CASE 78

1. What should be included in the differential diagnosis? (Choose all that apply.)
A. Amyloidosis
B. Myocarditis
C. Infarction
D. Sarcoidosis
2. What is the most likely diagnosis in the presence of paratracheal and symmetric hilar lymphadenopathy?
A. Amyloidosis
B. Myocarditis
D. Sarcoidosis
3. What is the most likely diagnosis if the patient’s chest radiograph was clear and her chest pain started after a viral illness?
A. Amyloidosis
B. Myocarditis
C. Infarction
D. Sarcoidosis
4. What is the significance of late gadolinium enhancement in myocarditis?
A. Fibrosis
C. Hyperemia
D. Edema
ANSWERS
References
Deux JF, Maatouk M, Lim P, et al. Acute myocarditis: diagnostic value of contrast-enhanced cine steady-state free precession MRI sequences. AJR Am J Roentgenol. 2011;197(5):1081–1087.
Feldman AM, McNamara D. Myocarditis. N Engl J Med. 2000;343(19):1388–1398.
Friedrich MG, Sechtem U, Schulz-Menger J, et al. Cardiovascular magnetic resonance in myocarditis: a JACC White Paper. J Am Coll Cardiol. 2009;53(17):1475–1487.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 91–92, 292–294.
Comment
Imaging
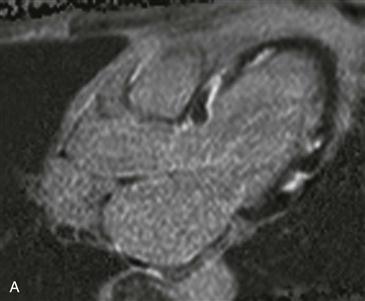
Late gadolinium enhancement four-chamber and short-axis images show patchy enhancement in the left ventricle with sparing of the endocardium (Figs. A and B). The differential diagnosis includes myocarditis or sarcoidosis. Amyloidosis is possible if the patient presented with symptoms of restrictive cardiomyopathy. This patient was diagnosed with myocarditis after excluding sarcoidosis.
Description
Myocarditis represents inflammation of myocardial tissue. It most commonly follows a viral infection and is usually seen in previously healthy patients. It is an important cause of sudden cardiac death in young patients and is a recognized cause of dilated cardiomyopathy. Endomyocardial biopsy is considered the gold standard for diagnosis, but it is invasive and may be negative owing to sampling error.
Diagnosis with MRI
MRI is a noninvasive technique that aids in the diagnosis of myocarditis in the correct clinical setting. MRI identifies the disease in 30% of patients with chest pain, elevated troponin, and clinically normal coronary arteries. There are three findings that occur with myocarditis:
Test sensitivity and specificity for diagnosing myocarditis increase with more positive findings (i.e., T2 hyperintensity, early gadolinium enhancement, and late gadolinium enhancement).
Prognosis
Late gadolinium enhancement occurring 4 weeks after the acute episode has shown prognostic value in predicting poor functional and clinical outcomes. A reduced ejection fraction and right ventricular involvement are echocardiographic markers of an increased risk for sudden cardiac death and future need for cardiac transplantation. Patients with myocarditis are usually treated supportively with heart failure and arrhythmia management. Immunosuppressive therapy is initiated when myocarditis results from an autoimmune disease.