Procedure 7 Acute Repair of Zone 1 Flexor Digitorum Profundus Avulsion
![]() See Video 4: Acute Repair of Zone 1 Flexor Digitorum Profundus Avulsion
See Video 4: Acute Repair of Zone 1 Flexor Digitorum Profundus Avulsion
Indications
 Loss of flexion of the distal interphalangeal (DIP) joint may occur owing to avulsion of the flexor digitorum profundus (FDP) from its insertion into the distal phalanx.
Loss of flexion of the distal interphalangeal (DIP) joint may occur owing to avulsion of the flexor digitorum profundus (FDP) from its insertion into the distal phalanx.
 Typical etiology is forced extension of the flexed finger, typically when tackling an opponent in football, which is often called “jersey finger.”
Typical etiology is forced extension of the flexed finger, typically when tackling an opponent in football, which is often called “jersey finger.”
 Reattachment is possible if presented 10 to 14 days after injury, or longer if FDP is not retracted proximally because of the restraint provided by the intact vincula.
Reattachment is possible if presented 10 to 14 days after injury, or longer if FDP is not retracted proximally because of the restraint provided by the intact vincula.
 If there is a late presentation, the potential need for tendon grafting or other procedures such as DIP fusion or tenodesis must be discussed.
If there is a late presentation, the potential need for tendon grafting or other procedures such as DIP fusion or tenodesis must be discussed.
 If tendon grafting is contemplated for late presentation, the patient must have a supple DIP joint. In addition, patient expectations must be appropriate.
If tendon grafting is contemplated for late presentation, the patient must have a supple DIP joint. In addition, patient expectations must be appropriate.
Examination/Imaging
Clinical Examination
Imaging
 Standard anteroposterior and lateral radiographs are necessary.
Standard anteroposterior and lateral radiographs are necessary.
 Lateral radiographs may demonstrate an avulsed bony fragment at the DIP or proximally in the finger or palm corresponding to the proximal retraction of the FDP tendon to which the bone fragment is attached (Fig. 7-2).
Lateral radiographs may demonstrate an avulsed bony fragment at the DIP or proximally in the finger or palm corresponding to the proximal retraction of the FDP tendon to which the bone fragment is attached (Fig. 7-2).
 Ultrasound may be beneficial in confirming the injury, identifying the location of the retracted tendon preoperatively, and aiding in surgical planning, particularly in late presentations.
Ultrasound may be beneficial in confirming the injury, identifying the location of the retracted tendon preoperatively, and aiding in surgical planning, particularly in late presentations.
Surgical Anatomy
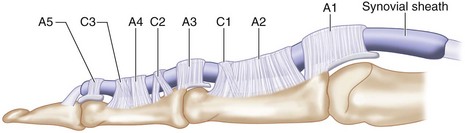
 Flexor zone 1 is distal to flexor digitorum superficialis (FDS) insertion over the middle third of the middle phalanx and contains only the FDP, C3, and A5 pulleys (Fig. 7-3).
Flexor zone 1 is distal to flexor digitorum superficialis (FDS) insertion over the middle third of the middle phalanx and contains only the FDP, C3, and A5 pulleys (Fig. 7-3).
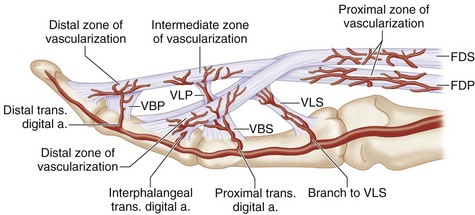
 Blood supply to the distal FDP is from the vinculum longus profundus (VLP), vinculum brevis profundus (VBP), and distal phalanx at its bony insertion (Fig. 7-4).
Blood supply to the distal FDP is from the vinculum longus profundus (VLP), vinculum brevis profundus (VBP), and distal phalanx at its bony insertion (Fig. 7-4).
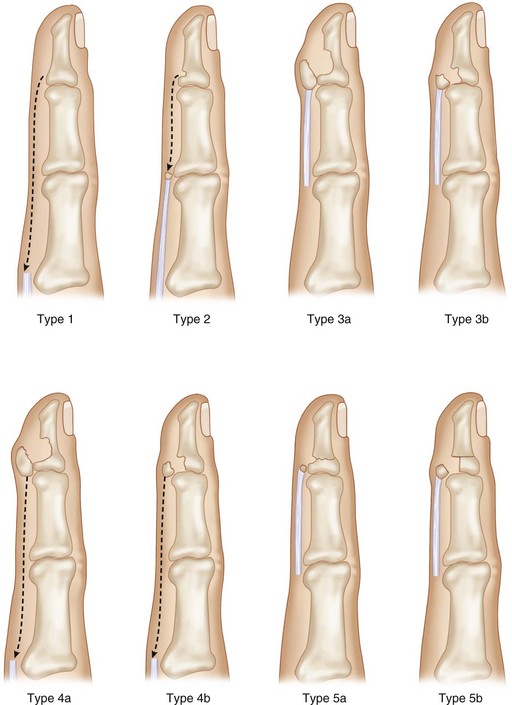
 Avulsed tendon can retract proximally in three patterns as defined by Leddy and Packer (1977). Additional types 4 and 5 have been described (Fig. 7-5).
Avulsed tendon can retract proximally in three patterns as defined by Leddy and Packer (1977). Additional types 4 and 5 have been described (Fig. 7-5).
 In most cases, the tendon can be retrieved from the above locations, passed through the pulley system, and reattached to the distal phalanx via pullout button or bone anchor.
In most cases, the tendon can be retrieved from the above locations, passed through the pulley system, and reattached to the distal phalanx via pullout button or bone anchor.
 With late presentation of greater than 4 weeks, the myostatic contracture of the avulsed tendon may preclude distal reconstruction, obligating a tendon graft.
With late presentation of greater than 4 weeks, the myostatic contracture of the avulsed tendon may preclude distal reconstruction, obligating a tendon graft.
Exposures
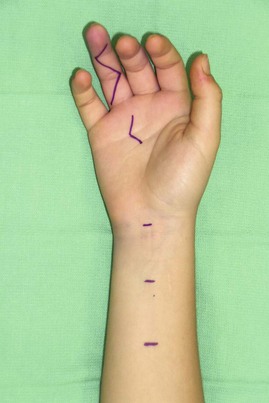
 A zigzag Bruner incision will provide the best exposure of the finger. The incision can be extended proximally as needed to retrieve the tendon or provide exposure for repair (Fig. 7-6).
A zigzag Bruner incision will provide the best exposure of the finger. The incision can be extended proximally as needed to retrieve the tendon or provide exposure for repair (Fig. 7-6).
 A palmar incision at the level of the A1 can help in retrieving the tendon to be passed through fibrous flexor sheath to zone 1.
A palmar incision at the level of the A1 can help in retrieving the tendon to be passed through fibrous flexor sheath to zone 1.
Procedure
Step 1
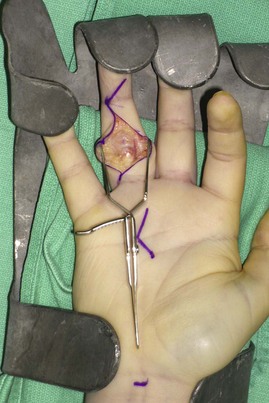
 Exploration of the finger with a zigzag incision is used to identify the proximal tendon at one of several classic locations—at A4, between A2 and A4 pulleys, or at A1 (Fig. 7-7).
Exploration of the finger with a zigzag incision is used to identify the proximal tendon at one of several classic locations—at A4, between A2 and A4 pulleys, or at A1 (Fig. 7-7).
 The A2 pulley is partially opened to retrieve the proximal tendon (Fig. 7-8).
The A2 pulley is partially opened to retrieve the proximal tendon (Fig. 7-8).
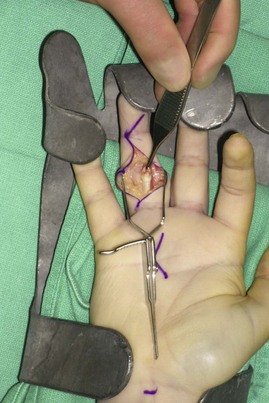
 At the distal tendon insertion, thin atrophic tendon remains that is not suitable for repair (Fig. 7-9).
At the distal tendon insertion, thin atrophic tendon remains that is not suitable for repair (Fig. 7-9).
 Excursion of the proximal tendon is tested and found to be inadequate for tension-free repair (Fig. 7-10).
Excursion of the proximal tendon is tested and found to be inadequate for tension-free repair (Fig. 7-10).
 The FDP is pulled proximally over the palm and dissected free from the FDS. Scar adhesion is released, which often develops if treatment is delayed.
The FDP is pulled proximally over the palm and dissected free from the FDS. Scar adhesion is released, which often develops if treatment is delayed.
 This provides additional mobility of tendon to allow primary repair (Fig. 7-11).
This provides additional mobility of tendon to allow primary repair (Fig. 7-11).
 A small feeding catheter is gently threaded through the A2 pulley into the palmar incision (Fig. 7-12). The feeding catheter is sutured to the proximal profundus tendon using a horizontal mattress suture, and the tendon is gently threaded through the pulley system into the distal incision (Fig. 7-13).
A small feeding catheter is gently threaded through the A2 pulley into the palmar incision (Fig. 7-12). The feeding catheter is sutured to the proximal profundus tendon using a horizontal mattress suture, and the tendon is gently threaded through the pulley system into the distal incision (Fig. 7-13).
 The wrist is flexed to decrease the tension on the profundus tendon so that more of the tendon can be retrieved into the distal incision. A needle is inserted to hold the tendon in place (Fig. 7-14).
The wrist is flexed to decrease the tension on the profundus tendon so that more of the tendon can be retrieved into the distal incision. A needle is inserted to hold the tendon in place (Fig. 7-14).
Step 2
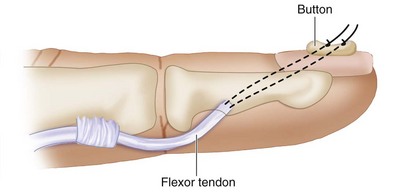
 In avulsion injuries, direct tenorrhaphy is not possible, and treatment consists of reattaching the proximal tendon to the bone via pullout suture over a button (Fig. 7-15).
In avulsion injuries, direct tenorrhaphy is not possible, and treatment consists of reattaching the proximal tendon to the bone via pullout suture over a button (Fig. 7-15).
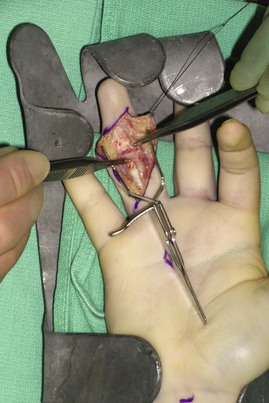
 The distal tendon remnant and scar is resected to expose the volar base of the distal phalanx.
The distal tendon remnant and scar is resected to expose the volar base of the distal phalanx.
 The volar proximal aspect of the distal phalanx is gently débrided until cancellous bone is encountered. A bone tunnel is not necessary (Fig. 7-16).
The volar proximal aspect of the distal phalanx is gently débrided until cancellous bone is encountered. A bone tunnel is not necessary (Fig. 7-16).
 Zigzag 3-0 Prolene suture is passed through the distal end of the tendon (Fig. 7-17).
Zigzag 3-0 Prolene suture is passed through the distal end of the tendon (Fig. 7-17).
 Keith needle holes are drilled obliquely through the base of the distal phalanx just lateral or distal to the bone through to the dorsum of the finger while avoiding the germinal matrix of the nail.
Keith needle holes are drilled obliquely through the base of the distal phalanx just lateral or distal to the bone through to the dorsum of the finger while avoiding the germinal matrix of the nail.
 The suture ends holding the distal aspect of the FDP tendon are then passed thought the Keith needle holes to be withdrawn over the nail bed.
The suture ends holding the distal aspect of the FDP tendon are then passed thought the Keith needle holes to be withdrawn over the nail bed.
 The sutures are then secured in place with a bolster, or button, on the dorsal aspect of the finger (Fig. 7-18).
The sutures are then secured in place with a bolster, or button, on the dorsal aspect of the finger (Fig. 7-18).
Step 2 Pearls
• Prolene sutures are used because they can slide out easily upon healing of the tendon to the bone, which takes about 6 weeks.
• One must be careful when placing the Keith needles through the nail to avoid proximal penetration of the germinal matrix, which may cause nail deformity.
• When tying down the Prolene suture over the nail, the surgeon must observe the tendon sitting securely within the bone trough at the distal phalanx.
• The elevated periosteum can be sutured to the end of the tendon using 4-0 Ethibond braided suture to provide additional support.
Postoperative Care and Expected Outcomes
 The patient is placed in a dorsal blocking splint with the wrist flexed at 60 degrees and the MCP joints flexed at 90 degrees to take tension off the tendon repair site (Fig. 7-19).
The patient is placed in a dorsal blocking splint with the wrist flexed at 60 degrees and the MCP joints flexed at 90 degrees to take tension off the tendon repair site (Fig. 7-19).
 The hand is splinted in this posture for about 4 weeks, and passive flexion-extension exercises are initiated for the DIP joint within 1 week.
The hand is splinted in this posture for about 4 weeks, and passive flexion-extension exercises are initiated for the DIP joint within 1 week.
 After 4 weeks, the splint is gradually extended to provide more tension at the suture line, and the patient is started on gentle active flexion exercises.
After 4 weeks, the splint is gradually extended to provide more tension at the suture line, and the patient is started on gentle active flexion exercises.
 The button and the Prolene suture are removed at 8 weeks after surgery in the clinic.
The button and the Prolene suture are removed at 8 weeks after surgery in the clinic.
 Three months after the tendon repair, the patient begins strengthening exercises and continues scar massages to achieve better excursion of the flexor tendon. (Fig. 7-20 demonstrates the early postoperative result of the patient shown in Fig. 7-1.)
Three months after the tendon repair, the patient begins strengthening exercises and continues scar massages to achieve better excursion of the flexor tendon. (Fig. 7-20 demonstrates the early postoperative result of the patient shown in Fig. 7-1.)
Pitfalls
Tendon rupture is a distinct possibility if the tendon does not heal to the bone. One should immediately explore the tendon system and place a tendon graft when a rupture is encountered because the tendon sheath will collapse quickly when the sheath is empty. Early exploration is much easier because the tendon sheath is still open, and retrieval and excision of the ruptured tendon within the sheath are relatively easy. However, if the exploration is delayed, the ruptured tendon may be adherent to the pulley system and the tendon sheath may contract, which makes primary tendon grafting difficult.