Procedure 75 Scaphotrapeziotrapezoid Arthrodesis and Lunate Excision with Replacement by Palmaris Longus Tendon
Indications
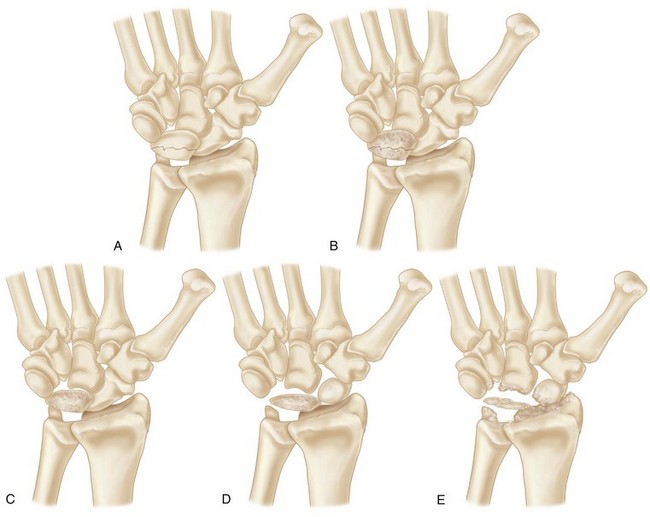
 Advanced avascular necrosis of the lunate from late stage IIIA to early stage IV according to the Lichtman preoperative 5-stage classification.
Advanced avascular necrosis of the lunate from late stage IIIA to early stage IV according to the Lichtman preoperative 5-stage classification.
 This procedure is mainly indicated for stage IIIB Kienböck disease, which is associated with carpal collapse with a fixed palmar scaphoid flexion.
This procedure is mainly indicated for stage IIIB Kienböck disease, which is associated with carpal collapse with a fixed palmar scaphoid flexion.
 A radiograph showing generalized arthrosis is not suitable for scaphotrapeziotrapezoid (STT) arthrodesis and lunate excision with replacement by the palmaris longus tendon.
A radiograph showing generalized arthrosis is not suitable for scaphotrapeziotrapezoid (STT) arthrodesis and lunate excision with replacement by the palmaris longus tendon.
 This procedure is contraindicated in patients with preoperative advanced osteoarthrosis between the radius and scaphoid because of the risk for further progression of osteoarthrosis at the radioscaphoid joint.
This procedure is contraindicated in patients with preoperative advanced osteoarthrosis between the radius and scaphoid because of the risk for further progression of osteoarthrosis at the radioscaphoid joint.
Examination/Imaging
Clinical Examination
 A complete examination of the involved and contralateral extremity is indicated, especially if the patient has a history of autoimmune disease or infection.
A complete examination of the involved and contralateral extremity is indicated, especially if the patient has a history of autoimmune disease or infection.
 Documentation of baseline pinch and grip strength is helpful.
Documentation of baseline pinch and grip strength is helpful.
 Attention to soft tissue swelling must be given because some patients have associated capsular inflammation, thickening, and synovitis.
Attention to soft tissue swelling must be given because some patients have associated capsular inflammation, thickening, and synovitis.
 Pain can be elicited in all directions of motion, and frequently there is a notable decrease in the arc of motion, particularly in extension.
Pain can be elicited in all directions of motion, and frequently there is a notable decrease in the arc of motion, particularly in extension.
 Degree of pain, range of motion of the wrist, and grip strength of both wrists should be meticulously measured preoperatively to evaluate postoperative results.
Degree of pain, range of motion of the wrist, and grip strength of both wrists should be meticulously measured preoperatively to evaluate postoperative results.
Imaging
Plain Radiographs
 Staging: Lichtman modification of Stahl staging
Staging: Lichtman modification of Stahl staging
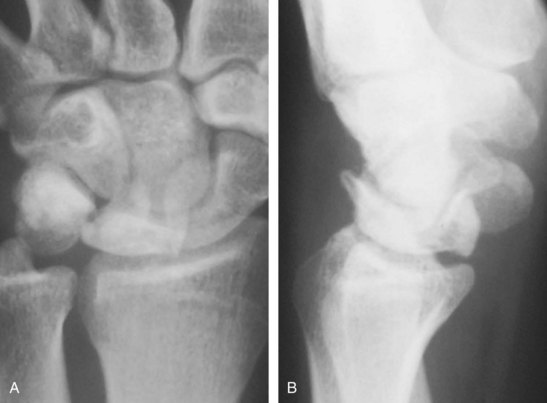
 Posteroanterior (PA) and lateral radiographs with the wrist in neutral rotation and neutral flexion-extension (Fig. 75-2).
Posteroanterior (PA) and lateral radiographs with the wrist in neutral rotation and neutral flexion-extension (Fig. 75-2).
 Ulnar variance radiographic views with the wrist in full pronation and full supination. The carpal height ratio is measured from PA view with the wrist in neutral position. The Stahl index is also measured from lateral view.
Ulnar variance radiographic views with the wrist in full pronation and full supination. The carpal height ratio is measured from PA view with the wrist in neutral position. The Stahl index is also measured from lateral view.
 Lunate sclerosis, carpal instability patterns, and fragmentation are seen.
Lunate sclerosis, carpal instability patterns, and fragmentation are seen.
 Shortened scaphoid in the long axis and cortical ring sign of the scaphoid are seen in stage IIIB, which indicates scaphoid in flexed position.
Shortened scaphoid in the long axis and cortical ring sign of the scaphoid are seen in stage IIIB, which indicates scaphoid in flexed position.
 Evaluation of relationship among scaphoid, trapezium, and trapezoid.
Evaluation of relationship among scaphoid, trapezium, and trapezoid.
Computed Tomography
 Computed tomography (CT) is needed to evaluate precisely the bony architecture of the lunate and the remainder of the carpus to determine which procedure is indicated and to determine whether arthritic changes of the midcarpal and radiocarpal joints are present.
Computed tomography (CT) is needed to evaluate precisely the bony architecture of the lunate and the remainder of the carpus to determine which procedure is indicated and to determine whether arthritic changes of the midcarpal and radiocarpal joints are present.
 A CT scan is useful for evaluation of fragmentation or fracture patterns and associated collapse.
A CT scan is useful for evaluation of fragmentation or fracture patterns and associated collapse.
Magnetic Resonance Imaging
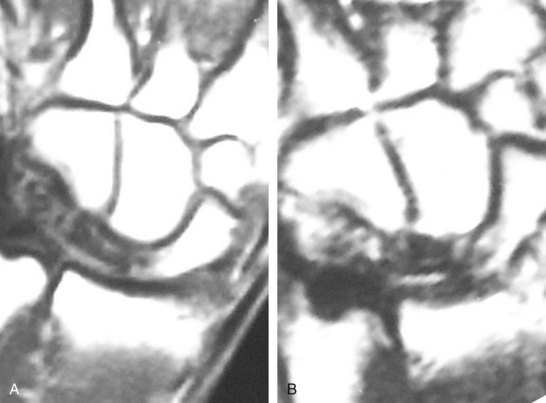
 MRI will show decreased uptake in both T1- and T2-weighted images. Gadolinium contrast has improved diagnosis and evaluation of lunate vascularity (Fig. 75-3).
MRI will show decreased uptake in both T1- and T2-weighted images. Gadolinium contrast has improved diagnosis and evaluation of lunate vascularity (Fig. 75-3).
 It is important to differentiate between ulnar impaction of the lunate and true Kienböck disease.
It is important to differentiate between ulnar impaction of the lunate and true Kienböck disease.
 Stage 0 has been proposed when lunate edema is visible on MRI only. MRI can show the degree of devascularization or revascularization.
Stage 0 has been proposed when lunate edema is visible on MRI only. MRI can show the degree of devascularization or revascularization.
Controversies
Treatment Options
Radial shortening osteotomy and capitate shortening may also unload the lunate.
Instead of STT arthrodesis, some surgeons prefer to perform scaphocapitate (SC) arthrodesis.
Revascularization with a vascularized bone graft has been advocated in early stages, and successes have been reported in late stages as well.
Core decompression of the lunate has also been described.
Salvage procedures for painful wrists that have not responded to the STT arthrodesis include total wrist arthrodesis, partial or total wrist arthroplasty, or proximal row carpectomy.
Exposures
Procedure
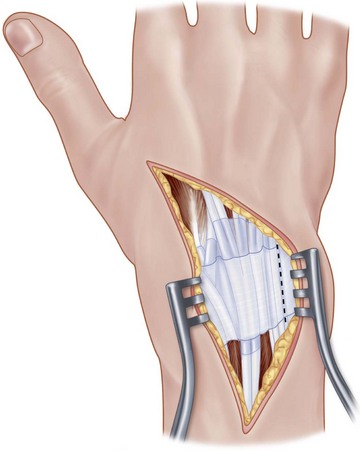
 Superficial branches of the radial nerve are retracted during the procedure.
Superficial branches of the radial nerve are retracted during the procedure.
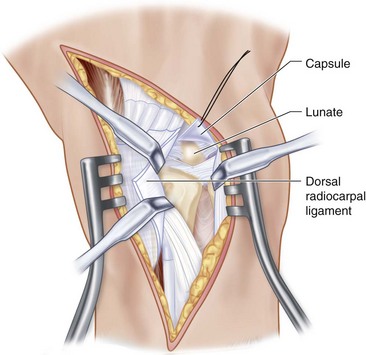
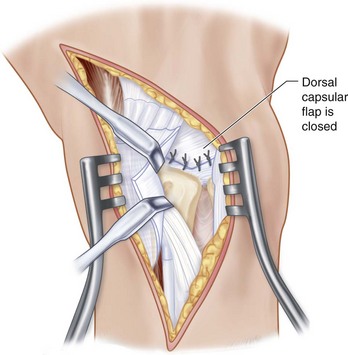
 Through the proximal half of the incision, the extensor retinaculum is exposed. The capsular flap is incised between the third and fourth dorsal compartments to expose the lunate (Fig. 75-5).
Through the proximal half of the incision, the extensor retinaculum is exposed. The capsular flap is incised between the third and fourth dorsal compartments to expose the lunate (Fig. 75-5).
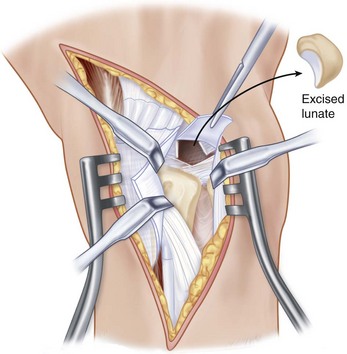
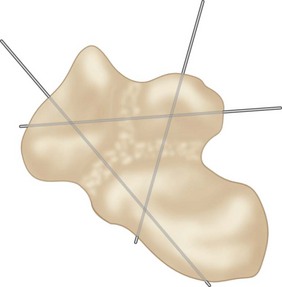
 The lunate is removed piecemeal or entirely in one piece, with great care to avoid injury to the palmar wrist ligaments (Fig. 75-6).
The lunate is removed piecemeal or entirely in one piece, with great care to avoid injury to the palmar wrist ligaments (Fig. 75-6).
 An ipsilateral palmaris longus tendon is removed with a tendon stripper.
An ipsilateral palmaris longus tendon is removed with a tendon stripper.
 The tendon strip is rolled into a “rugby ball,” sutured to itself, and inserted into the defect of the excised lunate.
The tendon strip is rolled into a “rugby ball,” sutured to itself, and inserted into the defect of the excised lunate.
Instrumentation/Implantation
Various types of small osteotomes and chisels are useful to remove the cortex of scaphoid, trapezium, and trapezoid. A low-powered surgical bur is also convenient to expose cancellous bones between the scaphoid, trapezium, and trapezoid.
A hand-held drill is necessary to insert K-wires between the scaphoid, trapezium, and trapezoid.
Step 1 Pitfalls
The lunate is ideally removed as one bone, although this is not easy. Therefore, we prefer to remove the lunate piecemeal.
The palmar wrist capsule and ligaments are protected during removal of the lunate.
If the palmaris longus tendon is absent, the plantaris tendon or a half slip of the extensor carpi radialis longus tendon is harvested.
Step 2
 Through the distal half of the incision, the wrist and thumb extensors are exposed.
Through the distal half of the incision, the wrist and thumb extensors are exposed.
 Wrist and thumb extensors are retracted.
Wrist and thumb extensors are retracted.
 The articular surfaces between the scaphoid, trapezium, and trapezoid are exposed.
The articular surfaces between the scaphoid, trapezium, and trapezoid are exposed.
 The articular cartilage and subchondral bone of the three joints are removed to expose the cancellous bone (Fig. 75-8).
The articular cartilage and subchondral bone of the three joints are removed to expose the cancellous bone (Fig. 75-8).
 Cancellous bone from the iliac crest is grafted into the joint spaces to prevent shortening of the carpus (Fig. 75-9).
Cancellous bone from the iliac crest is grafted into the joint spaces to prevent shortening of the carpus (Fig. 75-9).
Step 3
 The proximal pole of the scaphoid is depressed until it is under the dorsal surface of the lunate fossa on the radius to reduce the flexed posture of the scaphoid. This distal pole is pulled dorsally, if necessary, and K-wires are then driven percutaneously through the scaphoid into the capitate to maintain reduction (see Fig. 75-9).
The proximal pole of the scaphoid is depressed until it is under the dorsal surface of the lunate fossa on the radius to reduce the flexed posture of the scaphoid. This distal pole is pulled dorsally, if necessary, and K-wires are then driven percutaneously through the scaphoid into the capitate to maintain reduction (see Fig. 75-9).
 The position of the scaphoid is confirmed by intraoperative imaging (Fig. 75-10).
The position of the scaphoid is confirmed by intraoperative imaging (Fig. 75-10).
 Figure 75-10A shows a preoperative radiograph of Kienböck disease classified by stage IIIB.
Figure 75-10A shows a preoperative radiograph of Kienböck disease classified by stage IIIB.
 Figure 75-10B shows a radiograph of the excision of the lunate.
Figure 75-10B shows a radiograph of the excision of the lunate.
 Figure 75-10C shows a radiograph of an STT arthrodesis after the removal of the lunate.
Figure 75-10C shows a radiograph of an STT arthrodesis after the removal of the lunate.
 Figure 75-10D shows a radiograph 3 years after excision of the lunate and STT arthrodesis.
Figure 75-10D shows a radiograph 3 years after excision of the lunate and STT arthrodesis.
Postoperative Care and Expected Outcomes
 The patient is placed in a well-padded short-arm thumb spica splint with the thumb in maximal opposed position and the wrist and forearm in neutral positions.
The patient is placed in a well-padded short-arm thumb spica splint with the thumb in maximal opposed position and the wrist and forearm in neutral positions.
 The patient is given instructions on routine splint care, told to maintain a non–weight-bearing status for the upper extremity, and encouraged to work on gentle finger range-of-motion exercises.
The patient is given instructions on routine splint care, told to maintain a non–weight-bearing status for the upper extremity, and encouraged to work on gentle finger range-of-motion exercises.
 The postoperative splint is removed about 2 weeks after surgery. The wound is examined, and sutures are moved. The patient is then placed in a short-arm thumb spica cast. Finger range of motion is assessed to determine whether stiffness of the interphalangeal or metacarpophalangeal joints has developed.
The postoperative splint is removed about 2 weeks after surgery. The wound is examined, and sutures are moved. The patient is then placed in a short-arm thumb spica cast. Finger range of motion is assessed to determine whether stiffness of the interphalangeal or metacarpophalangeal joints has developed.
 Six weeks after surgery, the patient’s cast is removed, and unions among three bones are evaluated by plain radiographs or CT. A short-arm thumb spica cast is applied until arthrodesis is obtained.
Six weeks after surgery, the patient’s cast is removed, and unions among three bones are evaluated by plain radiographs or CT. A short-arm thumb spica cast is applied until arthrodesis is obtained.
 The patient is re-evaluated 10 or 12 weeks after surgery. Union should be achieved at this point. If so, the patient is not placed in a cast but rather is given a removable splint for comfort and to protect the surgical site. Wrist range of motion is emphasized.
The patient is re-evaluated 10 or 12 weeks after surgery. Union should be achieved at this point. If so, the patient is not placed in a cast but rather is given a removable splint for comfort and to protect the surgical site. Wrist range of motion is emphasized.
Minami A, Kato H, Suenaga N, et al. Scaphotrapezio-trapezoid fusion: long-term follow-up study. J Orthop Sci.. 2003;8:319-322.
Minami A, Kimura T, Suzuki K. Long-term results of Kienböck’s disease treated by triscaphe arthrodesis and excisional arthroplasty with a coiled palmaris longus tendon. J Hand Surg [Am]. 1994;19:219-228.
Watson HK, Ryu J, DiBella A. An approach to Kienböck’s disease: Triscaphe arthrodesis. J Hand Surg [Am]. 1985;10:17-87.