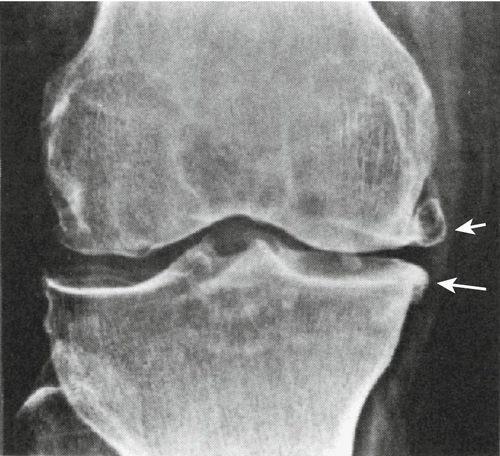
CHAPTER 70
Knee Osteoarthritis
Michael Sein, MD; Allen N. Wilkins, MD; Edward M. Phillips, MD
Definition
Osteoarthritis is steadily becoming the most common cause of disability for the middle-aged and has become the most common cause of disability for those older than 65 years [1]. The knee joint is the most common site for lower extremity osteoarthritis [2]. It is estimated that nearly half of all adults will have symptomatic knee osteoarthritis in their lifetimes [3]. In addition to the growing population of elderly patients with knee osteoarthritis, an increasing number of former athletes with previous knee injuries may experience post-traumatic knee osteoarthritis. Osteoarthritis of the knee results from mechanical and idiopathic factors. Osteoarthritis alters the balance between degradation and synthesis of articular cartilage and subchondral bone.
Osteoarthritis can involve any or all of the three major knee compartments: medial, patellofemoral, or lateral. The medial compartment is most often involved, leading to medial joint space collapse and thus to a genu varum (bowleg) deformity. Lateral compartment involvement may lead to a genu valgum (knock-knee) deformity. Isolated disease of the patellofemoral joint occurs in up to a quarter of patients with osteoarthritis of the knee [4]. Arthritis in one compartment may, through altered biomechanical stress patterns, eventually lead to involvement of another compartment.
Osteoarthritis affects all structures within and around a joint. Hyaline articular cartilage is lost. Bone remodeling occurs, with capsular stretching and weakness of periarticular muscles. Synovitis is present in some cases and ligamentous laxity occurs. Lesions in the bone marrow may also develop, which may suggest trauma to bone [5]. Osteoarthritis involves the joint in a nonuniform and focal manner. Localized areas of loss of cartilage can increase focal stress across the joint, leading to further cartilage loss. With a large enough area of cartilage loss or with bone remodeling, the joint becomes tilted, and malalignment develops.
The threat of knee osteoarthritis is not only a concern for elderly populations. Malalignment is the most potent risk factor for structural deterioration of the knee joint [6]. By further increasing the degree of focal loading, malalignment creates a vicious circle of joint damage that ultimately can lead to joint failure. The role of obesity as a risk factor for knee osteoarthritis has been well documented. A large, population-based prospective study found that the risk for knee osteoarthritis was seven times greater for people with a body mass index of 30 or higher compared with those with a body mass index below 25 [7]. Moreover, women (of average height) who lost 5 kg of weight reduced their risk of symptomatic knee osteoarthritis by 50% [8].
Sports injuries and vigorous physical activity are considered to be important risk factors in knee osteoarthritis. Elite athletes who take part in high-impact sports, such as soccer and ice hockey, have an increased risk of knee osteoarthritis [9]. It is unclear whether the increased risk in this particular study was directly related to traumatic injury. However, it has been suggested in another study that subjects with a history of knee injury are at a fivefold to sixfold increased risk for development of knee osteoarthritis [10]. Knee osteoarthritis is common in those performing heavy physical work, especially if this involves knee bending, squatting, kneeling, or repetitive use of joints [11]. It is unclear if the association of knee osteoarthritis with these work-related activities is secondary to the nature of the work or the increased likelihood of injury.
Symptoms
Knee osteoarthritis is characterized by joint pain, tenderness, decreased range of motion, crepitus, occasional effusion, and often inflammation of varying degrees. Initial osteoarthritis symptoms are generally minimal, given the gradual and insidious onset of the condition. Pain typically occurs around the knee, particularly during weight bearing, and decreases with rest. With progression of the disease, pain can persist even at rest. Activities associated with osteoarthritic pain are climbing stairs, getting out of a chair, getting in and out of a car, and walking long distances. Pain may also radiate to adjacent sites as osteoarthritis indirectly alters the biomechanics of other anatomic structures, such as ligaments, muscles, nerves, and veins.
Joint stiffness may occur after periods of inactivity, such as after awakening in the morning or prolonged sitting. Patients often report higher pain levels in the morning but usually for less than 30 minutes. Patients often experience limitation of movement because of joint stiffness or swelling. Many patients report a “locking” or a “catching” sensation, which is probably due to a variety of causes, including debris from degenerated cartilage or meniscus in the joint, increased adhesiveness of the relatively rough articular surfaces, muscle weakness, and even tissue inflammation. Stiffness can discourage mobility. This initiates a cycle that results in deconditioning, decreased function, and increased pain.
Barometric changes, such as those associated with damp, rainy weather, will often increase pain intensity. Patients often note that their knees “give way” or feel unstable at times.
Physical Examination
Examination of the patient includes testing for various possible causes of knee pain (see section on differential diagnosis). Therefore the entire limb, from the hip to the ankle, is examined. It is important to identify findings such as quadriceps weakness or atrophy and knee and hip flexion contractures. Gait should be observed for presence of a limp, functional limb length discrepancy, or buckling. Genu varum or valgum is often better appreciated when the patient is standing.
The affected knee should be compared with the contralateral uninvolved knee. Knee examination may reveal decreased knee extension or flexion secondary to effusion or osteophytes (both of which may be palpable). Osteophytes along the femoral condyles may be palpated, especially along the medial distal femur. Palpation may reveal patellar or parapatellar tenderness. Crepitation, resulting from juxtaposition of roughened cartilage surfaces, may be appreciated along the joint line when the knee is flexed or extended. A mild effusion and tenderness may be appreciated along the medial joint line or at the pes anserine bursa. Ligament testing may reveal laxity of one or both of the collateral ligaments. Lateral subluxation of the patella may be found in patients with genu valgum (Table 70.1). Another clue on examination that the patient probably has knee osteoarthritis is the finding of visible bone enlargements (exostoses) of the fingers. At the distal interphalangeal joints, these are referred to as Heberden nodes; at the proximal interphalangeal joints, they are known as Bouchard nodes, usually a slightly later finding.
Table 70.1
Typical Physical Examination Findings in Knee Osteoarthritis
| Inspection | Bone hypertrophy Varus deformity from preferential medial compartment involvement |
| Palpation | Increased warmth Joint effusion Joint line tenderness |
| Range of motion | Painful knee flexion Decreased joint flexion secondary to pain Crepitus (coarse) |
| Joint stability | Mediolateral instability |
The findings of the neurologic examination are typically normal, with the exception of decreased muscle strength, particularly in the quadriceps, due to disuse or guarding secondary to pain.
Diagnostic Studies
Osteoarthritis is diagnosed clinically on the basis of history and physical examination. Imaging, however, can be used to confirm the diagnosis and to rule out other conditions. Radiographic abnormalities can be found both in joint areas subjected to excessive pressure and in joint areas subjected to diminished pressure. These changes include joint space narrowing, subchondral sclerosis, and bone cysts in weight-bearing regions of the joint and osteophytes in low-pressure areas, especially along the marginal regions of the joint. Joint space narrowing is the initial finding, followed by subchondral sclerosis, then by osteophytes, and finally by cysts with sclerotic margins (known as synovial cysts, subchondral cysts, subarticular pseudocysts, or necrotic pseudocysts).
Radiographic evidence of osteoarthritis is not well correlated with symptoms [12]. Results have been conflicting, probably because of the differences in populations studied and radiographic and clinical criteria used. The presence of osteophytes had a strong association with knee pain, whereas the absence or presence of joint space narrowing was not associated with pain [13].
Knee pain severity was a more important determinant of functional impairment than radiographic severity of osteoarthritis [14,15]. There was no correlation between joint space narrowing and a disability score (Western Ontario and McMaster Universities Osteoarthritis index, WOMAC) at a single time point [15].
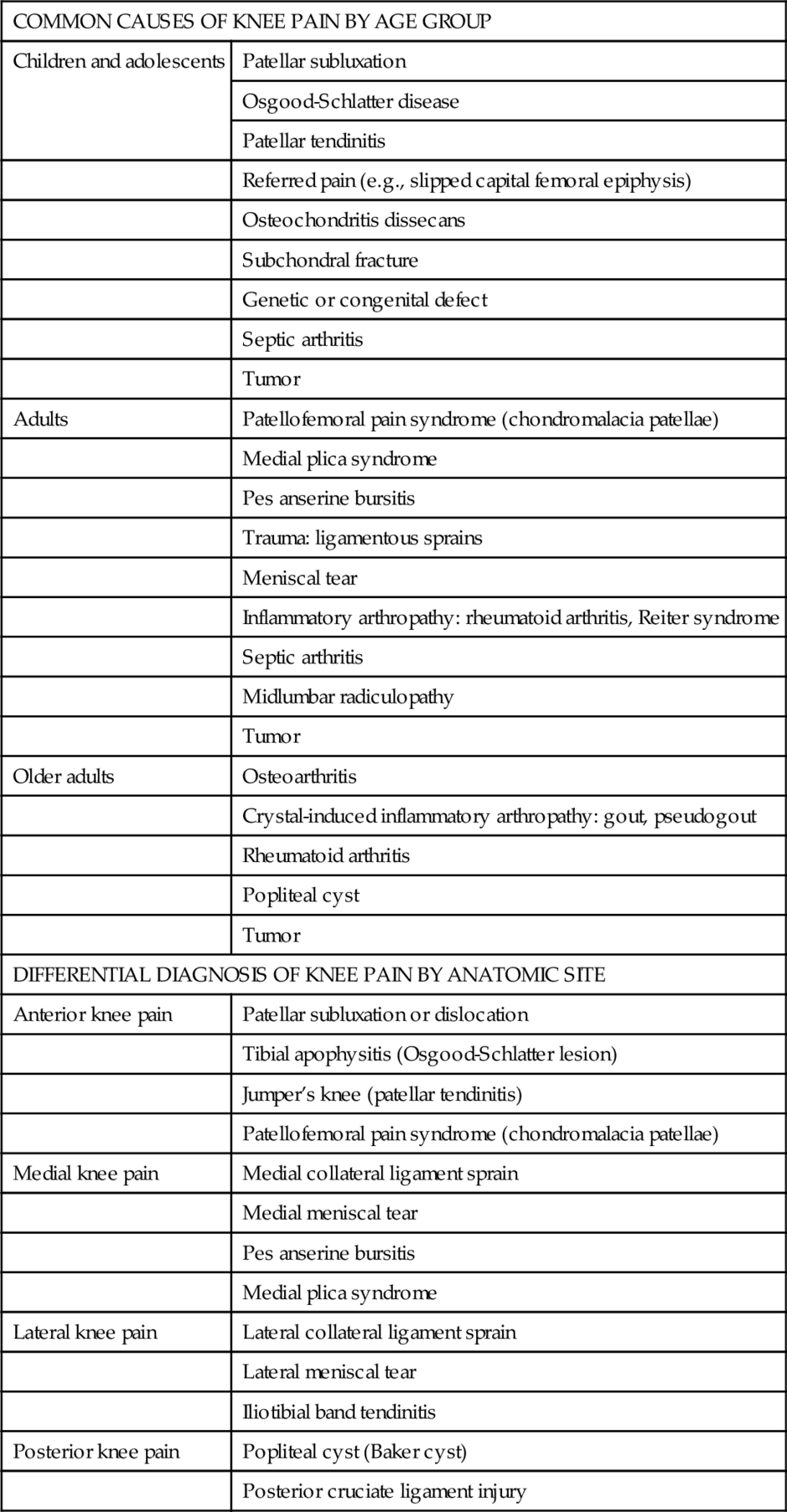
Osteophytes alone are associated with aging rather than with osteoarthritis. Indications for plain x-ray films include trauma, effusion, symptoms not readily explainable by physical examination findings, severe pain, presurgical planning, and failure of conservative management. Recommended films are weight-bearing (standing) anteroposterior, lateral, and patellar views. Radiographs taken during weight bearing with the knee in full extension and partial flexion may reveal a constellation of findings associated with osteoarthritis, including asymmetric narrowing of the joint space (typically medial compartment), osteophytes, sclerosis, and subchondral cysts (Fig. 70.1). A Merchant view specifically evaluates the patellofemoral space. Non–weight-bearing lateral views may help in the evaluation of the patellofemoral and tibiofemoral joint spaces. Tunnel views can help visualize loose osteochondral bodies.
Magnetic resonance imaging usually adds little but cost to the entire evaluation of osteoarthritis of the knee. It may reveal changes that suggest the presence of osteoarthritis. However, it is not indicated in the initial evaluation of older persons with chronic knee pain. Magnetic resonance imaging may detect incidental findings, such as meniscal tears, that are common in middle-aged and older adults with and without knee pain. Musculoskeletal ultrasonography has potential for detecting bone erosions, synovitis, tendon disease, and enthesopathy. It has a number of distinct advantages over magnetic resonance imaging, including good patient tolerability and ability to scan multiple joints in a short time. However, there are scarce data about its validity, reproducibility, and responsiveness to change, making interpretation and comparison of studies difficult. In particular, there are limited data describing standardized scanning methodology and standardized definitions of ultrasound pathologic changes [16].
Laboratory test results are typically normal, but analysis may be undertaken, especially for elderly patients, to establish a baseline (e.g., blood urea nitrogen concentration, creatinine concentration, or liver function tests before use of nonsteroidal anti-inflammatory drugs or acetaminophen) or to exclude other conditions such as rheumatoid arthritis. Synovial fluid analysis should not be undertaken unless destructive, crystalline, or septic arthritis is suspected.
Treatment
Initial
The PRICE regimen may help provide initial relief for patients in pain: protection with limited weight bearing by use of a cane or modification of exercise to reduce stress; relative rest (or taking adequate rests throughout the day, avoiding prolonged standing, climbing of stairs, kneeling, deep knee bending); ice (applied while the skin is protected with a towel for up to 15 minutes at a time several times a day; note, however, that some patients with chronic pain may find better relief with moist heat); compression (if swelling exists, wrapping with an elastic bandage or a sleeve may help); and elevation (may help diminish swelling, if it is present). There are a wide variety of initial treatment options for knee arthritis. Current guidelines put forth by the American College of Rheumatology emphasize the use of acetaminophen as a first-line therapy for osteoarthritis [17]. Other options include oral and topical nonsteroidal anti-inflammatory drugs; topical capsaicin cream; and nutritional intervention, such as glucosamine sulfate and chondroitin sulfate (Table 70.2). Orthotics and footwear are also included in the list of treatment options and are discussed further in the next section.
Table 70.2
Pharmacologic and Supplemental Nutrition Treatment Options
| Medication | Related Details |
| Acetaminophen | The maximum dosage is 4 g/day in patients with normal hepatic function. |
| Oral NSAIDs | Studies show almost equal efficacy among traditional NSAIDs [18]. A randomized prospective study demonstrated equal efficacy between selective cyclooxygenase 2 inhibitors and traditional NSAIDs [19]. |
| Tramadol-acetaminophen | American Pain Society guidelines recommend tramadol-acetaminophen for treatment of osteoarthritis pain when NSAIDs alone cannot provide adequate relief. It is considered safe and effective in a subset of elderly patients [20]. |
| Oxycodone | Patients with moderate to severe pain from osteoarthritis can achieve effective pain relief without deterioration in function when opioids are included as part of a comprehensive pain management program [21]. |
| Topical NSAIDs | A quantitative systematic review of 86 trials evaluating the efficacy of topical NSAIDs in osteoarthritis and tendinitis found them significantly more effective than placebo [22]. |
| Topical capsaicin | Limited data from controlled trials have shown improvements with capsaicin [23]. |
| Glucosamine sulfate (1500 mg orally qd) and chondroitin sulfate (1200 mg orally qd) | One large randomized clinical trial found that glucosamine and chondroitin sulfate alone or in combination did not reduce pain effectively in the overall group of patients with osteoarthritis of the knee. However, the combination of glucosamine and chondroitin sulfate was effective in the subgroup of patients with moderate to severe knee pain [24]. |
NSAIDs, nonsteroidal anti-inflammatory drugs.
Rehabilitation
Exercise
Exercises are likely to be most effective if they train muscles for the activities a person performs daily [25]. Randomized studies support the benefits of exercise, even if it is home based, on pain and function in patients with osteoarthritis [26]. Because there is currently no cure for osteoarthritis, most research continues to evaluate the use of exercise as a treatment to alleviate symptoms of the disease and to enhance functional capacity. Two meta-analyses published in 2004 focus specifically on the efficacy of strengthening [27] and aerobic exercise [28] for osteoarthritis.
With regard to muscle strengthening, improvements in strength, pain, function, and quality of life were noted. However, there was no evidence that the type of strengthening exercise influences outcome. Static or dynamic strengthening exercises can maintain or improve periarticular muscle strength, thereby reversing or preventing biomechanical abnormalities and their contribution to joint dysfunction and degeneration.
With regard to aerobic exercise, results indicated that aerobic exercise alleviates pain and joint tenderness and promotes functional status and respiratory capacity. Aerobic exercise improves activity tolerance, increases pain threshold, and can have positive effects on mood and motivation for participation in other activities. Whereas strengthening appears superior to aerobic exercise in the short term for specific impairment-related outcomes (e.g., pain), aerobic exercise appears more effective for functional outcomes in the longer term. There is also evidence that exercise can improve proprioception [27], thus improving biomechanics and protective responses.
Attempts to maintain function can be helped through non–weight-bearing strengthening, especially of the quadriceps. For patients with greater pain, this can be done with static exercise or through water aerobics, which allows motion at the knee with reduced joint loads. Exercise bicycles and walking should be recommended to enhance aerobic capacity. Deep knee bends in the presence of effusion should be avoided. Particular attention must be paid to strengthening of the medial quadriceps in patients with genu valgum who have lateral subluxation of the patella. Maintaining activity is critical to maintaining function. Even those patients scheduled for total knee arthroplasty should pursue static and dynamic strengthening as well as cardiovascular conditioning preoperatively to ease the postoperative rehabilitation [29].
Therapeutic Modalities
Transcutaneous electrical nerve stimulation (TENS), the application of an electrical current through the skin with the aim of pain modulation, is a frequently used modality in knee osteoarthritis. Although this is a popular treatment option, research supporting its efficacy is lacking. The treatment is supported only by a few small, short-term trials. In a small-scale, randomized, double-blind crossover trial comparing active and placebo TENS for symptomatic knee osteoarthritis in subjects who were considered to be candidates for total knee replacement, patients reported significantly more pain relief and less medication use with active TENS therapy than with the placebo [30]. For most patients, pain relief was experienced only during periods of active use of the device, although the beneficial effect was sustained for several hours in a few. Despite the positive results in these small trials, a meta-analysis could not confirm this modality’s effectiveness. The systematic review attributed inconclusive results to questionable methodologic quality and a high degree of heterogeneity among trials [31].
Additional therapeutic modalities, such as electrical stimulation or massage, may also be used. Therapists may also review postural alignment and joint positioning techniques, especially for when the patient is sleeping. In particular, the use of a pillow under bent knees, much favored by many patients when they are supine, should be avoided because resulting knee flexion contractures, even if small, can significantly increase stresses on the knee during gait. Stretching of the hamstrings and quadriceps may also prove beneficial. Patients should be counseled against prolonged wearing of high heels, which is associated with medial knee osteoarthritis [32].
Adaptive Equipment
Adaptive equipment, such as a cane or walker, can reduce hip or knee loading, thereby reducing pain. It may also prevent falls in patients with impaired balance. Proper training in the use of a cane is important because it reduces joint loading in the contralateral hip but amplifies forces in the ipsilateral hip.
Bracing and Footwear
The basic rationale for a knee brace for unicompartmental knee osteoarthritis is to improve function by reducing the patient’s symptoms. This can be accomplished, in theory, by reducing the biomechanical load on the affected compartment of the knee. Clinical trials are generally small and difficult to control adequately because of the nature of knee braces and the difficulty in designing a trial with a true placebo. Also, each brace has a unique design and may have features that make it more or less acceptable to the patient. Therefore clinical trials done with one brace design may not be applicable to all osteoarthritis knee braces.
A review of the published literature on knee bracing for osteoarthritis points out some of the limitations of the clinical trials to date but acknowledges the limited evidence for improvement in pain and function in patients using osteoarthritis braces compared with medical treatment or neoprene sleeves [33].
In patients with osteoarthritis and varus malalignment of the knees, a shoe wedge (thicker laterally) moves the center of loading laterally during walking, a change that extends from foot to knee, lessening medial load across the knee. Although such modifications to footwear decrease varus malalignment [34], one randomized trial [35] showed no reduction in pain compared with a neutral insert. However, a review of the published literature on the efficacy of laterally wedged foot orthotics for improving these symptoms does indicate a strong scientific basis for applying wedged insoles in an attempt to reduce pain in patients with medial compartment knee osteoarthritis [36].
Tilting or malalignment of the patella may cause patellofemoral pain. Patellar realignment with the use of braces or tape to pull the patella back into the trochlear sulcus of the femur or to reduce its tilt may lessen pain. In clinical trials with tape to reposition the patella into the sulcus without tilt, knee pain was reduced compared with placebo [37,38]. However, patients may find it difficult to apply tape, and skin irritation is common. Commercial patellar braces are also available, but their efficacy has not been studied formally.
Heel lifts or built-up shoes may be required in the presence of leg length discrepancy to prevent compensatory knee flexion gait on the longer side. In the presence of knee deformity, therapists can also evaluate for altered biomechanics (e.g., genu varum may lead to femoral internal torsion, resulting in compensatory external rotation of the tibia, which predisposes the patient to increased arthritic changes). Therapists can also visit the homes and workplaces of patients to suggest adjustments, such as raised toilet seats, grab bars, reachers, and the like.
Acupuncture
Acupuncture, a technique in existence for thousands of years, has gained renewed interest as a treatment of osteoarthritis. A multicenter, 26-week National Institutes of Health–funded randomized controlled trial found acupuncture to be effective as adjunctive therapy for reducing pain and improving function in patients with knee osteoarthritis [39].
Procedures
Intra-articular corticosteroid injections may help in reduction of local inflammation and improvement of symptoms. The response is generally rapid but may not be sustained in the longer term. A systematic review of intra-articular corticosteroid injections demonstrated evidence of pain reduction at 2 weeks and at 3 weeks after intervention. At 4 to 24 weeks after injection, evidence of an effect on pain and function was lacking [40]. Because the corticosteroid is delivered directly, systemic toxicity is minimized. Intra-articular corticosteroid injections should be given no more than two or three times a year to reduce potential damage to cartilage from the steroids. Given the short-term effect and limitation on injection frequency, corticosteroid injection is most often used as an adjunctive therapy for acute or severe symptom flares (Fig. 70.2). Table 70.3 lists potential systemic side effects of corticosteroid injections. Administration of steroids through iontophoresis may be an alternative for patients hesitant to undergo injections.
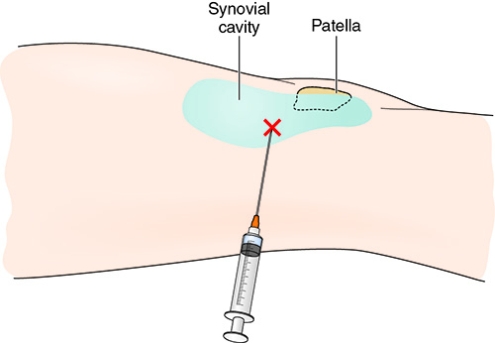
Table 70.3
Minimizing Potential Side Effects of Intra-articular Corticosteroid Injection
| Side Effect | Ways to Minimize Risk |
| Systemic effects | Avoid high doses and multiple simultaneous injections; use accurate injection techniques |
| Tendon rupture, fat atrophy, muscle wasting, skin pigment changes | Avoid misdirected injections |
| Septic arthritis | Use sterile technique; withhold therapy in at-risk patients |
| Nerve and blood vessel damage | Use accurate injection techniques |
| Postinjection symptom flare or synovitis | Avoid the same preparation for future injections |
| Flushing | Avoid high doses |
| Anaphylaxis | Take careful drug allergy history |
| Steroid arthropathy | Avoid high doses and overly frequent injections |
The authors’ preferred technique for intra-articular injection of the knee is as follows. With the patient supine, under sterile conditions with use of a 25-gauge needle, 2 or 3 mL of local anesthetic (e.g., 1% lidocaine) is injected just posterior to the upper lateral pole of the patella. Alternatively, ethyl chloride spray can be used. Then, by use of a 11⁄2-inch, 22- to 25-gauge needle, either local steroid (e.g., methylprednisolone, 20 to 40 mg/mL) or hyaluronic acid is injected in the same region (these products are available in 2-mL vials or prefilled syringes, one injection per vial). If a knee effusion exists, it may be necessary to drain the effusion to avoid dilution of the medications. This is ideally done with an 18- to 20-gauge needle. Switching of the syringes while the needle remains in place prevents additional trauma. Postinjection care includes local icing for 5 to 10 minutes. Patients are advised to avoid excessive weight bearing for 24 to 48 hours after an injection.
Viscosupplementation with hyaluronic acid, available as naturally occurring hyaluronan or synthetic hylan G-F 20, may be helpful. The rationale for using viscosupplementation is to impart protective properties to synovial fluid, including shock absorption, energy dissipation, and lubrication of the articular cartilage surface [41]. Hyaluronan is administered in a series of five weekly injections; hylan G-F 20 is given in three weekly injections. Treatments are typically repeated two to four times per year. Clinical trials of viscosupplementation have demonstrated limited efficacy in pain relief [42]. Compared with corticosteroid injection, the effect of hyaluronic acid appears to be less dramatic but more durable. In a meta-analysis comparing both interventions, hyaluronic acid was less effective for pain relief in the first 4 weeks after injection [43]. By week 4, the two approaches had equal efficacy. Beyond week 8, hyaluronic acid had a greater effect [43]. Side effects included local inflammation and increased pain at the injection site. There is no evidence that hyaluronan injection in humans alters biologic processes or progression of cartilage damage. The hyaluronic acid is injected into the knee in the same manner as the intra-articular steroid is administered.
Surgery (Table 70.4)
Most would agree that the term arthroscopic débridement includes lavage and the removal of loose bodies, debris, mobile fragments of articular cartilage, unstable torn menisci, and impinging osteophytes. However, it is clear from the literature that drilling, abrasion chondroplasty, microfracture, saucerization, notchplasty, osteophyte removal, synovectomy, and arthrolysis are also performed simultaneously in many clinical series. Patients who have a short history and a sudden onset of mechanical symptoms and also have knee effusions are likely to do best [44]. Meniscal symptoms and signs, synovitis or synovial impingement, osteophytic impingement, and catching or locking caused by loose bodies favor a good outcome. Significant instability and malalignment are poor prognostic factors. Patients who have radiographic signs of advanced degeneration are unlikely to benefit [45].
Table 70.4
Surgical Options for Osteoarthritis of the Knee
| Established Techniques | Indications | Outcome |
| Arthroscopic débridement | Knee effusions Meniscal signs and symptoms Synovitis Osteophytic impingement Catching or locking caused by loose bodies |
Most reports show improvement in 50% to 80% of patients; however, results deteriorate with time |
| Osteotomy of the proximal tibia or distal femur | Predominantly medial compartment involvement | Recovery is prolonged Relief of symptoms often incomplete |
| Unicompartmental knee replacement | Predominantly medial compartment involvement Minimal lateral compartment disease No major anterior knee pain Stable knee joint Correctable varus deformity Fixed flexion deformity of less than 10 degrees |
Survivorship rate for implants of 90% at 20 years |
| Patellofemoral replacement | Isolated patellofemoral joint involvement | Results have been variable |
| Total knee replacement | Tricompartmental disease | Survival rates of between 84% and 98% at 15 years |
Although arthroscopic surgery has been widely used for osteoarthritis of the knee, scientific evidence to support its efficacy is lacking. Most of the orthopedic literature supporting its use is based on retrospective studies, with authors reporting improvement in 50% to 80% of patients [46,47]. However, in a randomized, controlled trial, arthroscopic surgery for osteoarthritis of the knee provided no additional benefit to optimized physical and medical therapies [48].
Up to a quarter of patients with osteoarthritis of the knee have predominantly arthritis of the medial compartment. The surgical options for such patients are medial unicompartmental knee replacement, proximal tibial or distal femoral osteotomy, and total knee replacement (see Chapter 80). Osteotomy is a less drastic measure than knee replacement and is often favored by younger, active patients with unicompartmental symptoms. In osteotomy, a wedge-shaped piece of bone is removed from either the femur or tibia to bring the knee joint back into a more physiologic alignment. This procedure moves the weight-bearing axis to the less damaged compartment. Recovery is prolonged and relief of symptoms often incomplete, but osteotomy may delay the need for total knee replacement for 5 to 10 years [49,50]. Successful treatment could allow a return to sport. The risks specific to this surgery depend on the technique and include nonunion at the osteotomy site, common peroneal nerve injury, pain from the proximal tibiofibular joint, and overcorrection or undercorrection of the deformity. Part of an ongoing debate within the orthopedic community concerns the relative merits of high tibial osteotomy compared with unicompartmental knee replacement in younger patients. Unicompartmental knee replacement requires a smaller surgical approach than for total knee replacement, leading to less blood loss and quicker rehabilitation. The range of knee motion after unicompartmental knee replacement is generally superior to that after total knee replacement. Finally, revision of a unicompartmental knee replacement to a total knee replacement is potentially more straightforward than revision of a total knee replacement [51]. The prerequisites for a unicompartmental knee replacement include stability of the joint, correctable varus deformity, fixed flexion deformity of less than 10 degrees, and minimal lateral compartment disease. Radiographic evidence of patellofemoral osteoarthritis is not necessarily a problem, provided patients do not have major anterior knee pain. Survivorship rates for implants are estimated at 93% and 90% at 15 and 20 years, respectively [52]. These rates are comparable to the best reported for total knee replacement and are an improvement on rates previously reported for unicompartmental knee replacement.
The relative merits of unicompartmental knee replacement over total knee replacement or proximal tibial osteotomy in young (< 60 years) active patients continue to be debated. Unicompartmental knee replacement has now become an accepted treatment for older patients with medial compartment arthritis. The results of unicompartmental knee replacement in lateral compartment disease have yet to be fully determined. Total knee replacements, with a quarter-century track record, have generally provided most patients with good pain relief. Whereas joint replacement surgery has been found in numerous studies to provide pain relief, it paradoxically may lead to increase of services as patients become more mobile [53].
Patients considered for patellofemoral replacement must be assessed for degenerative changes in the rest of the knee joint. Several types of patellofemoral arthroplasties are available, but the results have been variable, highlighting the need for careful selection of patients [54–56]. The most common problems are maltracking of the patella, excessive wear of the polyethylene implant, and disease progression in the rest of the knee joint. Severe chondromalacia may necessitate patellectomy (patella excision). Knee arthrodesis today is generally reserved for patients in whom knee replacement surgery fails. Other less commonly used surgical options, such as synovectomy and small prostheses (to correct deformity), are also possible.
Potential Disease Complications
Progressive knee osteoarthritis may result in reduced mobility and the general systemic complications of immobility and deconditioning. Antalgic gait can result in contralateral hip disease (e.g., greater trochanteric bursitis). The risk of falls will be increased by decreased mobility at the knee. Complaints of chronic pain may result from the initial knee osteoarthritis if it is inadequately treated.
Potential Treatment Complications
Complications of anti-inflammatory medication and steroid injections are well known. Repeated steroid injections can lead to further cartilage destruction as well as to sepsis. Infection is a rare but possible result of joint injection or surgery. Cryotherapy or heat therapy can, of course, lead to frostbite or burns. Hyaluronic acid injections may result in localized transient pain or effusion.
Arthroscopy may damage the articular surface membrane, thus initiating damage to uninvolved cartilage. Excessive arthroscopic scraping has sometimes been associated with persistent pain. The possibility of infection and deep venous thrombosis and the small but real possibility of intraoperative mortality limit the use of surgery to a last-line option. One series of patients not taking anticoagulants experienced a 50% rate of deep venous thrombosis, 14.5% of which was proximal deep venous thrombosis [57], thus indicating the importance of anticoagulation, which reduces the risk to less than 5%. In any case, mechanical wear and prosthesis loosening, especially for cemented prostheses, often lead to the need for revision after a decade or so.