Procedure 73 Scapholunate Ligament Reconstruction Using a Flexor Carpi Radialis Tendon Graft
![]() See Video 54: Scapholunate Ligament Reconstruction Using the Flexor Carpi Radialis Tendon
See Video 54: Scapholunate Ligament Reconstruction Using the Flexor Carpi Radialis Tendon
Examination/Imaging
Clinical Examination
 Patients complain of radial-sided wrist pain especially with loading activities, weakness of grip, and swelling.
Patients complain of radial-sided wrist pain especially with loading activities, weakness of grip, and swelling.
 Tenderness is found in the radial snuffbox or over the SL interval just distal to the Lister tubercle.
Tenderness is found in the radial snuffbox or over the SL interval just distal to the Lister tubercle.
 Discomfort is reported at extremes of wrist extension and radial deviation.
Discomfort is reported at extremes of wrist extension and radial deviation.
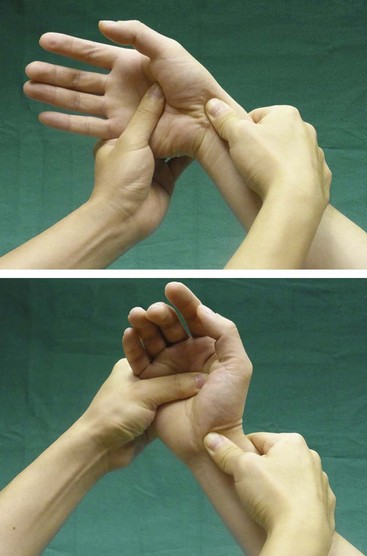
 The scaphoid shift test (Watson test) may be positive in SL dissociation. The examiner places four fingers behind the radius. The thumb is placed on the scaphoid tuberosity, and the other hand is used to move the wrist passively from ulnar to radial deviation. In ulnar deviation, the scaphoid is extended, whereas in radial deviation, the scaphoid is flexed. Pressure on the tuberosity while the wrist is moved from ulnar deviation to radial deviation prevents the scaphoid from flexing. In such circumstances, if the SL ligaments are completely insufficient or torn, the proximal pole subluxates dorsally out of the scaphoid fossa, inducing pain on the dorsoradial aspect of the wrist. When pressure is released, a typical clunk may occur, indicating an abrupt self-reduction of the scaphoid back into its normal position (Fig. 73-1). This test is painful for the patient and should be done selectively, when obvious SL separation is not seen on radiograph.
The scaphoid shift test (Watson test) may be positive in SL dissociation. The examiner places four fingers behind the radius. The thumb is placed on the scaphoid tuberosity, and the other hand is used to move the wrist passively from ulnar to radial deviation. In ulnar deviation, the scaphoid is extended, whereas in radial deviation, the scaphoid is flexed. Pressure on the tuberosity while the wrist is moved from ulnar deviation to radial deviation prevents the scaphoid from flexing. In such circumstances, if the SL ligaments are completely insufficient or torn, the proximal pole subluxates dorsally out of the scaphoid fossa, inducing pain on the dorsoradial aspect of the wrist. When pressure is released, a typical clunk may occur, indicating an abrupt self-reduction of the scaphoid back into its normal position (Fig. 73-1). This test is painful for the patient and should be done selectively, when obvious SL separation is not seen on radiograph.
 A positive SL ballottement test may be elicited. The examiner holds the patient’s scaphoid between the thumb (placed over the scaphoid tuberosity on the palmar side) and index finger (placed over the proximal pole of the scaphoid on the dorsum) of one hand, while holding the lunate between the thumb and index of the other hand. The examiner then attempts to move the scaphoid and lunate in opposite directions. If the test induces pain, this test is positive, and the patient may have SL instability (Fig. 73-2).
A positive SL ballottement test may be elicited. The examiner holds the patient’s scaphoid between the thumb (placed over the scaphoid tuberosity on the palmar side) and index finger (placed over the proximal pole of the scaphoid on the dorsum) of one hand, while holding the lunate between the thumb and index of the other hand. The examiner then attempts to move the scaphoid and lunate in opposite directions. If the test induces pain, this test is positive, and the patient may have SL instability (Fig. 73-2).
Imaging
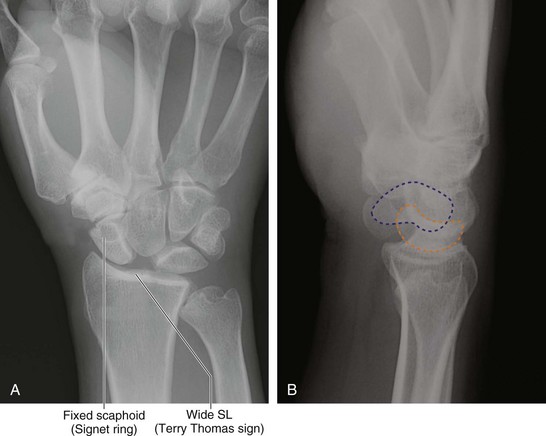
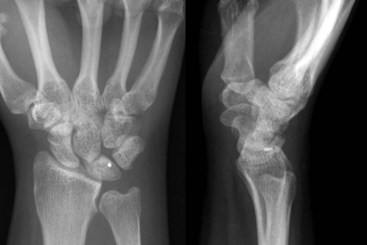
 A gap greater than 3 mm between the scaphoid and lunate on a standard posteroanterior (PA) view indicates SL dissociation. The presence of a flexed scaphoid on a PA view (signet ring sign) (Fig. 73-3A) and an extended lunate on a lateral view is suggestive of SL dissociation with associated carpal malalignment (DISI) (Fig. 73-3B).
A gap greater than 3 mm between the scaphoid and lunate on a standard posteroanterior (PA) view indicates SL dissociation. The presence of a flexed scaphoid on a PA view (signet ring sign) (Fig. 73-3A) and an extended lunate on a lateral view is suggestive of SL dissociation with associated carpal malalignment (DISI) (Fig. 73-3B).
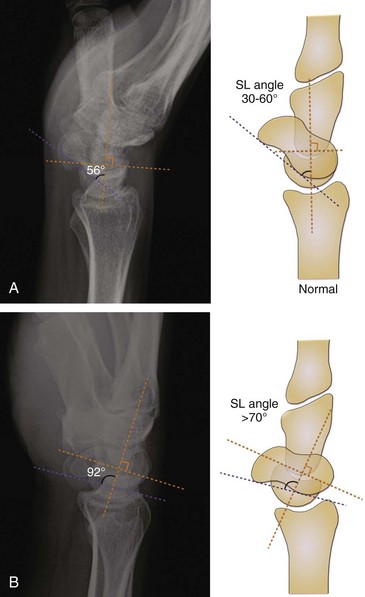
 The normal SL angle ranges from 30 to 60 degrees (Fig. 73-4A). An SL angle greater than 70° indicates DISI (Fig. 73-4B). The SL angle is formed by intersection of the scaphoid axis (a line joining the most palmar point on the distal pole with the most palmar point on the proximal pole of the scaphoid) and lunate axis (a line drawn perpendicular to the line joining the most distal palmar and dorsal points of the lunate).
The normal SL angle ranges from 30 to 60 degrees (Fig. 73-4A). An SL angle greater than 70° indicates DISI (Fig. 73-4B). The SL angle is formed by intersection of the scaphoid axis (a line joining the most palmar point on the distal pole with the most palmar point on the proximal pole of the scaphoid) and lunate axis (a line drawn perpendicular to the line joining the most distal palmar and dorsal points of the lunate).
 The presence of osteoarthritic changes involving the radiocarpal or midcarpal joints is a contraindication for ligament reconstruction. Figure 73-5 shows radiographs of a patient with bilateral SL dissociation. He has osteoarthritic changes involving the radial styloid and radioscaphoid joint on the left side.
The presence of osteoarthritic changes involving the radiocarpal or midcarpal joints is a contraindication for ligament reconstruction. Figure 73-5 shows radiographs of a patient with bilateral SL dissociation. He has osteoarthritic changes involving the radial styloid and radioscaphoid joint on the left side.
 Magnetic resonance imaging is often valuable to define other injuries and disorders that may affect the surgical outcome.
Magnetic resonance imaging is often valuable to define other injuries and disorders that may affect the surgical outcome.
 Arthroscopy can be used to determine the extent of SL ligament disruption and the presence of arthritis.
Arthroscopy can be used to determine the extent of SL ligament disruption and the presence of arthritis.
Surgical Anatomy
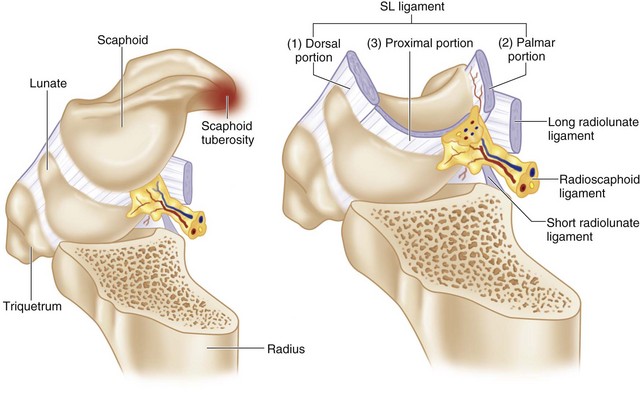
 The SL ligament is a C-shaped structure that connects the dorsal, proximal, and volar surfaces of the scaphoid and lunate. It has three portions: (1) the dorsal portion, which has the highest rupture strength and is responsible for rotational and translational restraint; (2) the proximal membranous portion; and (3) the volar portion (Fig. 73-6).
The SL ligament is a C-shaped structure that connects the dorsal, proximal, and volar surfaces of the scaphoid and lunate. It has three portions: (1) the dorsal portion, which has the highest rupture strength and is responsible for rotational and translational restraint; (2) the proximal membranous portion; and (3) the volar portion (Fig. 73-6).
Exposures
Dorsal
 An 8-cm longitudinal dorsal wrist incision centered over the Lister tubercle is made (Fig. 73-7).
An 8-cm longitudinal dorsal wrist incision centered over the Lister tubercle is made (Fig. 73-7).
 The extensor retinaculum over the third compartment is opened, and the extensor pollicis longus (EPL) is retracted radially to expose the dorsal wrist capsule.
The extensor retinaculum over the third compartment is opened, and the extensor pollicis longus (EPL) is retracted radially to expose the dorsal wrist capsule.
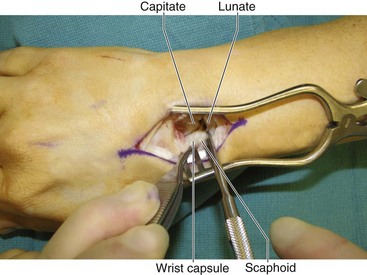
 The dorsal capsule is then opened through a longitudinal incision to visualize the SL interval (Fig. 73-8).
The dorsal capsule is then opened through a longitudinal incision to visualize the SL interval (Fig. 73-8).
Volar
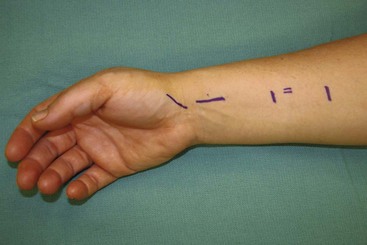
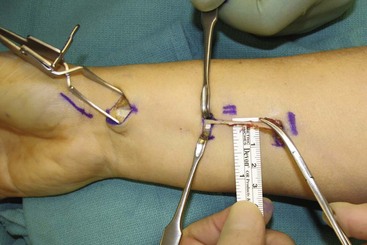
 Three 1-cm incisions along the course of flexor carpi radialis (FCR) are made. Another oblique incision is made over the scaphoid tuberosity (Fig. 73-9).
Three 1-cm incisions along the course of flexor carpi radialis (FCR) are made. Another oblique incision is made over the scaphoid tuberosity (Fig. 73-9).
Procedure
Step 2: Reduction of Scaphoid and Lunate
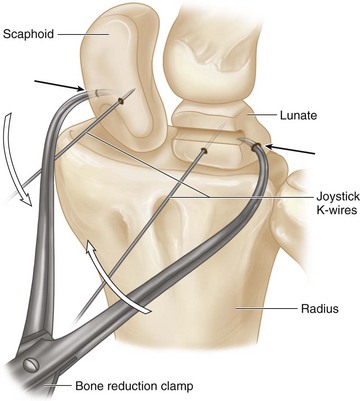
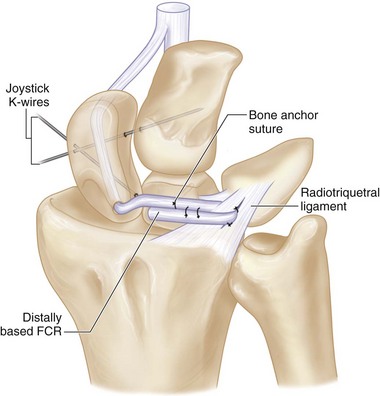
 Two 0.045-inch K-wires are placed dorsally into the scaphoid and lunate, respectively, to act as joysticks for reduction of these two bones (Fig. 73-11).
Two 0.045-inch K-wires are placed dorsally into the scaphoid and lunate, respectively, to act as joysticks for reduction of these two bones (Fig. 73-11).
Step 2 Pearls
Make certain that the joystick K-wires engage the bone well and do not pull out. Sometimes using threaded wires may ensure more secure purchase of the carpal bones. The wires must be drilled away from the anticipated tunnel that will contain the FCR tendon slip.
The scaphoid is flexed, and the lunate is extended. To correct the DISI, one needs to extend the scaphoid and flex the lunate. This is done using the joystick K-wires. Directing the scaphoid K-wire proximally and the lunate K-wire distally makes correction of the deformity easier.
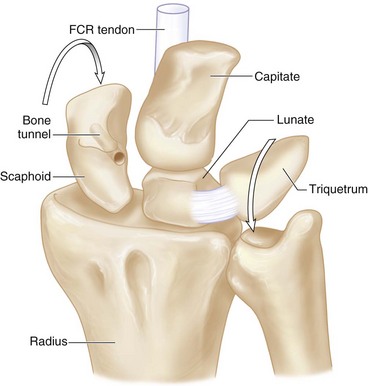
Step 3: Create a Bone Tunnel within Scaphoid
Step 4: Harvest a Strip of Distally Based FCR
Step 5: Pass the FCR through the Scaphoid Tunnel
 A grasping suture is placed at the cut end of the distally based FCR and passed through the scaphoid tunnel from volar to dorsal (Fig. 73-15).
A grasping suture is placed at the cut end of the distally based FCR and passed through the scaphoid tunnel from volar to dorsal (Fig. 73-15).
Step 6: Reduce SL Interval
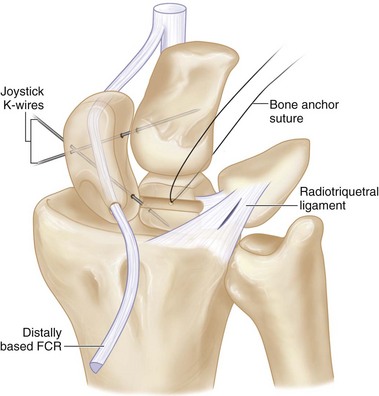
Step 7: Secure the FCR to the Lunate
 A shallow trough is made on the dorsum of the lunate using a bur.
A shallow trough is made on the dorsum of the lunate using a bur.
 The FCR graft is secured in the midportion of this trough using a 1.8-mm bone anchor suture (Mitek Mini QuickAnchor or similar) (Fig. 73-17).
The FCR graft is secured in the midportion of this trough using a 1.8-mm bone anchor suture (Mitek Mini QuickAnchor or similar) (Fig. 73-17).
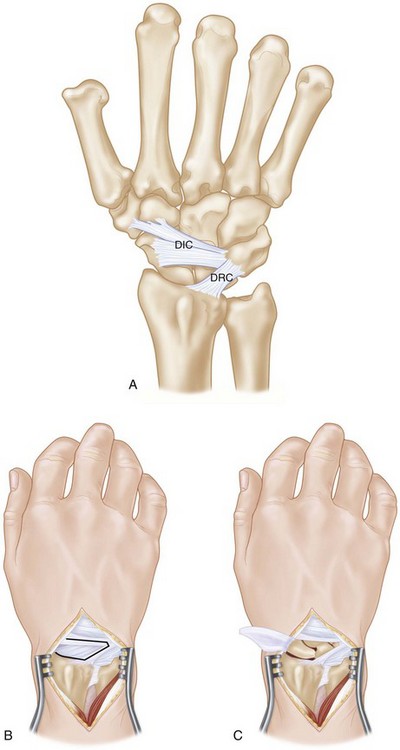
 The remaining portion of the FCR graft is passed through a slit in the distal portion of the dorsal radiotriquetral ligament and sutured back to itself over the lunate (Fig. 73-18).
The remaining portion of the FCR graft is passed through a slit in the distal portion of the dorsal radiotriquetral ligament and sutured back to itself over the lunate (Fig. 73-18).
Postoperative Care and Expected Outcomes
 Following surgery, the patient is placed in a volar wrist splint for 8 weeks.
Following surgery, the patient is placed in a volar wrist splint for 8 weeks.
 Ten days after the operation, the wound is examined and sutures are removed.
Ten days after the operation, the wound is examined and sutures are removed.
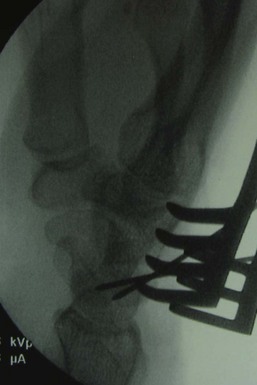
 The K-wires are removed 6 to 8 weeks after the surgery (Fig. 73-19). The K-wires are often cut under the skin to avoid pin tract infection, which is common when the K-wires are left outside the skin for more than 3 weeks. Pin tract infection into the wrist is a disastrous complication.
The K-wires are removed 6 to 8 weeks after the surgery (Fig. 73-19). The K-wires are often cut under the skin to avoid pin tract infection, which is common when the K-wires are left outside the skin for more than 3 weeks. Pin tract infection into the wrist is a disastrous complication.
 Eight weeks after the surgery, the patient is transitioned to a removable volar splint for an additional 4 weeks, and gentle active wrist range of motion commences.
Eight weeks after the surgery, the patient is transitioned to a removable volar splint for an additional 4 weeks, and gentle active wrist range of motion commences.
Chabas JF, Gay A, Valenti D, et al. Results of the modified Brunelli tenodesis for treatment of scapholunate instability: a retrospective study of 19 patients. J Hand Surg [Am]. 2008;33:1469-1477.
van den Abbeele KLS, Loh YC, Stanley JK, Trail IA. Early results of a modified Brunelli procedure for scapholunate instability. J Hand Surg [Br]. 1998;23:258-261.