Procedure 74 Lunotriquetral Ligament Reconstruction Using a Slip of the Extensor Carpi Ulnaris Tendon
![]() See Video 55: Lunotriquetral Ligament Reconstruction Using the Extensor Carpi Ulnaris Tendon
See Video 55: Lunotriquetral Ligament Reconstruction Using the Extensor Carpi Ulnaris Tendon
Examination/Imaging
Clinical Examination
 Patients with LT instability present with ulnar-sided wrist pain. Other causes of ulnar-sided wrist pain include ulnar impaction syndrome, extensor carpi ulnaris (ECU) subluxation, distal radioulnar joint (DRUJ) instability, triangular fibrocartilage complex (TFCC) injuries, pisotriquetral arthritis, and hook of hamate fractures.
Patients with LT instability present with ulnar-sided wrist pain. Other causes of ulnar-sided wrist pain include ulnar impaction syndrome, extensor carpi ulnaris (ECU) subluxation, distal radioulnar joint (DRUJ) instability, triangular fibrocartilage complex (TFCC) injuries, pisotriquetral arthritis, and hook of hamate fractures.
 The following clinical tests can help differentiate LT instability from other causes of ulnar-sided wrist pain.
The following clinical tests can help differentiate LT instability from other causes of ulnar-sided wrist pain.
Imaging
 A posteroanterior radiograph may show a step-off between the lunate and triquetrum and the disruption of the normal convex arc of the proximal carpal row (Gilula line). Unlike the scapholunate dissociation, a gap in the LT interval is rarely seen in patients with LT instability.
A posteroanterior radiograph may show a step-off between the lunate and triquetrum and the disruption of the normal convex arc of the proximal carpal row (Gilula line). Unlike the scapholunate dissociation, a gap in the LT interval is rarely seen in patients with LT instability.
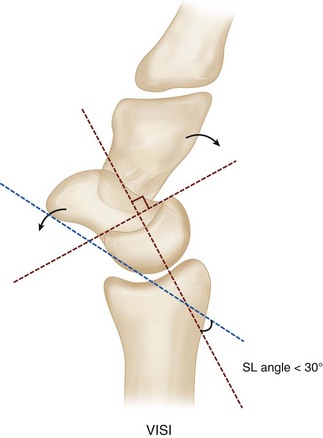
 Plain radiographs may show a volar intercalated segment instability (VISI) deformity, marked by volar tilting of the lunate (Fig. 74-3).
Plain radiographs may show a volar intercalated segment instability (VISI) deformity, marked by volar tilting of the lunate (Fig. 74-3).
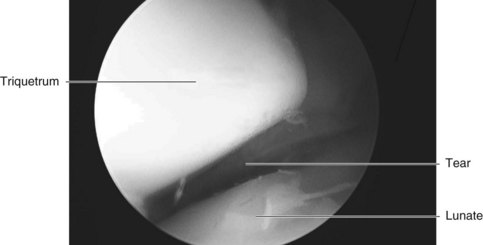
 Wrist arthroscopy is useful to diagnose an LT ligament tear when plain radiographs are normal (Fig. 74-4). The LT interosseous space is tightly closed in normal subjects, whereas in LT dissociations, the space can be opened with the probe, and a gap can be seen between the involved carpals from the midcarpal portal.
Wrist arthroscopy is useful to diagnose an LT ligament tear when plain radiographs are normal (Fig. 74-4). The LT interosseous space is tightly closed in normal subjects, whereas in LT dissociations, the space can be opened with the probe, and a gap can be seen between the involved carpals from the midcarpal portal.
Surgical Anatomy
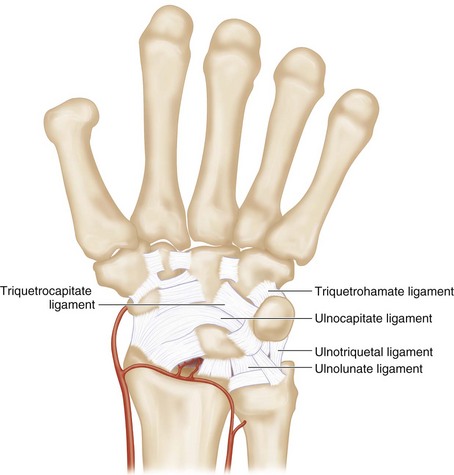
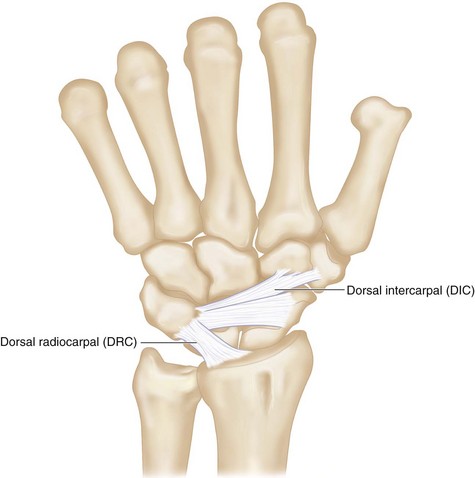
 The LT ligament is C shaped, spanning the (1) dorsal, (2) proximal, and (3) palmar edges of the joint surfaces. The palmar region is the thickest and strongest. It is the primary stabilizer of the LT joint. Additional supports of the LT joint include the ulnocarpal (ulnolunate, ulnocapitate, and ulnotriquetral ligaments), midcarpal (triquetrohamate and triquetrocapitate ligaments), and dorsal carpal (dorsal intercarpal and radiotriquetral) ligaments (Figs. 74-5 and 74-6).
The LT ligament is C shaped, spanning the (1) dorsal, (2) proximal, and (3) palmar edges of the joint surfaces. The palmar region is the thickest and strongest. It is the primary stabilizer of the LT joint. Additional supports of the LT joint include the ulnocarpal (ulnolunate, ulnocapitate, and ulnotriquetral ligaments), midcarpal (triquetrohamate and triquetrocapitate ligaments), and dorsal carpal (dorsal intercarpal and radiotriquetral) ligaments (Figs. 74-5 and 74-6).
 The key injury in LT dissociation is a failure of the stronger palmar portion of the LT ligament. The lunate, then connected only to the scaphoid, follows the inherent tendency of the scaphoid to flex. However, a complete tear of only the LT ligament will not result in carpal collapse (VISI) because the secondary stabilizers maintain the lunate and triquetrum in position.
The key injury in LT dissociation is a failure of the stronger palmar portion of the LT ligament. The lunate, then connected only to the scaphoid, follows the inherent tendency of the scaphoid to flex. However, a complete tear of only the LT ligament will not result in carpal collapse (VISI) because the secondary stabilizers maintain the lunate and triquetrum in position.
Exposures
Dorsal
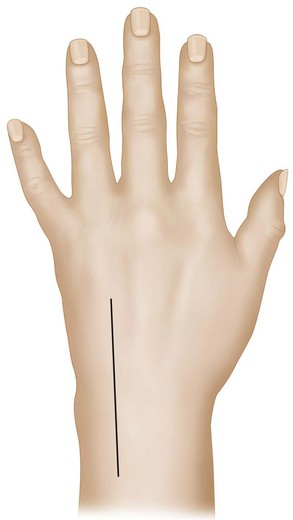
 A 6-cm longitudinal incision centered over the radiocarpal joint is made over the dorsal wrist between the fourth and fifth compartments (Fig. 74-7).
A 6-cm longitudinal incision centered over the radiocarpal joint is made over the dorsal wrist between the fourth and fifth compartments (Fig. 74-7).
 The wrist capsule is opened through a longitudinal incision. A longitudinal incision is also quite suitable for later imbrication of the ulnar wrist capsule over the LT ligament repair.
The wrist capsule is opened through a longitudinal incision. A longitudinal incision is also quite suitable for later imbrication of the ulnar wrist capsule over the LT ligament repair.
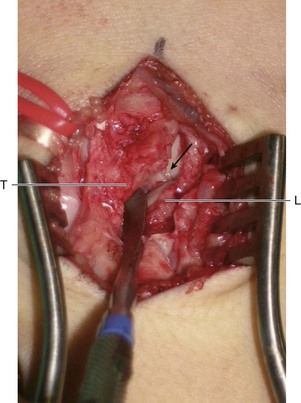
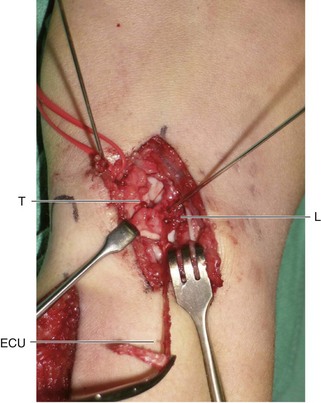
 Figure 74-8 shows a Freer elevator in the LT interval demonstrating a complete rupture of the LT ligament.
Figure 74-8 shows a Freer elevator in the LT interval demonstrating a complete rupture of the LT ligament.
 The ECU tendon is identified in the proximal portion of this incision.
The ECU tendon is identified in the proximal portion of this incision.
Pitfalls
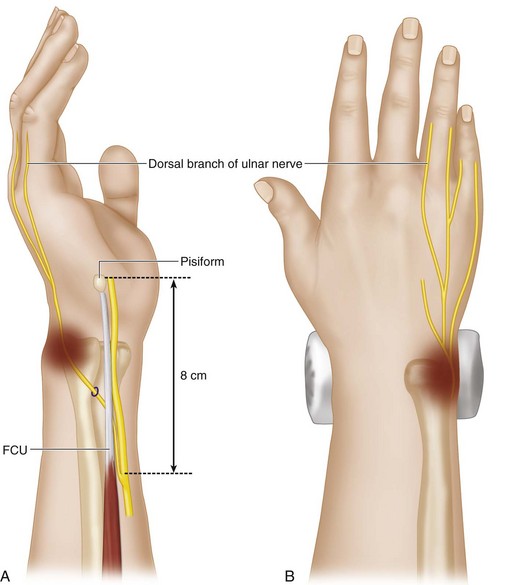
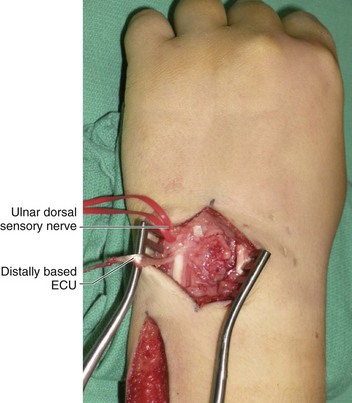
Branches of the ulnar dorsal sensory nerve should be protected. This nerve arises from the ulnar aspect of the ulnar nerve about 8 cm proximal to the pisiform. It then passes dorsal to the flexor carpi ulnaris (FCU) and pierces the deep fascia about 5 cm from the pisiform. It reaches the dorsum of the hand after coursing in close relation to the ulnar styloid process (Fig. 74-9).
Procedure
Step 2: Harvest a Strip of Distally Based ECU
Step 3: Reduction of Lunate and Triquetrum
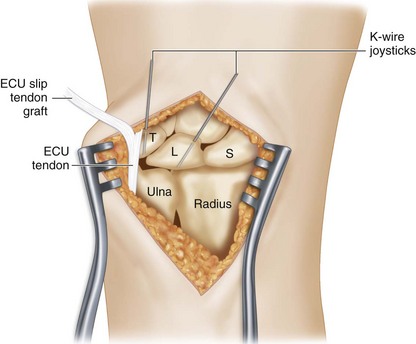
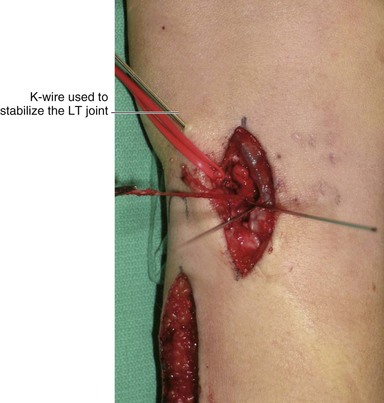
 Two 0.045-inch Kirschner wires (K-wires) are inserted into the lunate and the triquetrum to act as joysticks to reduce the carpal bones (Fig. 74-11).
Two 0.045-inch Kirschner wires (K-wires) are inserted into the lunate and the triquetrum to act as joysticks to reduce the carpal bones (Fig. 74-11).
Step 3 Pearls
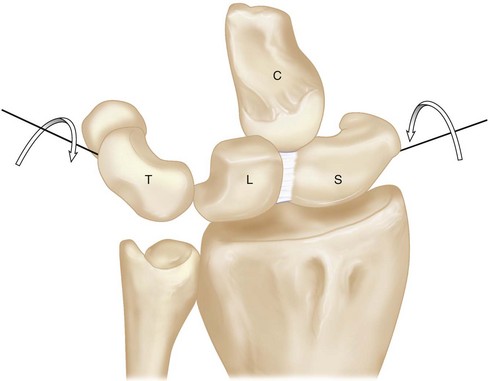
The joystick K-wires are used to correct the VISI deformity. The lunate is flexed and the triquetrum extended (Fig. 74-12). The lunate K-wire should be inserted in an oblique distal to proximal direction, whereas the triquetral K-wire should be inserted in an oblique proximal to distal direction. The VISI deformity can be corrected by making both K-wires perpendicular to the axis of the forearm.
Step 4: Create a Bone Tunnel within Triquetrum and Lunate
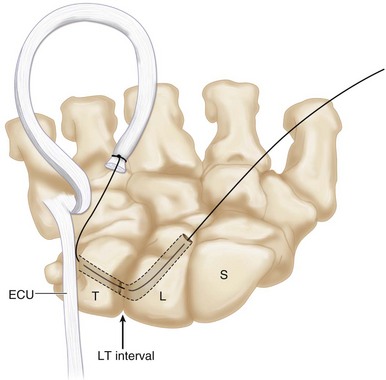
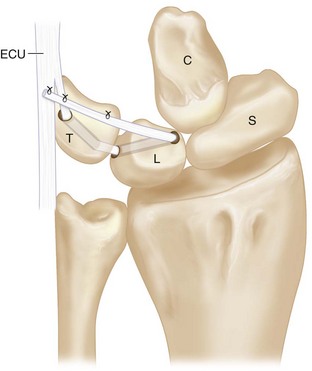
 A K-wire is passed from the distal, dorsal, and ulnar aspect of the triquetrum to exit at the proximal, palmar, and radial corner of triquetrum. Once acceptable placement of the K-wire is confirmed, a 2.5-mm cannulated drill is inserted over the K-wire to create a bone tunnel within the triquetrum.
A K-wire is passed from the distal, dorsal, and ulnar aspect of the triquetrum to exit at the proximal, palmar, and radial corner of triquetrum. Once acceptable placement of the K-wire is confirmed, a 2.5-mm cannulated drill is inserted over the K-wire to create a bone tunnel within the triquetrum.
 A similar bone tunnel is created from the distal, dorsal, and radial corner of the lunate to exit at the proximal, palmar, and ulnar aspect of the lunate (Fig. 74-13). A microcurette is used to remove the cartilage remnants at the exit sites of the drill holes.
A similar bone tunnel is created from the distal, dorsal, and radial corner of the lunate to exit at the proximal, palmar, and ulnar aspect of the lunate (Fig. 74-13). A microcurette is used to remove the cartilage remnants at the exit sites of the drill holes.
Step 5: Pass the ECU through the Lunate and Triquetrum Tunnel
Step 6: Secure the ECU Graft to Itself and over the Remnant of the LT Ligament
 The VISI deformity is corrected using the previously placed joystick wires, and the corrected position is maintained by a 0.045-inch K-wire passed between the lunate and triquetrum (Fig. 74-15).
The VISI deformity is corrected using the previously placed joystick wires, and the corrected position is maintained by a 0.045-inch K-wire passed between the lunate and triquetrum (Fig. 74-15).
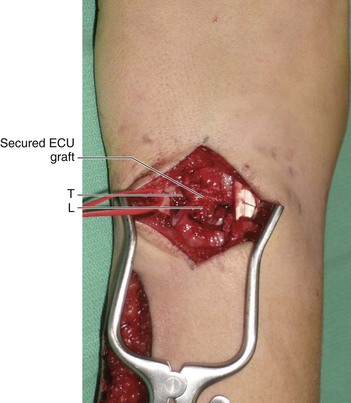
 The end of the tendon graft is sutured back to itself and to any remnants of the LT ligament over the triquetrum using 3-0 Ethibond sutures (Fig. 74-16). This will tighten the triquetrum against the lunate (Fig. 74-17).
The end of the tendon graft is sutured back to itself and to any remnants of the LT ligament over the triquetrum using 3-0 Ethibond sutures (Fig. 74-16). This will tighten the triquetrum against the lunate (Fig. 74-17).
Step 7: Closure
 The extensor retinaculum over the fourth and fifth compartments is closed using 3-0 Ethibond sutures.
The extensor retinaculum over the fourth and fifth compartments is closed using 3-0 Ethibond sutures.
 The two joystick K-wires are removed, and the K-wire stabilizing the lunate and triquetrum is cut under the skin.
The two joystick K-wires are removed, and the K-wire stabilizing the lunate and triquetrum is cut under the skin.
 The wrist capsule is closed tightly. The tourniquet is deflated, and all bleeding areas are cauterized.
The wrist capsule is closed tightly. The tourniquet is deflated, and all bleeding areas are cauterized.
Postoperative Care and Expected Outcomes
 The patient is kept in a wrist volar splint for 8 weeks.
The patient is kept in a wrist volar splint for 8 weeks.
 After 8 weeks, the K-wires are removed, and the patient starts gentle range-of-motion exercises (Figs. 74-18 and 74-19).
After 8 weeks, the K-wires are removed, and the patient starts gentle range-of-motion exercises (Figs. 74-18 and 74-19).
 Pain is generally significantly improved in about 90% of patients after this procedure. The postoperative grip strength and range of wrist motion are usually increased, and the patient’s satisfaction at long-term follow-up is also high (about 90%).
Pain is generally significantly improved in about 90% of patients after this procedure. The postoperative grip strength and range of wrist motion are usually increased, and the patient’s satisfaction at long-term follow-up is also high (about 90%).