Procedure 70 Medial Femoral Condyle Vascularized Bone Flap for Scaphoid Nonunion
![]() See Video 52: Free Medial Femoral Condyle Vascularized Bone Transfer for Scaphoid Nonunion
See Video 52: Free Medial Femoral Condyle Vascularized Bone Transfer for Scaphoid Nonunion
Indications
 The main indication is a history of previously failed bone grafting, with plain radiographic and magnetic resonance imaging (MRI) evidence of avascular necrosis associated with scaphoid foreshortening.
The main indication is a history of previously failed bone grafting, with plain radiographic and magnetic resonance imaging (MRI) evidence of avascular necrosis associated with scaphoid foreshortening.
 If there are intraoperative findings showing no bleeding from the proximal and distal scaphoid, it is appropriate to reconstruct the defect with vascularized bone flap.
If there are intraoperative findings showing no bleeding from the proximal and distal scaphoid, it is appropriate to reconstruct the defect with vascularized bone flap.
 Another indication of medial femoral condyle vascularized bone flap is atrophic nonunion of a long bone with a small bone defect that is surrounded by poorly vascularized bed.
Another indication of medial femoral condyle vascularized bone flap is atrophic nonunion of a long bone with a small bone defect that is surrounded by poorly vascularized bed.
 If the nonunion site has punctate bleeding after débridement, corticocancellous wedge bone grafting through the dorsal approach for proximal pole nonunion and through the volar approach for waist nonunion with humpback deformity should be attempted.
If the nonunion site has punctate bleeding after débridement, corticocancellous wedge bone grafting through the dorsal approach for proximal pole nonunion and through the volar approach for waist nonunion with humpback deformity should be attempted.
Examination/Imaging
Imaging
 Posteroanterior (PA), lateral, and oblique radiographs of the hand should be taken to assess any dorsal intercalated segment instability (DISI) deformities or scaphoid foreshortening.
Posteroanterior (PA), lateral, and oblique radiographs of the hand should be taken to assess any dorsal intercalated segment instability (DISI) deformities or scaphoid foreshortening.
 Bone scans are useful in visualizing the fracture 4 hours after injury, but not for detection of a nonunion.
Bone scans are useful in visualizing the fracture 4 hours after injury, but not for detection of a nonunion.
 Computed tomography (CT) scans are useful in assessing pseudoarthrosis and show the extent of bone loss. Furthermore, they can pinpoint the exact position of the fractured fragments and determine whether there is any necrosis of the proximal pole. Humpback deformity may be revealed in sagittal views.
Computed tomography (CT) scans are useful in assessing pseudoarthrosis and show the extent of bone loss. Furthermore, they can pinpoint the exact position of the fractured fragments and determine whether there is any necrosis of the proximal pole. Humpback deformity may be revealed in sagittal views.
 An MRI with intravenous contrast (gadolinium) will help determine proximal pole vascularity. Cartilage erosions and osseous avascular necrosis are evaluated mainly in T1-weighted sequences.
An MRI with intravenous contrast (gadolinium) will help determine proximal pole vascularity. Cartilage erosions and osseous avascular necrosis are evaluated mainly in T1-weighted sequences.
Surgical Anatomy
Recipient Site: Vascular Anatomy of Scaphoid
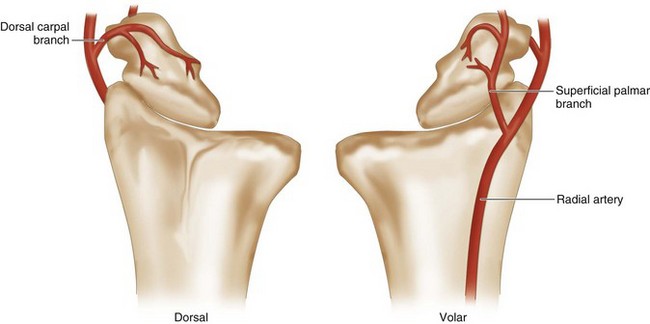
 The major blood supply to the scaphoid is through the radial artery, which enters through the dorsal ridge and supplies 70% to 80% of the intraosseous vascularity to the entire proximal pole. This vessel and its branches enter distally and dorsally in retrograde fashion to the scaphoid. The dorsal vessels travel proximally along the dorsal scaphoid ridge, and the majority of vessels enter the scaphoid waist and continue as intraosseous vessels. The scaphoid proximal pole is uniquely susceptible to avascular necrosis following fracture owing to high dependence on a single dominant retrograde traveling intraosseous vessel (Fig. 70-1).
The major blood supply to the scaphoid is through the radial artery, which enters through the dorsal ridge and supplies 70% to 80% of the intraosseous vascularity to the entire proximal pole. This vessel and its branches enter distally and dorsally in retrograde fashion to the scaphoid. The dorsal vessels travel proximally along the dorsal scaphoid ridge, and the majority of vessels enter the scaphoid waist and continue as intraosseous vessels. The scaphoid proximal pole is uniquely susceptible to avascular necrosis following fracture owing to high dependence on a single dominant retrograde traveling intraosseous vessel (Fig. 70-1).
 Volar radial artery branches provide the blood supply to 20% to 30% of the bone in the region of the distal tuberosity.
Volar radial artery branches provide the blood supply to 20% to 30% of the bone in the region of the distal tuberosity.
Donor Site: Medial Femoral Condyle
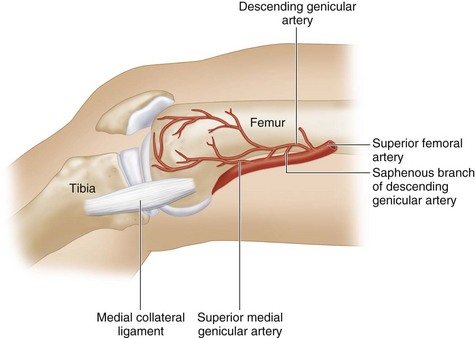
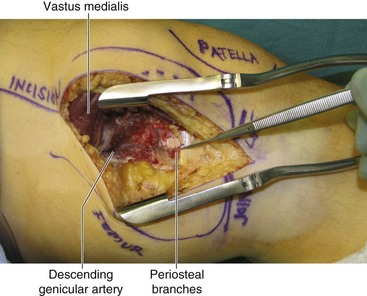
 The superficial femoral artery gives off the descending genicular artery branch just proximal to the adductor hiatus. The descending genicular artery travels distally and gives off a saphenous branch proximally and musculare branches distally. The superior medial genicular artery arises from the superficial femoral artery more distally.
The superficial femoral artery gives off the descending genicular artery branch just proximal to the adductor hiatus. The descending genicular artery travels distally and gives off a saphenous branch proximally and musculare branches distally. The superior medial genicular artery arises from the superficial femoral artery more distally.
 The descending genicular artery and superior medial genicular artery continue distally, penetrate the bone, and provide the blood supply to the medial femoral condyle as intraosseous nutrient vessels.
The descending genicular artery and superior medial genicular artery continue distally, penetrate the bone, and provide the blood supply to the medial femoral condyle as intraosseous nutrient vessels.
 The saphenous branch of the descending genicular artery supplies the medial femoral condyle skin flap (Fig. 70-2).
The saphenous branch of the descending genicular artery supplies the medial femoral condyle skin flap (Fig. 70-2).
Exposures
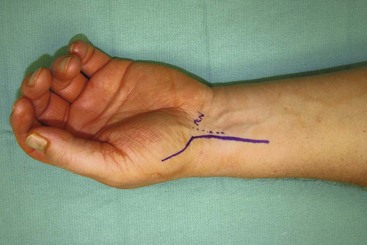
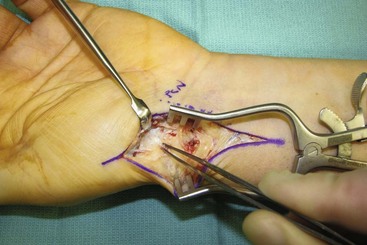
 The scaphoid and radial artery are exposed by a palmar incision. This curvilinear incision extends proximally from the radial aspect of the thenar eminence parallel and radial to the flexor carpi radialis (Fig. 70-3).
The scaphoid and radial artery are exposed by a palmar incision. This curvilinear incision extends proximally from the radial aspect of the thenar eminence parallel and radial to the flexor carpi radialis (Fig. 70-3).
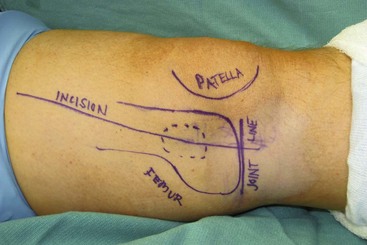
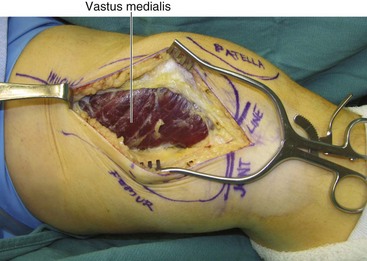
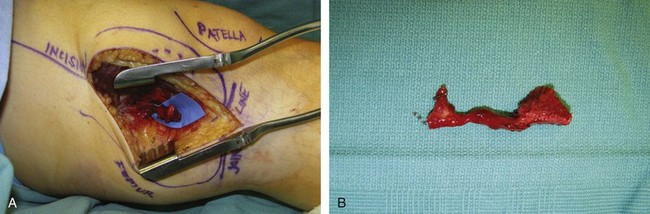
 The medial femoral condyle of the ipsilateral medial knee and its nutrient vessels are exposed using a longitudinal lower medial thigh incision (Fig. 70-4).
The medial femoral condyle of the ipsilateral medial knee and its nutrient vessels are exposed using a longitudinal lower medial thigh incision (Fig. 70-4).
Procedure
Team 1: Donor Site (Bone Graft Harvest)
Step 1
Step 2
Step 3
Step 4
Step 5
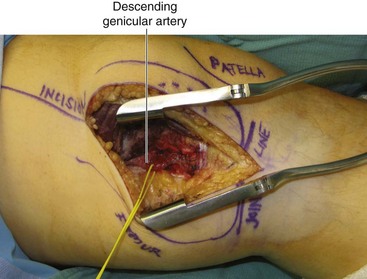
 Based on the size of the defect, a rectangular medial femoral condyle bone graft is selected at the area where the distal nutrient branches of the descending genicular artery penetrate into the bone.
Based on the size of the defect, a rectangular medial femoral condyle bone graft is selected at the area where the distal nutrient branches of the descending genicular artery penetrate into the bone.
 The size of the bone graft should be sufficient to fill the defect. Bone graft from this location has sufficient cortical bone to provide a strong strut to correct the humpback deformity of the scaphoid. The distal radius bone graft typically does not have sufficient cortical bone strong enough to buttress the bone defect. The bone graft is usually 10 to 12 mm in thickness.
The size of the bone graft should be sufficient to fill the defect. Bone graft from this location has sufficient cortical bone to provide a strong strut to correct the humpback deformity of the scaphoid. The distal radius bone graft typically does not have sufficient cortical bone strong enough to buttress the bone defect. The bone graft is usually 10 to 12 mm in thickness.
Step 6
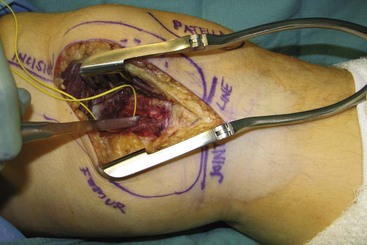
 The periosteum is sharply incised using a no. 15 blade, and the bone is cut with a small osteotome along the marking line (Fig. 70-8).
The periosteum is sharply incised using a no. 15 blade, and the bone is cut with a small osteotome along the marking line (Fig. 70-8).
Step 7
Team 2: Recipient Site Preparation and Microanastomosis
Step 2
 The FCR sheath is opened, the tendon retracted ulnarly, and the floor of the FCR tunnel sharply incised longitudinally to expose the radiocarpal joint at the level of the scaphoid (Fig. 70-10).
The FCR sheath is opened, the tendon retracted ulnarly, and the floor of the FCR tunnel sharply incised longitudinally to expose the radiocarpal joint at the level of the scaphoid (Fig. 70-10).
Step 2 Pearls
The radioscaphocapitate (RSC) and long radiolunate (LRL) ligaments are identified and incised. Much of the LRL and a portion of the RSC are left intact to help stabilize the proximal pole.
Preserving this ligamentous support also helps maintain fracture reduction.
Volar capsulotomy in the scaphotrapezial joint is performed to improve the visualization of the scaphoid.
Step 3
 The scaphoid is then examined, paying attention to the articular cartilage of the radioscaphoid and midcarpal joints.
The scaphoid is then examined, paying attention to the articular cartilage of the radioscaphoid and midcarpal joints.
 A Freer elevator is used to define the location of the nonunion and the borders of the scaphoid.
A Freer elevator is used to define the location of the nonunion and the borders of the scaphoid.
 Fibrous and/or necrotic tissues at the proximal and distal poles are examined carefully. A small curet or rongeur is used for débridement and removal of intervening fibrotic tissue (Fig. 70-11).
Fibrous and/or necrotic tissues at the proximal and distal poles are examined carefully. A small curet or rongeur is used for débridement and removal of intervening fibrotic tissue (Fig. 70-11).
Step 4
 The tourniquet is deflated to assess punctate bleeding from the nonunion site.
The tourniquet is deflated to assess punctate bleeding from the nonunion site.
 The absence of punctate bleeding suggests avascularity, and further débridement is performed until punctate bleeding is confirmed (Fig. 70-12).
The absence of punctate bleeding suggests avascularity, and further débridement is performed until punctate bleeding is confirmed (Fig. 70-12).
 The size of the bony defect is measured after débridement.
The size of the bony defect is measured after débridement.
 A slow-speed bur is helpful to débride the fibrous nonunion, but the scaphoid must be constantly irrigated during burring to prevent additional bone necrosis.
A slow-speed bur is helpful to débride the fibrous nonunion, but the scaphoid must be constantly irrigated during burring to prevent additional bone necrosis.
Step 5
Step 7
 The bone graft harvested from the medial femoral condyle is further shaped to fit the defect.
The bone graft harvested from the medial femoral condyle is further shaped to fit the defect.
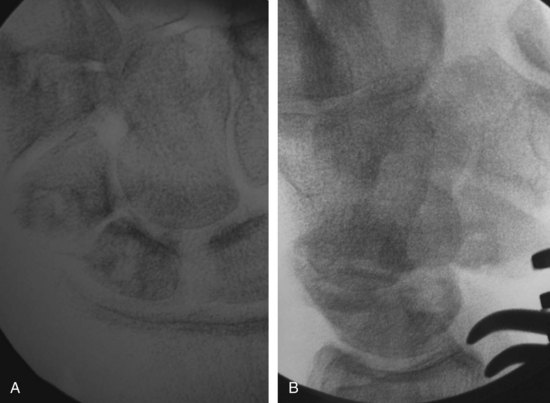
 The flap is inserted into the defect, and Kirschner wires (or headless cannulated screws) are passed through the scaphoid and bone flap for fixation under fluoroscopic imaging to confirm correction of the scaphoid shortening and DISI deformity (Fig. 70-14).
The flap is inserted into the defect, and Kirschner wires (or headless cannulated screws) are passed through the scaphoid and bone flap for fixation under fluoroscopic imaging to confirm correction of the scaphoid shortening and DISI deformity (Fig. 70-14).
 The K-wires should be left under the skin and removed when the bone has healed, typically 3 months after surgery.
The K-wires should be left under the skin and removed when the bone has healed, typically 3 months after surgery.
Step 8
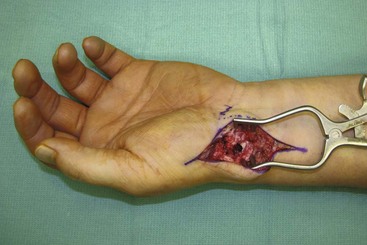
 The recipient artery (descending genicular artery or superior medial genicular artery) is anastomosed to the radial artery in an end-to-side fashion using 9-0 nylon sutures under microscopic magnification.
The recipient artery (descending genicular artery or superior medial genicular artery) is anastomosed to the radial artery in an end-to-side fashion using 9-0 nylon sutures under microscopic magnification.
 The venae comitantes of the descending genicular artery or superior medial genicular artery is anastomosed to the venae comitantes of the radial artery or to the cephalic vein in an end-to-end fashion by 9-0 nylon sutures (Fig. 70-15).
The venae comitantes of the descending genicular artery or superior medial genicular artery is anastomosed to the venae comitantes of the radial artery or to the cephalic vein in an end-to-end fashion by 9-0 nylon sutures (Fig. 70-15).
Step 9
 After microanastomosis, the wound is closed with 4-0 nylon sutures (Fig. 70-16).
After microanastomosis, the wound is closed with 4-0 nylon sutures (Fig. 70-16).
 A hand-held Doppler is used to detect the signal of arterial anastomosis, and the location is marked for postoperative monitoring.
A hand-held Doppler is used to detect the signal of arterial anastomosis, and the location is marked for postoperative monitoring.
 A thumb spica dorsal short-arm splint is applied to keep the thumb abducted and the wrist in slight flexion.
A thumb spica dorsal short-arm splint is applied to keep the thumb abducted and the wrist in slight flexion.
Postoperative Care and Expected Outcomes
 The splint maintains the thumb in abduction and the wrist in slight flexion for 2 weeks.
The splint maintains the thumb in abduction and the wrist in slight flexion for 2 weeks.
 The stitches are removed 2 weeks after surgery, and thumb spica short-arm cast or splint (for a reliable patient) is applied for 8 to 12 weeks until the vascularized bone graft is united. CT scan can confirm healing of the scaphoid before allowing the patient to initiate unrestricted activities.
The stitches are removed 2 weeks after surgery, and thumb spica short-arm cast or splint (for a reliable patient) is applied for 8 to 12 weeks until the vascularized bone graft is united. CT scan can confirm healing of the scaphoid before allowing the patient to initiate unrestricted activities.
 The thigh is immobilized for a few days postoperatively until the patient feels comfortable.
The thigh is immobilized for a few days postoperatively until the patient feels comfortable.
Doi K, Hattori Y. Vascularized bone graft from the supracondylar region of the femur. Microsurgery. 2009;29:379-384.
Jones DBJr, Burger H, Shin AY, et al. Treatment of scaphoid waist nonunions with an avascular proximal pole and carpal collapse: a comparison of two vascularized bone grafts. J Bone Joint Surg [Am]. 2008;90:2616-2625.