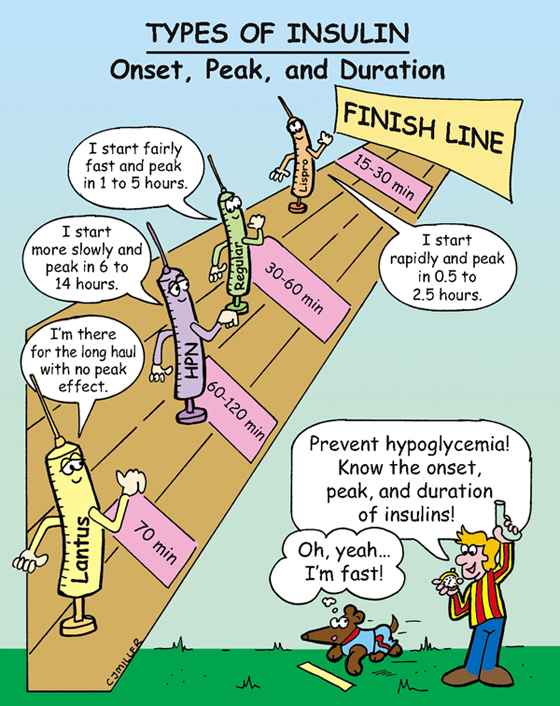
Types of Insulin
ACTIONS
NURSING IMPLICATIONS
1. U100 insulin is the most common concentration.
2. NPH is the only cloudy insulin; roll vial gently between palms to mix.
3. *Draw up clear (regular, lispro—short acting) before the cloudy (intermediate) insulin to prevent contaminating a short-acting insulin with a long-acting insulin.*
4. Inject subcutaneously; aspiration is not necessary.
5. Avoid massaging the site after injection.
6. ‡Rotate sites within anatomic area; the abdomen is preferred for more rapid, even absorption.‡
7. *Only NPH (Humulin) can be mixed with short-acting insulins.*
8. *Only the short-acting insulins may be administered intravenous (IV).*
9. *Hypoglycemia is the primary drawback in maintaining tight control of glucose.*
10. *Store unopened vials of insulin in the refrigerator; vial currently in use should be stored at room temperature for 1 month.*
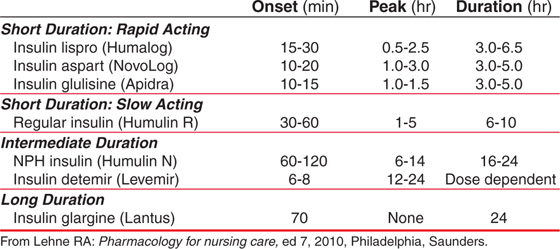
Sulfonylureas
• First generation—tolbutamide (Orinase), acetohexamide (Dymelor), chlorpropamide (Diabinese), tolazamide (Tolinase)
• Second generation—glipizide (Glucotrol), glyburide (Diabeta), glimepiride (Amaryl)
ACTIONS
Stimulates the beta cells of the pancreas to increase release of insulin. It also increases the sensitivity of peripheral insulin receptors, which increase insulin binding in the peripheral tissues. Second-generation medications act the same but are stronger.
USES
• Type 2 diabetes mellitus; may be used with other hypoglycemic conditions.
• Used as adjunct to diet and exercise programs to maintain glucose control.
CONTRAINDICATIONS AND PRECAUTIONS
• Not effective in patients with type 1 diabetes mellitus.
SIDE EFFECTS
NURSING IMPLICATIONS
1. ‡Instruct patient to take the drug 15 to 30 minutes before meals. Do not take medication and skip meals.‡
2. Self-monitor blood glucose (SMBG) levels three to five times daily.
3. Teach patient to maintain weight and dietary restrictions along with medication.
4. †Hypoglycemia (fatigue, hunger, cool moist skin, increased anxiety, dizziness, palpitations) should be treated immediately—take a fast-acting oral sugar (e.g., glucose tablets, orange juice).†
5. ‡If patient is not in the hospital and cannot swallow, emergency services (9-1-1) should be initiated.‡
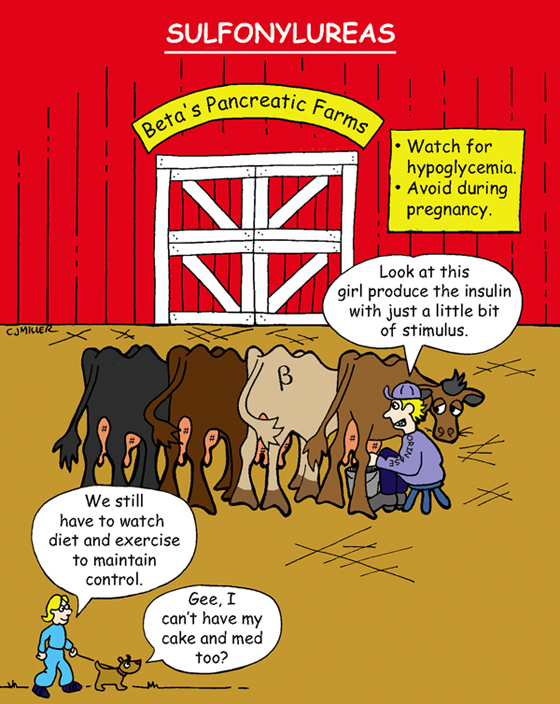
Metformin (Glucophage)
CLASSIFICATION
Oral hypoglycemic
ACTIONS
Inhibits glucose production in the liver, reduces glucose absorption in intestine, and sensitizes insulin receptors at sites in fat and skeletal muscle.
USES
• Lowers blood glucose in patients with type 2 diabetes.
• May be used for blood sugar control in patients with gestational diabetes.
CONTRAINDICATIONS
• Conditions that predispose a patient to lactic acidosis (e.g., liver disease, severe infections, hypoxemia, dehydration)
PRECAUTIONS
• Patients who consume large amounts of alcohol.
• Heart failure may predispose patient to lactic acidosis.
• Patients with renal failure.
SIDE EFFECTS
• **Decreased appetite, nausea, diarrhea**
• Decreases absorption of vitamin B12 and folic acid
NURSING IMPLICATIONS
1. *Monitor serum glucose and HbA1c.*
2. *Assess effectiveness of blood sugar control when used with other oral hypoglycemics (sulfonylureas).*
• ‡Take medication as scheduled (do not skip or add doses; do not stop taking medication).‡
• ‡Maintain dietary restrictions for glucose control.‡
4. ‡Teach patient the signs of lactic acidosis: hyperventilation, muscle aches, extreme fatigue.‡
5. ‡Encourage increase in vitamin B12 and folic acid in diet.‡
Corticosteroids
CLASSIFICATION
Adrenocorticosteroid, glucocorticoid
ACTIONS
Suppresses the inflammatory and immune systems by inhibiting synthesis of chemical mediators—prostaglandins, leukotrienes, and histamine. Decreases inflammation, which then reduces swelling, warmth, redness, and pain.
USES
• Addison disease; hormone replacement therapy, cancer therapy
PRECAUTIONS
• Pediatric patients, pregnancy, and breast-feeding
• Hypertension, heart failure, renal impairment
• Esophagitis, peptic ulcer disease (PUD), and diabetes
SIDE EFFECTS
• **Increased risk of new infection, mask development of infection, and delayed wound healing**
• Osteoporosis, **glucose intolerance (hyperglycemia),** †peptic ulcer, gastrointestinal (GI) bleeding†
• Muscle wasting, fluid and electrolyte disturbance, **Cushing syndrome**
NURSING IMPLICATIONS
1. *Monitor fluid balance and potassium and glucose levels.*
2. *Warn patient to take as prescribed and not to discontinue therapy suddenly.*
3. Assess for underlying infection and decreased wound healing.
4. *Daily doses need to increase during stress.*
5. Assess for Cushing symptoms.
6. Check stools for occult blood.
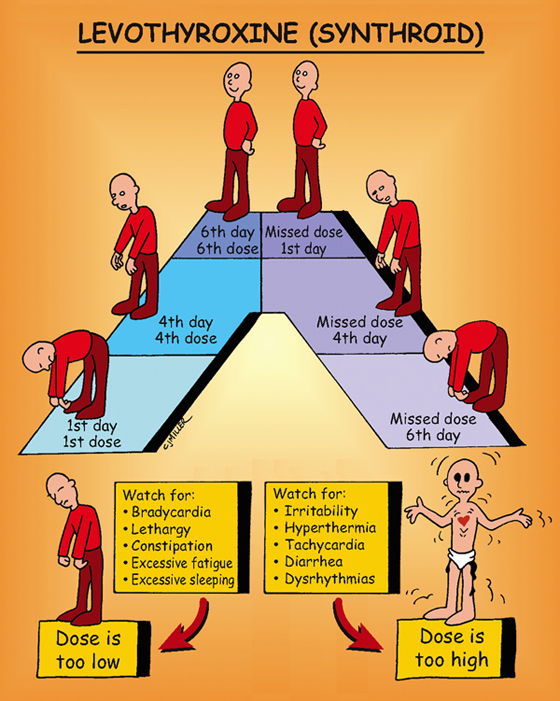
Levothyroxine (Synthroid)
CLASSIFICATION
Thyroid hormone
ACTIONS
Increases basal metabolic rate, enhances gluconeogenesis, stimulates protein synthesis.
USES
• Replacement in decreased or absent thyroid function
• Management of thyroid cancer
CONTRAINDICATIONS AND PRECAUTIONS
• Thyrotoxicosis and myocardial infarction without hypothyroidism
• Older adult patients; patients with impaired cardiac function, hypertension
SIDE EFFECTS
• **Overdose may cause thyrotoxicosis—tachycardia, increased blood pressure, angina, tremor, nervousness, insomnia, heat intolerance**
• Long-term use—osteoporosis and increased risk for atrial fibrillation
NURSING IMPLICATIONS
1. *Monitor for tachycardia and irregular pulse.*
2. ‡Teach patient to report any persistent symptoms of thyrotoxicosis.‡
3. ‡Replacement for hypothyroidism is life long. Do not discontinue.‡
4. ‡Instruct patient to have thyroid-stimulating hormone levels drawn periodically.‡
5. ‡Takes approximately 6 to 8 weeks for the full effects of the medication to be seen.‡
6. ‡Teach patient to take the medication in the morning, preferably 30 minutes before meals.‡