Procedure 71 Open Reduction and Acute Repair of Perilunate Fracture-Dislocations
Examination/Imaging
Clinical Examination
 Severe wrist edema, tenderness, and ecchymosis may accompany the extreme pain that the patient is experiencing.
Severe wrist edema, tenderness, and ecchymosis may accompany the extreme pain that the patient is experiencing.
 Passive wrist motion is usually limited, painful, and disjointed (not smooth).
Passive wrist motion is usually limited, painful, and disjointed (not smooth).
 It is essential that a thorough neurovascular examination be performed to rule out acute carpal tunnel syndrome.
It is essential that a thorough neurovascular examination be performed to rule out acute carpal tunnel syndrome.
 If numbness, tingling, and two-point discrimination worsen after closed reduction, immediate carpal tunnel release should be performed (along with open reduction and fixation).
If numbness, tingling, and two-point discrimination worsen after closed reduction, immediate carpal tunnel release should be performed (along with open reduction and fixation).
 If the neurovascular examination is improving or normal and a good reduction is achieved, the surgery can be performed electively.
If the neurovascular examination is improving or normal and a good reduction is achieved, the surgery can be performed electively.
Imaging
 Lunate and perilunate dislocations are occasionally missed in the emergency room and dismissed as a severe wrist sprain despite having adequate imaging. Therefore, it is essential to obtain a thorough radiographic examination and scrutinize the images to prevent missing an acute injury.
Lunate and perilunate dislocations are occasionally missed in the emergency room and dismissed as a severe wrist sprain despite having adequate imaging. Therefore, it is essential to obtain a thorough radiographic examination and scrutinize the images to prevent missing an acute injury.
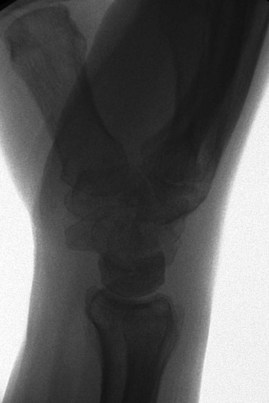
 A standard radiographic series of the wrist must be obtained to evaluate for dislocation. Assess for disruption of Gilula arc lines on the posteroanterior image. On a lateral radiograph, the radial shaft, lunate, capitate, and metacarpal shafts should be collinear (Fig. 71-1).
A standard radiographic series of the wrist must be obtained to evaluate for dislocation. Assess for disruption of Gilula arc lines on the posteroanterior image. On a lateral radiograph, the radial shaft, lunate, capitate, and metacarpal shafts should be collinear (Fig. 71-1).
 Radiographs should also be inspected to rule out associated radial styloid, scaphoid, capitate, or triquetral fractures (Fig. 71-2).
Radiographs should also be inspected to rule out associated radial styloid, scaphoid, capitate, or triquetral fractures (Fig. 71-2).
 Computed tomography can help better define any questionable fractures of the carpal bones.
Computed tomography can help better define any questionable fractures of the carpal bones.
Surgical Anatomy
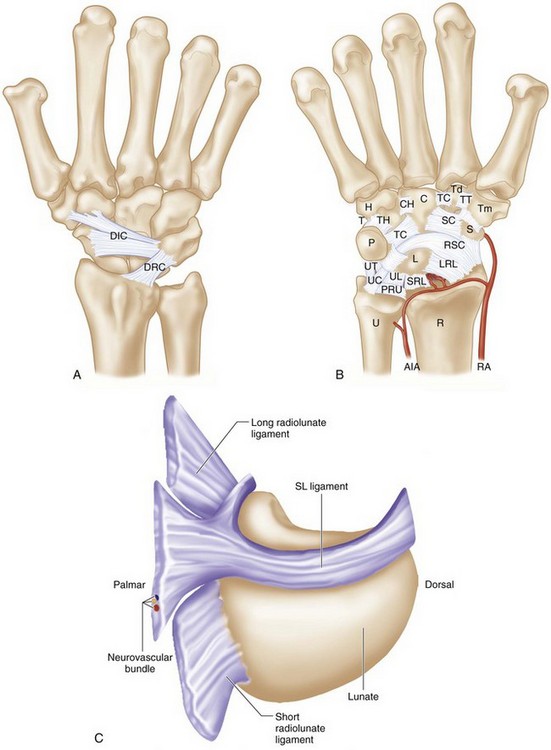
 The dorsal radiocarpal and intercarpal ligaments are frequently ruptured in these severe injuries (Fig 71-3A).
The dorsal radiocarpal and intercarpal ligaments are frequently ruptured in these severe injuries (Fig 71-3A).
 The strong volar ligaments have a characteristic transverse rent that is repaired through the volar approach (Fig. 71-3B).
The strong volar ligaments have a characteristic transverse rent that is repaired through the volar approach (Fig. 71-3B).
 The lunate dislocates through the space of Poirier, a relatively weak region of the volar capsule just below the arc of the radioscaphocapitate and ulnocapitate ligaments (see Fig. 71-3B).
The lunate dislocates through the space of Poirier, a relatively weak region of the volar capsule just below the arc of the radioscaphocapitate and ulnocapitate ligaments (see Fig. 71-3B).
 The dorsal portion of the scapholunate ligament is the thickest and strongest portion of the C-shaped ligament and should be repaired if adequate ligament tissue is present (Fig. 71-3C).
The dorsal portion of the scapholunate ligament is the thickest and strongest portion of the C-shaped ligament and should be repaired if adequate ligament tissue is present (Fig. 71-3C).
 The short radiolunate ligament serves as the pivot for the lunate when it dislocates into the carpal tunnel. It also provides blood supply to the dislocated lunate to prevent avascular necrosis.
The short radiolunate ligament serves as the pivot for the lunate when it dislocates into the carpal tunnel. It also provides blood supply to the dislocated lunate to prevent avascular necrosis.
Positioning
 The patient is positioned supine on the operating room table with the arm abducted on a radiolucent hand table.
The patient is positioned supine on the operating room table with the arm abducted on a radiolucent hand table.
 A minifluoroscope is positioned vertically at the end of the hand table with the image intensifier under the table.
A minifluoroscope is positioned vertically at the end of the hand table with the image intensifier under the table.
 Five to 10 pounds of longitudinal traction using finger traps may be helpful to obtain and maintain lunate reduction and proper position of the carpal bones.
Five to 10 pounds of longitudinal traction using finger traps may be helpful to obtain and maintain lunate reduction and proper position of the carpal bones.
Exposures
 A 7- to 8-cm longitudinal dorsal incision centered over the wrist is made, with exposure of the carpus through the third dorsal compartment (extensor pollicis longus [EPL] sheath).
A 7- to 8-cm longitudinal dorsal incision centered over the wrist is made, with exposure of the carpus through the third dorsal compartment (extensor pollicis longus [EPL] sheath).
 An extended carpal tunnel release incision is also made at the wrist. This extends from the Kaplan cardinal line distally to 3 to 4 cm proximal to the distal wrist flexion crease (Fig. 71-4).
An extended carpal tunnel release incision is also made at the wrist. This extends from the Kaplan cardinal line distally to 3 to 4 cm proximal to the distal wrist flexion crease (Fig. 71-4).
Procedure
Step 1: Volar Approach
 After the extended carpal tunnel incision, dissection is carried down through the transverse carpal ligament and distal antebrachial fascia to completely decompress the median nerve (Fig. 71-5).
After the extended carpal tunnel incision, dissection is carried down through the transverse carpal ligament and distal antebrachial fascia to completely decompress the median nerve (Fig. 71-5).
 The nerve and all flexor tendons are retracted to expose the floor of the carpal tunnel, the transverse ligamentous rent, and lunate within the carpal tunnel if it had not been previously reduced (Fig. 71-6).
The nerve and all flexor tendons are retracted to expose the floor of the carpal tunnel, the transverse ligamentous rent, and lunate within the carpal tunnel if it had not been previously reduced (Fig. 71-6).
 The lunate can be manually reduced with dorsal pressure and some longitudinal traction.
The lunate can be manually reduced with dorsal pressure and some longitudinal traction.
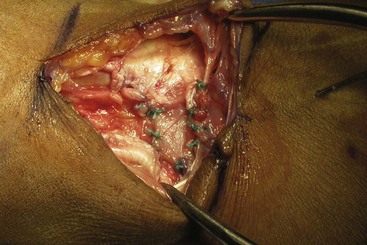
 The transverse ligamentous rent is repaired using multiple 3-0 braided nonabsorbable sutures (Fig. 71-7).
The transverse ligamentous rent is repaired using multiple 3-0 braided nonabsorbable sutures (Fig. 71-7).
Step 2: Dorsal Approach
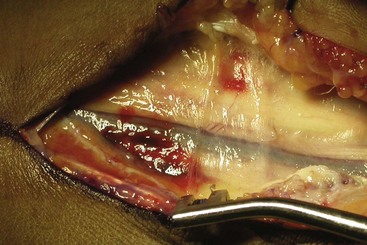
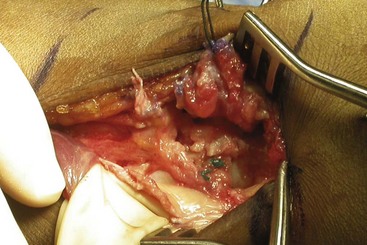
 After elevation and retraction of the EPL, deeper capsular exposure reveals the severe dorsal radiocarpal and intercarpal ligamentous damage (Fig. 71-8).
After elevation and retraction of the EPL, deeper capsular exposure reveals the severe dorsal radiocarpal and intercarpal ligamentous damage (Fig. 71-8).
 The ligament disruption often provides adequate exposure of the carpal bones; if not, a longitudinal capsulotomy is performed.
The ligament disruption often provides adequate exposure of the carpal bones; if not, a longitudinal capsulotomy is performed.
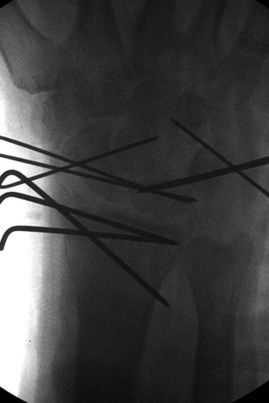
 A 0.062-inch K-wire is inserted into the lunate to use as a joystick for reduction.
A 0.062-inch K-wire is inserted into the lunate to use as a joystick for reduction.
 By means of the joystick, the lunate is made to be collinear with the longitudinal axis of the radius (as verified on the radiographs) and then held reduced with a temporary 0.062-inch dorsal radioulnate K-wire.
By means of the joystick, the lunate is made to be collinear with the longitudinal axis of the radius (as verified on the radiographs) and then held reduced with a temporary 0.062-inch dorsal radioulnate K-wire.
 Alternatively, a K-wire can be placed retrograde from the capitate through the lunate to hold the lunate reduction. Unlike the radiolunate wire, this wire does not need to be removed at the completion of the surgery.
Alternatively, a K-wire can be placed retrograde from the capitate through the lunate to hold the lunate reduction. Unlike the radiolunate wire, this wire does not need to be removed at the completion of the surgery.
Step 3
Step 4
Step 5
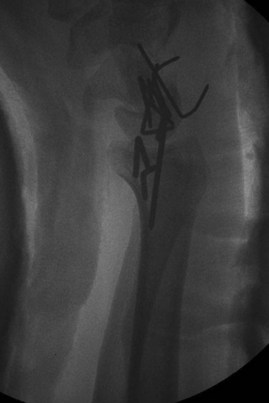
 Inspection of the SL and LT ligaments will determine the feasibility of ligamentous repair.
Inspection of the SL and LT ligaments will determine the feasibility of ligamentous repair.
 The ligaments may be avulsed from the scaphoid, lunate, or triquetrum or may be torn in midsubstance.
The ligaments may be avulsed from the scaphoid, lunate, or triquetrum or may be torn in midsubstance.
 If midsubstance tears are noted, repair is completed with 3-0 nonabsorbable sutures (Fig. 71-11).
If midsubstance tears are noted, repair is completed with 3-0 nonabsorbable sutures (Fig. 71-11).
 If bony avulsions are found, repair is completed with mini-suture anchors.
If bony avulsions are found, repair is completed with mini-suture anchors.
Postoperative Care and Expected Outcomes
 A bulky short arm thumb spica splint is applied postoperatively.
A bulky short arm thumb spica splint is applied postoperatively.
 The patient is seen at 2- to 3-week intervals for assessment of pin sites, and radiographs are taken to verify the reduction.
The patient is seen at 2- to 3-week intervals for assessment of pin sites, and radiographs are taken to verify the reduction.
 Severe injuries such as this often lead to restricted wrist range of motion and development of early wrist arthritis.
Severe injuries such as this often lead to restricted wrist range of motion and development of early wrist arthritis.
Hildebrand KA, Ross DC, Patterson SD, et al. Dorsal perilunate dislocations and fracture-dislocations: questionnaire, clinical, and radiographic evaluation. J Hand Surg [Am]. 2000;25:1069-1079.
Trumble T, Verheyden J. Treatment of isolated perilunate and lunate dislocations with combined dorsal and volar approach and intraosseous cerclage wire. J Hand Surg [Am]. 2004;29:412-417.