hole will allow for proximal-distal plate adjustments as determined clinically and fluoroscopically (Fig. 78-11).
 A provisional K-wire is then placed through the threaded locking guide at the distal end of the plate but not into the radius to facilitate quick placement after reduction of the carpus.
A provisional K-wire is then placed through the threaded locking guide at the distal end of the plate but not into the radius to facilitate quick placement after reduction of the carpus.
 The dorsal lip or marginal fracture can be reduced now against the scaphoid and lunate, which will correct any associated dorsal carpal subluxation.
The dorsal lip or marginal fracture can be reduced now against the scaphoid and lunate, which will correct any associated dorsal carpal subluxation.
 The marginal fracture will then be provisionally fixed into the volar cortex through the provisional K-wire that had been previously placed into the threaded locking guide at the distal end of the plate.
The marginal fracture will then be provisionally fixed into the volar cortex through the provisional K-wire that had been previously placed into the threaded locking guide at the distal end of the plate.
 Congruity of the articular surface must be confirmed with direct visualization as well as fluoroscopically.
Congruity of the articular surface must be confirmed with direct visualization as well as fluoroscopically.
 If the plate is acting purely as a buttress, distal locking screws are not necessary.
If the plate is acting purely as a buttress, distal locking screws are not necessary.
 If additional fixation for stability is necessary, 2.4-mm screws are then placed bicortically along the distal row of the plate, using fluoroscopy to confirm placement.
If additional fixation for stability is necessary, 2.4-mm screws are then placed bicortically along the distal row of the plate, using fluoroscopy to confirm placement.
 One or two additional bicortical screws are placed proximally to the proximal extent of the fracture to finalize construct (Figure 78-12).
One or two additional bicortical screws are placed proximally to the proximal extent of the fracture to finalize construct (Figure 78-12).
Step 3 Pitfalls
Failure to recognize styloid component or any volar-ulnar fragments will lead to incongruity of articular surface and radiocarpal arthrosis.
These fractures may be associated with dorsal radiocarpal subluxation, volar ligament injuries, articular surface impaction, and avulsion fractures.
All bicortical fixations should be checked radiographically to ensure that they are not prominent volarly.
Step 4: Reduction and Fixation of Lunate Facet Fractures
 Subchondral collapse of the lunate facet can be addressed with the use of a Freer elevator or dental pick placed into the facet fracture line in the metaphysic.
Subchondral collapse of the lunate facet can be addressed with the use of a Freer elevator or dental pick placed into the facet fracture line in the metaphysic.
 The lunate facet fragment is then manually reduced by elevating the depressed surface and checked both by fluoroscopy and directly if an arthrotomy has been made to ensure adequate reduction.
The lunate facet fragment is then manually reduced by elevating the depressed surface and checked both by fluoroscopy and directly if an arthrotomy has been made to ensure adequate reduction.
 A provisional K-wire can be placed along the subchondral surface from the radial styloid to the sigmoid notch to act as a buttress for the reduced lunate facet fracture.
A provisional K-wire can be placed along the subchondral surface from the radial styloid to the sigmoid notch to act as a buttress for the reduced lunate facet fracture.
 For provisional reduction of coronal facet fractures, temporary K-wires can also be placed to stabilize the coronal fracture line.
For provisional reduction of coronal facet fractures, temporary K-wires can also be placed to stabilize the coronal fracture line.
 For sagittal splits, intrafragmentary compression is possible using a large bone reduction clamp.
For sagittal splits, intrafragmentary compression is possible using a large bone reduction clamp.
 One point of the clamp is placed along the ulnar border of the lunate facet, one point is placed along the radial styloid, and after compression of the clamp, a transverse provisional K-wire is placed to hold reduction.
One point of the clamp is placed along the ulnar border of the lunate facet, one point is placed along the radial styloid, and after compression of the clamp, a transverse provisional K-wire is placed to hold reduction.
 When an impacted fragment is elevated, there will often be a metaphyseal void that must be filled with cancellous allograft or bone graft substitute to support the articular surface.
When an impacted fragment is elevated, there will often be a metaphyseal void that must be filled with cancellous allograft or bone graft substitute to support the articular surface.
 After preliminary reduction is confirmed both by direct visualization and fluoroscopy, an L-shaped 2.4-mm plate is typically used for buttress fixation of the intermediate column and articular surface (see Fig. 78-8).
After preliminary reduction is confirmed both by direct visualization and fluoroscopy, an L-shaped 2.4-mm plate is typically used for buttress fixation of the intermediate column and articular surface (see Fig. 78-8).
 The dorsoulnar plate usually needs to be contoured to allow placement along the dorsoulnar aspect of the distal part of the radius.
The dorsoulnar plate usually needs to be contoured to allow placement along the dorsoulnar aspect of the distal part of the radius.
 The plate is then fixed proximally to the shaft well distally along the L-portion of the plate.
The plate is then fixed proximally to the shaft well distally along the L-portion of the plate.
 It is especially important to obtain bicortical screw fixation along the ulnar side of the radius if there is a coronal split in the facet because it is vital to obtain compression of the volar ulnar fragment.
It is especially important to obtain bicortical screw fixation along the ulnar side of the radius if there is a coronal split in the facet because it is vital to obtain compression of the volar ulnar fragment.
 If stable fixation cannot be obtained with only a dorsal approach, a volar approach between the FCR and radial artery may be used to stabilize the volar cortex.
If stable fixation cannot be obtained with only a dorsal approach, a volar approach between the FCR and radial artery may be used to stabilize the volar cortex.
 If this fails, an external fixator can be applied.
If this fails, an external fixator can be applied.
 The wrist is taken through a range of motion, including flexion, extension, supination, and pronation, to ensure clinical stability.
The wrist is taken through a range of motion, including flexion, extension, supination, and pronation, to ensure clinical stability.
Step 4 Pearls
If there are nonarticular fragments seen along the dorsal aspects of the scaphoid and lunate facet that still have capsular attachments, an effort should be made to save them with their attachments.
Bone grafting metaphyseal defects after elevation of depressed articular fragments is essential to maintain reduction.
Step 5: Assessment of DRUJ Stability and Wound Closure
 After stabilization of the radius, any instability of the DRUJ should be assessed (defined as greater than 8 mm of palmar to dorsal translation of the ulna relative to the radius).
After stabilization of the radius, any instability of the DRUJ should be assessed (defined as greater than 8 mm of palmar to dorsal translation of the ulna relative to the radius).
 Large fractures of the ulnar styloid, as well as displaced ulnar head fractures, should raise suspicions of instability.
Large fractures of the ulnar styloid, as well as displaced ulnar head fractures, should raise suspicions of instability.
 If instability is noted, consideration should be given to a closed reduction and percutaneous pinning of the DRUJ with the forearm maintained in supination.
If instability is noted, consideration should be given to a closed reduction and percutaneous pinning of the DRUJ with the forearm maintained in supination.
 If no instability is noted, no immobilization is necessary.
If no instability is noted, no immobilization is necessary.
 If an arthrotomy has been made, the dorsal capsule should be closed with 3-0 nonabsorbable suture.
If an arthrotomy has been made, the dorsal capsule should be closed with 3-0 nonabsorbable suture.
 The extensor retinaculum should be repaired with interrupted 2-0 absorbable suture, making sure the EPL tendon remains in its transposed position superficial to the retinaculum.
The extensor retinaculum should be repaired with interrupted 2-0 absorbable suture, making sure the EPL tendon remains in its transposed position superficial to the retinaculum.
 After wound irrigation, the skin should be closed with either nylon or Prolene sutures in an interrupted fashion.
After wound irrigation, the skin should be closed with either nylon or Prolene sutures in an interrupted fashion.
Postoperative Care and Expected Outcomes
 A bulky sterile dressing and volar splint, leaving the thumb and fingers free, is applied for postoperative comfort for 7 to 10 days (except in those with DRUJ instability).
A bulky sterile dressing and volar splint, leaving the thumb and fingers free, is applied for postoperative comfort for 7 to 10 days (except in those with DRUJ instability).
 After removal of dressing, active and passive digital range-of-motion exercises are initiated.
After removal of dressing, active and passive digital range-of-motion exercises are initiated.
 A custom, short-arm volar splint is applied in neutral position, which can be removed five to seven times daily to perform active wrist range-of-motion exercises.
A custom, short-arm volar splint is applied in neutral position, which can be removed five to seven times daily to perform active wrist range-of-motion exercises.
 An elastic garment should be used to control postoperative edema.
An elastic garment should be used to control postoperative edema.
 Weaning of splint for activities of daily living can be started at 4 weeks.
Weaning of splint for activities of daily living can be started at 4 weeks.
 After clinical and radiographic evidence of fracture healing is seen (6 to 8 weeks), the splint is discontinued completely.
After clinical and radiographic evidence of fracture healing is seen (6 to 8 weeks), the splint is discontinued completely.
Dorsal Distraction (Bridge) Plating
Indications
 Highly comminuted, articular distal radius fractures as well as those associated with significant metaphyseal and diaphyseal comminution
Highly comminuted, articular distal radius fractures as well as those associated with significant metaphyseal and diaphyseal comminution
 Polytrauma patients to facilitate activities of daily living
Polytrauma patients to facilitate activities of daily living
 Extensive tendon injuries that may require multiple procedures and an extended period of time for soft tissue and osseous healing
Extensive tendon injuries that may require multiple procedures and an extended period of time for soft tissue and osseous healing
 Severe osteoporosis in which fracture fixation is expected to be poor
Severe osteoporosis in which fracture fixation is expected to be poor
 Patients who refuse external fixation for psychological or aesthetic concerns
Patients who refuse external fixation for psychological or aesthetic concerns
Examination/Imaging
Imaging
 Initial plain radiographic evaluation must include posteroanterior, lateral, and oblique views (Figs. 78-13 and 78-14).
Initial plain radiographic evaluation must include posteroanterior, lateral, and oblique views (Figs. 78-13 and 78-14).
 Ulnar deviation views can be used in patients with suspected scaphoid fractures.
Ulnar deviation views can be used in patients with suspected scaphoid fractures.
 Proximal injuries must be ruled out with radiographs of the elbow and forearm.
Proximal injuries must be ruled out with radiographs of the elbow and forearm.
 Computed tomography scan provides excellent delineation of intra-articular extension as well as characterization of fracture comminution for operative planning (Fig. 78-15).
Computed tomography scan provides excellent delineation of intra-articular extension as well as characterization of fracture comminution for operative planning (Fig. 78-15).
Surgical Anatomy
 The EPL tendon should be released from its compartment and freed from its groove to prevent injury or impingement of the plate onto the tendon if an open articular reduction is necessary.
The EPL tendon should be released from its compartment and freed from its groove to prevent injury or impingement of the plate onto the tendon if an open articular reduction is necessary.
 The plate should pass superficial to the joint capsule and periosteum and within the second dorsal compartment, occupied by the extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB).
The plate should pass superficial to the joint capsule and periosteum and within the second dorsal compartment, occupied by the extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB).
 The extensor tendons over the index finger metacarpal must be identified and retracted to facilitate distal fixation.
The extensor tendons over the index finger metacarpal must be identified and retracted to facilitate distal fixation.
 The proximal portion of the plate will be placed along the dorsoradial aspect of the radial shaft adjacent to the brachioradialis and outcropping muscles.
The proximal portion of the plate will be placed along the dorsoradial aspect of the radial shaft adjacent to the brachioradialis and outcropping muscles.
 The superficial branch of the radial nerve is at risk during the proximal dissection of the radial shaft.
The superficial branch of the radial nerve is at risk during the proximal dissection of the radial shaft.
Exposures
 The exposure involves two or three dorsal incisions and is performed under tourniquet control (Fig. 78-16).
The exposure involves two or three dorsal incisions and is performed under tourniquet control (Fig. 78-16).
 A 4-cm incision is made dorsally over the midpart of the shaft of the index finger metacarpal, with the extensor tendons identified and retracted.
A 4-cm incision is made dorsally over the midpart of the shaft of the index finger metacarpal, with the extensor tendons identified and retracted.
 A second 4- to 6-cm incision is made on the dorsoradial aspect of the radial shaft, just proximal to the outcropping muscle bellies (extensor pollicis brevis and abductor pollicis longus).
A second 4- to 6-cm incision is made on the dorsoradial aspect of the radial shaft, just proximal to the outcropping muscle bellies (extensor pollicis brevis and abductor pollicis longus).
 The interval between the ECRL and ECRB is used to expose the radial diaphysis.
The interval between the ECRL and ECRB is used to expose the radial diaphysis.
 The surgeon must expose enough radial shaft to secure three screws proximal to the fracture site, no less than 4 cm proximal to the most proximal comminuted segment.
The surgeon must expose enough radial shaft to secure three screws proximal to the fracture site, no less than 4 cm proximal to the most proximal comminuted segment.
 A third incision, about 3 cm in length over the Lister tubercle, can be made if an articular reduction or bone graft is necessary; the EPL is mobilized to facilitate reduction.
A third incision, about 3 cm in length over the Lister tubercle, can be made if an articular reduction or bone graft is necessary; the EPL is mobilized to facilitate reduction.
Pearls
Placement of incisions is facilitated with fluoroscopic guidance.
The surgeon holds the distal end of the plate at the index metacarpal neck-shaft junction and identifies the proximal extent of the plate over the radial shaft to ensure placement of three screws proximal to the fracture.
The third incision also allows for exposure of the fracture when necessary, permitting metaphyseal bone grafting and articular reduction.
Procedure
Dorsal Distraction (Bridge) Plating
Step 1: Selection of an Appropriate-Length Plate
 A 20-hole, 2.4-mm Distal Radius Bridge Plate (Synthes, Paoli, PA) is used (Fig. 78-17).
A 20-hole, 2.4-mm Distal Radius Bridge Plate (Synthes, Paoli, PA) is used (Fig. 78-17).
 If this custom plate is not available, a 2.7- or 3.5-mm limited contact dynamic compression plate (LC-DCP) can be substituted.
If this custom plate is not available, a 2.7- or 3.5-mm limited contact dynamic compression plate (LC-DCP) can be substituted.
 Under fluoroscopic guidance, hold the distal end of the plate at the metacarpal neck and identify the proximal extent of the plate over the radial shaft to allow the placement of three screws proximal to the fracture.
Under fluoroscopic guidance, hold the distal end of the plate at the metacarpal neck and identify the proximal extent of the plate over the radial shaft to allow the placement of three screws proximal to the fracture.
Step 2: Retrograde Passage of the Plate
 After exposures have been made, a periosteal elevator or long Metzenbaum scissors is carefully inserted proximal to distal along the floor of the second compartment to create a tunnel between the extensor tendons and the periosteum and joint capsule (Fig. 78-18).
After exposures have been made, a periosteal elevator or long Metzenbaum scissors is carefully inserted proximal to distal along the floor of the second compartment to create a tunnel between the extensor tendons and the periosteum and joint capsule (Fig. 78-18).
 The plate should lie superficial to the periosteum and along the floor of the second dorsal compartment.
The plate should lie superficial to the periosteum and along the floor of the second dorsal compartment.
 The plate is then passed from the distal to proximal incision under the index finger extensor tendons (Fig. 78-19).
The plate is then passed from the distal to proximal incision under the index finger extensor tendons (Fig. 78-19).
Step 2 Pearls
Retraction of the ECRB and ECRL in the proximal wound will allow for visualization of the radial shaft and the periosteal elevator so that long scissors can be passed subperiosteally.
The trajectory of the plate is parallel to the radial aspect of the undersurface of the extensor tendons to the index finger.
Step 3: Initial Plate Fixation to the Index Metacarpal
 The fracture is initially reduced with manual traction of the wrist.
The fracture is initially reduced with manual traction of the wrist.
 Using fluoroscopy, the plate is then aligned centrally over the index metacarpal distally and the radial shaft proximally.
Using fluoroscopy, the plate is then aligned centrally over the index metacarpal distally and the radial shaft proximally.
 A bicortical screw is placed in the second-to-last hole in the center of the metacarpal shaft.
A bicortical screw is placed in the second-to-last hole in the center of the metacarpal shaft.
Step 3 Pearls
Using only a single screw will allow, if necessary, slight adjustments of the plate position for fracture reduction and plate alignment.
To avoid possible rotary displacement of the hand in relation to the shaft, it is important to obtain provisional reduction of both radial inclination and length before securing the plate to the metacarpal shaft.
Step 4: Plate Fixation to the Radial Shaft
 Reapply traction to the arm to restore radial length and confirm alignment with fluoroscopy.
Reapply traction to the arm to restore radial length and confirm alignment with fluoroscopy.
 Maintain traction, centralize the proximal portion of plate over the radial shaft, and clamp the plate to the proximal radial shaft using serrated bone-holding clamps.
Maintain traction, centralize the proximal portion of plate over the radial shaft, and clamp the plate to the proximal radial shaft using serrated bone-holding clamps.
 Reassess the fracture alignment using fluoroscopy to ensure restoration of radial length, inclination, and palmar tilt.
Reassess the fracture alignment using fluoroscopy to ensure restoration of radial length, inclination, and palmar tilt.
 Perform a clinical as well as a fluoroscopic assessment to ensure proper fracture alignment and absence of rotational abnormalities.
Perform a clinical as well as a fluoroscopic assessment to ensure proper fracture alignment and absence of rotational abnormalities.
 Three bicortical proximal screws are placed in the shaft to secure the plate.
Three bicortical proximal screws are placed in the shaft to secure the plate.
 Two additional bicortical screws are applied to the metacarpal shaft to ensure three distal points of fixation (Fig. 78-20).
Two additional bicortical screws are applied to the metacarpal shaft to ensure three distal points of fixation (Fig. 78-20).
 Final radiographic assessment is repeated to ensure maintenance of reduction (Fig. 78-21).
Final radiographic assessment is repeated to ensure maintenance of reduction (Fig. 78-21).
Step 4 Pearls
Assess supination and pronation of the forearm with the plate clamped proximally to the radial shaft to confirm a full range of motion.
It is very helpful to maintain the arm in 45 to 60 degrees of supination while maintaining distraction before the serrated clamp is applied proximally to avoid pronation of the distal fragment.
Once plate placement has been determined with at least one proximal and distal screw, locking screws can be used, particularly in osteopenic bone.
Step 4 Pitfalls
Overdistraction (defined as a radiocarpal space greater than 5 mm) must be avoided to prevent possible permanent loss of finger range of motion as well as the potential development of complex regional pain syndrome.
Extrinsic extensor tightness can also develop with overdistraction; it is vital to ensure full passive digital range of motion after plate fixation.
Step 5: Fixation of the Articular Surface and Diaphyseal Fragments (if Necessary)
 If there are any diaphyseal fragments that are amenable to lag screw fixation to the shaft, this can be performed at this time.
If there are any diaphyseal fragments that are amenable to lag screw fixation to the shaft, this can be performed at this time.
 Reduction of the articular surface can be performed through the third incision used to free the EPL tendon and pass the plate proximally.
Reduction of the articular surface can be performed through the third incision used to free the EPL tendon and pass the plate proximally.
 Using a dental pick or Freer elevator, the articular incongruity can be reduced through an empty hole in the plate or adjacent to the plate.
Using a dental pick or Freer elevator, the articular incongruity can be reduced through an empty hole in the plate or adjacent to the plate.
 Subchondral and metaphyseal support for maintaining articular reduction can be achieved with allograft or bone graft substitute.
Subchondral and metaphyseal support for maintaining articular reduction can be achieved with allograft or bone graft substitute.
 When feasible, a 2.7-mm cortical screw is then inserted through the plate directly under the lunate fossa to act as a buttress against subchondral collapse.
When feasible, a 2.7-mm cortical screw is then inserted through the plate directly under the lunate fossa to act as a buttress against subchondral collapse.
 K-wires (0.45 or 0.62 inch) can also be placed percutaneously to hold small articular fragments reduced.
K-wires (0.45 or 0.62 inch) can also be placed percutaneously to hold small articular fragments reduced.
 Case series: Posteroanterior radiograph of another case (Fig. 78-22A)
Case series: Posteroanterior radiograph of another case (Fig. 78-22A)
 Case series: Radiographs of the plate bridging the fracture (Fig. 78-22B).
Case series: Radiographs of the plate bridging the fracture (Fig. 78-22B).
Step 5 Pearls
It is absolutely essential to address any depressed articular fragments that do not reduce with ligamentotaxis.
Bone grafting for both subchondral and metaphyseal defects that are magnified or created by the distraction is an essential component for long-term maintenance of articular reduction and fracture healing.
K-wires should be left outside or deep to the skin and removed at 6 weeks.
Step 5 Pitfalls
Failure to reduce articular fragments may lead to symptomatic radiocarpal arthrosis.
Use of the nick-and-spread method to insert percutaneous K-wire fixation is imperative to prevent injury to the branches of the superficial radial nerve.
Contraindications to bone grafting include grade III open fractures with gross contamination and soft tissue defects that preclude primary wound closure.
After stabilization of the radius, any instability of the DRUJ should be assessed (defined as greater than 8 mm of palmar to dorsal translation of the ulna relative to the radius).
Large fractures of the ulnar styloid as well as displaced ulnar head fractures should raise suspicions of instability.
If instability is noted, the forearm should be maintained in supination for 3 to 4 weeks.
If no instability is noted, immobilization is unnecessary.
If an arthrotomy has been made, the dorsal capsule should be closed with 3-0 nonabsorbable suture.
Postoperative Care and Expected Outcomes
 A bulky dressing and splint are used postoperatively for pain control for a few days (except in those with DRUJ instability).
A bulky dressing and splint are used postoperatively for pain control for a few days (except in those with DRUJ instability).
 Active and passive digital range-of-motion exercises are started immediately and maintained throughout the distraction period.
Active and passive digital range-of-motion exercises are started immediately and maintained throughout the distraction period.
 After the first postoperative visit at 7 to 10 days, a thermoplastic short-arm splint is applied, and an elastic garment is applied to control edema.
After the first postoperative visit at 7 to 10 days, a thermoplastic short-arm splint is applied, and an elastic garment is applied to control edema.
 Pronation and supination are encouraged.
Pronation and supination are encouraged.
 Patients may use the affected extremity for activities of daily living.
Patients may use the affected extremity for activities of daily living.
 Patients may not lift greater than 5 pounds.
Patients may not lift greater than 5 pounds.
 As noted by Hanel and colleagues (2006), the duration of plate immobilization does not correlate with the range of motion of the wrist or with the DASH score at 1 year.
As noted by Hanel and colleagues (2006), the duration of plate immobilization does not correlate with the range of motion of the wrist or with the DASH score at 1 year.
Pearls
Patients may return to work with distraction in place if they can maintain their restrictions.
A platform walker for mobilization may be used in polytrauma patients if the fixation is deemed stable enough intraoperatively.
Hardware removal can electively be scheduled for about 8 to 12 weeks after surgery depending on the nature of the fracture and documentation of radiographic union.
Range-of-motion exercises of the wrist and fingers are started immediately after plate removal, and no splinting is required.
Pitfalls
Maintain distraction plate until radiographic osseous healing has occurred (bridging callous seen in both the coronal and sagittal plane).
Judging osseous healing may be difficult to visualize with the 3.5-mm plate.
Early removal may lead to late fracture collapse.
Late removal can lead to possible extensor tendon attrition and rupture and permanent wrist stiffness.
Burke EF, Singer RM. Treatment of comminuted distal radius with the use of an internal distraction plate. Tech Hand Upper Extrem Surg. 1998;2:248-252.
Carter PR, Frederick HA, Georgiann FL. Open reduction and internal fixation of unstable distal radius fractures with a low-profile plate: a multicenter study of 73 fractures. J Hand Surg [Am]. 1998;23:300-307.
Ginn TA, Ruch DS, Yang CC, Hanel DP. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution: surgical technique. J Bone Joint Surg [Am]. 2006;88:29-36.
Hanel DP, Lu TS, Weil WM. Bridge plating of distal radius fractures: the Harborview method. Clin Orthop Relat Res. 2006;445:91-99.
Kamath AF, Zurakowski D, Day CS. Low-profile dorsal plating for dorsally angulated distal radius fractures: an outcomes study. J Hand Surg [Am]. 2006;31:1061-1067.
Lozano-Calderón SA, Doornberg J, Ring D. Fractures of the dorsal articular margin of the distal part of the radius with dorsal radiocarpal subluxation. J Bone Joint Surg [Am]. 2006;88:1486-1493.
Papadonikolakis A, Ruch DS. Internal distraction plating of distal radius fractures. Tech Hand Upper Extrem Surg. 2005;9:2-6.
Rozental TD, Beredjiklian PK, Bozentka DJ. Functional outcome and complications following two types of dorsal plating for unstable fractures of the distal part of the radius. J Bone Joint Surg [Am]. 2003;85:1956-1960.
Ruch DS, Ginn TA, Yang CC, et al. Use of a distraction plate for distal radial fractures. J Bone Joint Surg [Am]. 2005;87:945-954.
Simic PM, Robison J, Gardner MJ, et al. Treatment of distal radius fractures with a low-profile dorsal plating system: an outcomes assessment. J Hand Surg [Am]. 2006;31:382-386.