CASE 76

1. What should be included in the differential diagnosis for the cardiac findings? (Choose all that apply.)
A. Myocarditis
B. Infarction
C. Ischemia
E. Sarcoidosis
2. What is the high-resolution chest CT finding?
A. Nodules
B. Masses
3. Which pattern best describes the distribution of the lung nodules?
A. Random
B. Tree-in-bud
4. What is the likely diagnosis?
A. Myocarditis
B. Hypertrophic cardiomyopathy
C. Sarcoidosis
D. Amyloidosis
ANSWERS
References
Smedema JP, Snoep G, van Kroonenburgh MP, et al. Evaluation of the accuracy of gadolinium-enhanced cardiovascular magnetic resonance in the diagnosis of cardiac sarcoidosis. J Am Coll Cardiol. 2005;45(10):1683–1690.
Youssef G, Beanlands RS, Birnie DH, et al. Cardiac sarcoidosis: applications of imaging in diagnosis and directing treatment. Heart. 2011;97(24):2078–2087.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 89, 92.
Comment
Imaging
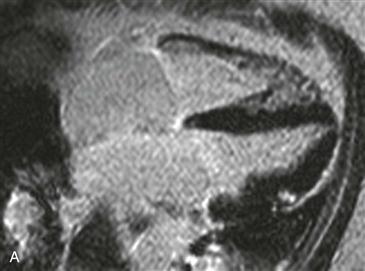
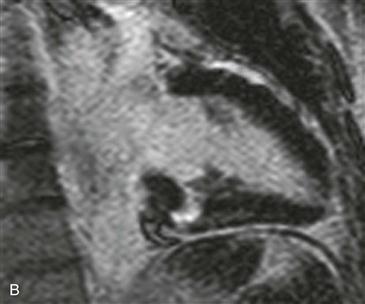
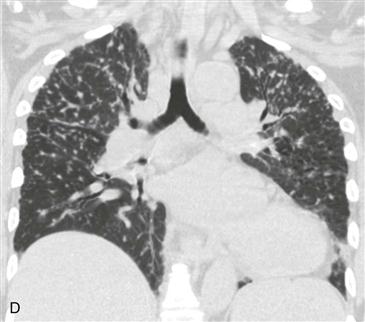
Two inversion recovery late gadolinium enhancement images show nodular enhancing foci that spare the subendocardium (Figs. A and B). The main differential diagnostic considerations include several nonischemic cardiomyopathies (i.e., myocarditis, sarcoidosis, amyloidosis). Chest CT scan shows a perilymphatic distribution of lung nodules with a mid to upper zone predominance (Figs. C and D). Putting these two findings together, the most likely diagnosis is sarcoidosis.
Modalities Used to Diagnose Myocardial Sarcoidosis
Sarcoidosis is an idiopathic disease characterized by the presence of noncaseating granulomas. MRI, PET/CT, and gallium and thallium nuclear imaging can be useful in the diagnosis of cardiac involvement. MRI is a particularly robust technique because of the absence of ionizing radiation and the ability to guide endomyocardial biopsy to appropriate areas of active disease. MRI can assess treatment response after initiation of corticosteroids or immunomodulator therapy.
Diagnosis
The diagnosis is difficult in the absence of known pulmonary sarcoidosis. MRI findings of active disease include patchy and nodular T2 hyperintensity with focal wall thickening and late gadolinium enhancement in involved myocardium. Scarring, fibrosis, and wall thinning identify the chronic form of disease. The patchy myocardial enhancement in sarcoidosis often spares the subendocardium and does not follow a vascular distribution.
Cardiomyopathy
Myocardial sarcoidosis can cause a restrictive cardiomyopathy. The left ventricular myocardium has increased stiffness (reduced compliance) leading to poor diastolic filling and reduced cardiac output. Systolic function is often preserved or mildly decreased. Clinically, patients may present with constrictive or restrictive physiology with dyspnea on exertion, lower extremity edema, ascites, and equalization of cardiac chamber pressures. MRI can differentiate restrictive cardiomyopathy from constrictive pericarditis. Constrictive pericarditis often has pericardial thickening measuring greater than 4 mm. Potential causes of restrictive cardiomyopathy include sarcoidosis and amyloidosis; restrictive cardiomyopathy can also be idiopathic.