CASE 70
History: A 30-year-old man presents with fever and abdominal pain.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in the figure? (Choose all that apply.)
2. What clinical condition is a major predisposing factor to the development of splenic abscesses?
3. What is the most common source of septic emboli that can result in splenic abscesses?
4. What local condition is most commonly associated with the development of a splenic abscess?
ANSWERS
CASE 70
Splenic Abscess
1. A, B, and E
2. C
3. C
4. C
References
Kamaya A, Weinstein S, Desser TS. Multiple lesions of the spleen: differential diagnosis of cystic and solid lesions. Semin Ultrasound CT MRI. 2006;27:389–403.
Warshauer DM, Hall HL. Solitary splenic lesions. Semin Ultrasound CT MRI. 2006;27:370–388.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 218.
Comment
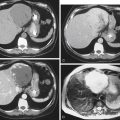
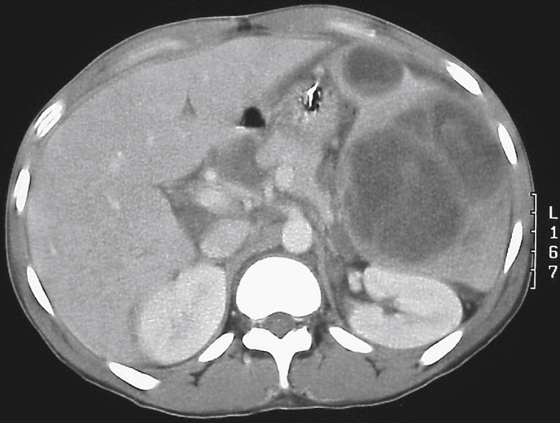
Splenic abscesses are being encountered more commonly as a result of better diagnostic studies, such as CT (see figure) and ultrasound, and the increased number of patients with immunosuppression (e.g., patients with AIDS, transplant recipients, and those undergoing chemotherapy). Splenic abscesses can develop in several ways, including as a result of metastatic infection from septic emboli (endocarditis), as a result of contiguous infection (pyelonephritis or pancreatitis), as a sequela of an infarct or trauma with secondary infection, and as a result of generalized immunosuppression with sepsis. A small fraction of splenic abscesses develop in the absence of any underlying condition. Most infectious organisms, such as staphylococci, streptococci, and Escherichia coli, are aerobic. There is often a high incidence of fungal abscesses, no doubt because many of these patients are immunosuppressed.
The most common finding on plain radiography is a left pleural effusion. CT is the best modality for detecting splenic abscesses, although they also may be demonstrated by ultrasound or even MRI. The problem with CT is that many other conditions have an appearance similar to that of an abscess, and from an imaging perspective it might be impossible to differentiate an epithelial or a posttraumatic splenic cyst from an abscess. Clinical history is as important to the radiologist as it is to the clinician. Those who do not understand this have a poor grasp of the role of imaging in patient care.
Abscesses are areas of low density caused by necrotic or infected tissue. Gas is rarely demonstrated but is pathognomonic of an abscess if present. A hematoma or an infarct can appear like an abscess, as would a neoplastic process, such as lymphoma. The wall of an abscess is usually thick and somewhat irregular, which can help to differentiate it from a splenic cyst. The rim of a splenic cyst enhances only when a well-defined capsule develops about the edge of the cyst, which occurs only later in the inflammatory process. Nuclear imaging may be helpful if there is concern about the nature of a splenic mass. Gallium scans and labeled white blood cell studies are active in areas of an abscess; however, lymphoma is also gallium positive. Labeled leukocyte studies always show splenic activity and can obscure an abscess.