CASE 71
History: A 53-year-old man presents with hematemesis. Upper gastrointestinal endoscopy identified an extramucosal mass distorting the greater curvature of the stomach.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in Figures A to C? (Choose all that apply.)
D. Splenic artery pseudoaneurysm
E. Communicating peripancreatic fluid collection
2. The pancreas is a small organ. Several of its anatomic features allow acute pancreatitis to have a widespread impact. Which of the following is not one of these contributing features?
3. What is the condition in acute pancreatitis called when significant bleeding occurs?
D. Disseminated intravascular coagulopathy
4. What is the major cause of acute pancreatitis?
ANSWERS
CASE 71
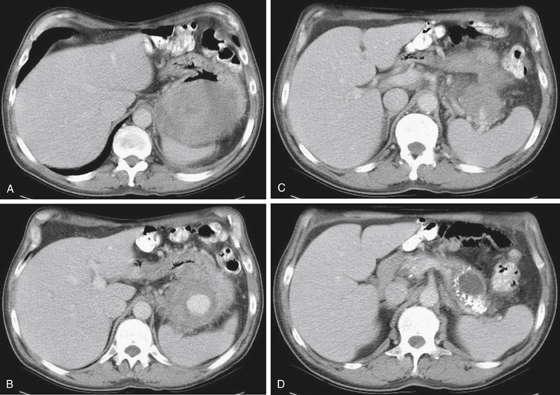
Hemorrhagic Pancreatitis
1. A, C, D, and E
2. D
3. C
4. A
References
Agrawal GA, Johnson PT, Fishman EK. Splenic artery aneurysms and pseudoaneurysms: clinical distinctions and CT appearances. Am J Roentgenol. 2007;188:992–999.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 155.
Comment
Pancreatitis is a relatively common inflammatory condition in which, for various reasons, autodigestion of the gland occurs, resulting in edema and fluid around the gland, swelling and loss of the normal planes around the gland, and, in the acute phase, almost invariably, changes at the left lung base secondary to diminished diaphragmatic excursion, hypoventilation, and resultant atelectasis and effusion. If a vessel is eroded, significant bleeding can occur, such as in this case. The incidence ranges from 20 to 30 cases per 100,000 population. The usual presentation is epigastric pain, sometimes radiating to the back, nausea, tachycardia, tachypnea, and often fever. Occasionally the patient is hypotensive, especially in severe hemorrhagic pancreatitis. The swollen head of the gland can impress the common bile duct, causing some degree of biliary obstruction.
The most common cause is alcohol abuse. However, other causes include endoscopic retrograde cholangiopancreatography (ERCP), trauma, gallstones, certain medications, penetrating peptic ulcers, and pancreatic divisum. One of the more interesting complications is splenic artery pseudoaneurysm (see figures). These pseudoaneurysms develop as a result of inflammation and enzymatic activity weakening a point in the splenic artery wall. Although this complication is unusual, if found it constitutes a danger to the patient of sudden life-threatening bleeding.