CHAPTER 7
Cervical Spinal Stenosis
Definition
Cervical spinal stenosis refers to pathologic narrowing of the spinal canal that can be either congenital or acquired. The congenital type is commonly due to short pedicles that produce an abnormally shallow central spinal canal [1]. Less frequently, congenital stenosis may be associated with developmental disorders, such as achondroplasia, Klippel-Feil syndrome, Morquio syndrome, and trisomy 21 (i.e., Down syndrome) [2,3]. The main contributing factors in development of the acquired type are the degenerative, hypertrophic, age-related changes that affect the intervertebral discs, facet joints, and uncovertebral joints as well as the ligamentum flavum (Fig. 7.1). On radiologic imaging, these degenerative changes are present in 25% to 50% of the population by the age of 50 years and in 75% to 85% by 65 years [4–6]. Some of the other factors that may contribute to pathologic narrowing of the spinal canal are degenerative spondylolisthesis, ossification of the posterior longitudinal ligament, and atlantoaxial subluxation as seen in rheumatoid arthritis; rarely, it may be secondary to such extradural pathologic processes as metastatic disease, abscess formation, and trauma [7]. Aside from age, other demographic factors do not contribute significantly to the development of cervical stenosis [8]. Whereas ossification of the posterior longitudinal ligament was once considered specific to the Japanese, it has since been well documented in Western and other Asian populations [9].
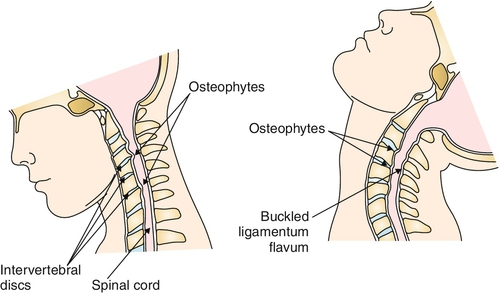
Symptomatic spinal cord compression, or cervical myelopathy, commonly occurs at the cervical levels C5-C7, given the relatively increased mobility of these segments and the subsequent development of degenerative “wear and tear.” Concomitant compression of the exiting cervical nerve roots is also typically observed in cervical spondylotic disease. Symptom production can occur by constant, mechanical compression of the neural elements or be of an intermittent, dynamic nature as seen with extremes of cervical flexion and extension. Chronic compression can lead to local cord ischemia with subsequent development of cervical myelopathy [10].
Symptoms
Symptomatic presentation of cervical spinal stenosis can differ from patient to patient, depending on the pathologic process, the anatomic structures, and the cervical levels involved. Intervertebral disc degeneration and zygapophyseal joint arthritis commonly are manifested with axial neck pain. Patients with cervical foraminal stenosis may complain of radicular arm pain as well as of paresthesias, dysesthesias, numbness, and weakness of the upper extremity. On the other hand, patients with cervical central canal stenosis can present with myelopathic symptoms of the upper and lower extremities, neurogenic bladder or bowel, sexual dysfunction, and unsteady and stiff-legged gait as well as weakness, paresthesias, or numbness of the lower extremities. Lower extremity pain is not known to be a clinical symptom unless concomitant lumbar spinal disease is present.
Physical Examination
Physical examination findings of the patient with cervical stenosis should be consistent with upper or lower motor neuron signs, depending on the spinal level involved. Lower motor neuron findings are more commonly seen in the upper extremities; these include muscle atrophy, diminished sensation, decreased reflexes, diminished muscle tone, and weakness. Upper extremity myelopathic findings, such as hyperactive reflexes, increased tone, and present Hoffmann sign, can also be observed in cases of upper and mid cervical spinal cord involvement. A Spurling sign (radicular pain on axial loading of an extended head rotated toward the involved extremity) can also be present. A well-documented feature of cervical spondylotic myelopathy is so-called myelopathy hand, characterized by wasting of intrinsic and extrinsic hand muscles, loss of power of adduction and extension of the ulnar two or three digits, and inability to rapidly grip and release. Myelopathy hand is demonstrated by the hand grip-and-release test, which measures alternating closed-fist and full finger extension movements (normal result is 20 times in 10 seconds); the finger escape sign is tested with fingers fully extended and adducted, noting a tendency for ulnar digit spread [11].
Lower extremity examination is more consistent with upper motor neuron findings in the presence of cervical stenosis with myelopathy. Increased reflexes, Babinski sign, sustained or unsustained clonus, spasticity, weakness, decreased tactile and vibratory sensation, impaired proprioception, and neurogenic bowel or bladder can be seen. Lhermitte sign, an electric-like sensation that the patient reports going down the back when the neck is flexed (Fig. 7.2), can sometimes be elicited [12]. Refer to Chapter 1 for more detail.

Functional Limitations
The functional limitations depend on the extent of neurologic involvement. A person with mild symptoms can still be completely independent with activities of daily living, mobility, household chores, and work duties. In some cases, pain and weakness can produce various degrees of disability in self-care, such as grooming, bathing, and dressing, as well as in more physically demanding functions, especially in the community setting, such as lifting, carrying, and ambulation. Bowel and bladder incontinence as well as abnormalities of mood and sleep can further lead to social isolation and an increased level of actual and self-perceived disability. In extreme cases, paraplegia and quadriplegia can limit nearly all functional activities.
Diagnostic Studies
Facet and uncovertebral joint arthropathy, loss of intervertebral disc space, neuroforaminal narrowing, and presence of spondylolisthesis can be evaluated with cervical spine radiographs; if dynamic instability is suspected, flexion-extension views are advised. Presence of osseous and soft tissue disease as well as the extent of nerve root and spinal cord compression can be assessed by magnetic resonance imaging (MRI) (Fig. 7.3). Cervical myelography can provide additional information on the behavior of neural elements during flexion and extension. An upright dynamic MRI study may be able to provide the same information on the behavior of neural elements with less procedural invasiveness [13] (Fig. 7.4). Somatosensory evoked potentials can confirm the presence of myelopathy, and electromyography can confirm peripheral nerve root involvement [14].



Several radiologic criteria exist to define what constitutes significant stenosis of the cervical spine. The normal anterior-posterior dimension of the spinal canal at C3 through C7 is 16 to 18 mm [15]. Neck flexion reduces canal diameter by 2 to 3 mm, whereas extension may decrease it up to 3.5 mm at 45 degrees because of ligamentum flavum infolding [16,17]. According to some sources, an absolute cervical spinal stenosis is present when the sagittal spinal canal diameter is less than 10 mm, and relative spinal stenosis is present when this measurement is 10 to 13 mm [18,19]. A Torg ratio of less than 0.8, which is measured by dividing the sagittal diameter of the spinal canal by the sagittal diameter of the respective vertebral body, has been used to predict the presence of significant spinal stenosis and tries to eliminate any inherent radiographic measurement errors [20]. A more widely accepted approach in evaluating the extent of stenotic pathologic changes is through the use of MRI, which permits the functional capacity of the surrounding subarachnoid space and the state of the spinal cord itself to be more definitively assessed. Several studies have demonstrated a poor correlation between Torg ratio and extent of stenosis identified on MRI [21].
Diffusion-weighted sequences, in particular a technique known as diffusion tensor imaging, allow the visualization of specific nerve tract bundles and may detect early damage to the myelin sheath. Although its utility in imaging the spinal cord is currently limited, diffusion tensor imaging has demonstrated enhanced sensitivity for detection of early cervical spondylotic myelopathy and intramedullary lesions [22,23]. The presence of intramedullary signal abnormalities warrants further investigation and a more aggressive treatment approach (see Fig. 7.3). Computed tomographic myelography continues to offer some advantages over MRI, including superior spatial resolution, ability to distinguish bone from soft tissue intrusion into the cervical foramina, and dynamic visualization of the flow of contrast material [24].
Treatment
Initial
Conservative treatment is generally undertaken in the absence of clinical evidence of cervical myelopathy. If cervical myelopathy is suspected or clearly evident, the patient must be immediately referred for an evaluation by a spine surgical specialist. When a patient is symptomatic with pain but does not have myelopathic symptoms, relative decrease in physical activity for no longer than 2 or 3 days is initially recommended. For severe cervical or radicular pain, a soft neck collar can be prescribed for a few days with subsequent self-weaning by alternating periods of collar removal [25].
Self-application of ice or heat for cervical pain and transcutaneous electrical nerve stimulation for radicular symptoms can be of benefit to some patients.
Initial analgesics of choice are acetaminophen and nonsteroidal anti-inflammatory drugs, which may show some effect in cervical as well as in radicular pain when they are taken at regular intervals. More than one family of nonsteroidals should be tried before they are deemed to be ineffective. A short course of opioids and muscle relaxants may benefit those patients with severe pain and strong contraindications to the use of acetaminophen and nonsteroidal anti-inflammatory drugs. For recalcitrant, functionally limiting radicular symptoms, a 7- to 10-day tapering course of oral steroids is recommended. Persistent radicular pain can be treated with neuropathic pain medications, such as gabapentin, pregabalin, tricyclic antidepressants, duloxetine, and others [26].
Education of the patient about the nature of cervical stenosis, its worrisome signs and symptoms (e.g., progressive difficulties with gait, urinary retention or incontinence), injury prevention, and the importance of staying active is of paramount importance. In older patients, fall prevention and fall precautions should be immediately addressed to prevent catastrophic neurologic consequences. In individuals with MRI evidence of severe cervical stenosis, certain physical activities, such as horseback or motorcycle riding, climbing ladders, and participation in contact sports, should be strongly discouraged. Patients should also be advised to avoid the extremes of repetitive cervical extension and flexion, as in swimming the breast stroke, painting a ceiling, or performing legs overhead backward stretching.
Rehabilitation
Physical and occupational therapy should focus on keeping patients as active as possible while educating them about activities that might place them at risk for further injury. Continued physical activity, such as walking and the use of a stationary bicycle, is recommended to prevent overall muscle and aerobic deconditioning. Gentle cervical traction may also be tried in the absence of severe stenosis or myelopathic findings. With passing of the acute phase, a program consisting of stretching and isometric neck exercises should be undertaken. Once the pain-free range of motion is achieved, isotonic neck strengthening is initiated [27]. Eventually, patients should be graduated to a home exercise program.
Work site evaluation and institution of certain job restrictions are recommended to prevent repetitive hyperextension or hyperflexion activities. These might include adjustment of computer monitor height, recommendation for a phone headset, and restriction of duties requiring activities above eye level. The use of bifocals should also be addressed because these require frequent head positional changes.
Depression and anxiety can lead to symptom magnification and should be addressed by a mental health care provider. Cognitive-behavioral therapy, biofeedback, self-hypnosis, and relaxation techniques must always be considered part of the comprehensive pain management treatment.
Procedures
A trial of interlaminar or transforaminal epidural steroid injections is advocated for acute or subacute radicular symptoms of severe intensity unresponsive to more conservative measures. Care should be taken to avoid the introduction of a spinal needle at the level of stenosis when an interlaminar approach is used. Transforaminal epidural steroid injections should be performed by a well-trained practitioner with the use of digital subtraction angiography and with preference toward nonparticulate steroids (e.g., dexamethasone) to avoid catastrophic complications. Patients without significant central spinal canal compromise and who continue to suffer with chronic severe radicular symptoms, unresponsive to conservative approaches, may be candidates for a spinal cord stimulator trial and implantation.
Arthritic cervical facet joints, which are innervated by medial branch nerves, can be another source of pain. Intra-articular steroid injections can provide up to several months of significant pain relief. If these fail to provide significant analgesic effect, diagnostic medial branch nerve blocks can be performed; if results are found to be positive, radiofrequency nerve ablation should follow.
Surgery
Immediate surgical intervention should be sought with symptoms of progressive weakness, bladder or bowel incontinence, unsteady gait, and upper motor neuron findings. Decompressive single-level or multilevel laminectomy, laminoplasty, discectomy, foraminotomy, and cervical fusion by use of bone graft or instrumentation are the common surgical procedures. Referral to a surgical specialist should be considered for intractable radicular symptoms [28,29].
Various classification systems have been used to grade the severity of spondylotic myelopathy and to guide the decision for surgery. The Nurick scale, used more frequently in a research setting, is based exclusively on ambulatory function [30]. The Japanese Orthopaedic Association (JOA) classification system and its modified versions evaluate additional variables, including upper extremity function and manual dexterity, sensory changes of the trunk and extremities, and bladder function [31]. Operative management is typically recommended for a JOA score of less than 13 with clinical symptoms and evidence of spinal cord compression on imaging [32].
Potential Disease Complications
If it is left untreated, progressive pressure on the exiting cervical nerve roots and the spinal cord may lead to worsening weakness, loss of sensation, dysfunction of the bladder and bowel, or tetraplegia.
The natural course of symptomatic cervical spondylotic myelopathy, when it is treated conservatively, demonstrates slow gradual decline in many patients, with periods of long quiescence or mild clinical improvement in some [33].
Potential Treatment Complications
Application of aggressive or improper physical or occupational therapy treatments can lead to further injury to the already compromised spinal cord and the exiting nerve roots. Cervical traction may promote signs and symptoms of myelopathy and radiculopathy. Atrophy of cervical musculature can occur with prolonged use of a cervical collar [34]. Aggressive cervical manual technique can cause vertebral artery dissection and severe neurologic sequelae.
Nonsteroidal anti-inflammatory medications carry well-known side effects of gastrointestinal irritation, bleeding, edema, and nephropathy. These medications are to be used cautiously or avoided in patients with a past history of peptic ulcer disease or with decreased renal function. A proton pump inhibitor or misoprostol should be considered for ulcer prophylaxis in individuals at high risk. All of the neuropathic pain medications carry significant side effects; gabapentin and pregabalin possess the best tolerance. The most common complaints are sedation, dizziness, and poor ambulatory balance. Continued use of opioids can lead to physiologic dependence, tolerance, sedation, constipation, and rarely addiction. Objective evidence of improved function and decreased level of pain is required for their continued use.
Interlaminar epidural steroid injections carry a small risk of dural puncture and subsequent development of a post–dural puncture headache. In most patients, these headaches are self-limited and respond well to bed rest, hydration, and caffeine. Improper placement of the needle tip and intravascular injection of particulate steroids with the transforaminal epidural approach can lead to spinal cord injury, stroke, and brain stem infarct. All interventions, percutaneous and surgical, carry a rare risk of spinal infection, compressive hematoma, and nerve and spinal cord injury.







