Procedure 69 Vascularized Bone Grafting for Scaphoid Nonunion
![]() See Video 51: Pedicled Vascularized Bone Transfer for Scaphoid Nonunion
See Video 51: Pedicled Vascularized Bone Transfer for Scaphoid Nonunion
Indications
 Scaphoid fracture nonunions are seen that have developed avascular necrosis (AVN).
Scaphoid fracture nonunions are seen that have developed avascular necrosis (AVN).
 Vascularized bone grafting is contraindicated in fracture nonunions associated with significant degenerative changes in the radioscaphoid or midcarpal joint. These wrists require a salvage procedure.
Vascularized bone grafting is contraindicated in fracture nonunions associated with significant degenerative changes in the radioscaphoid or midcarpal joint. These wrists require a salvage procedure.
 A scaphoid nonunion humpback deformity cannot be corrected unless a structural graft is used.
A scaphoid nonunion humpback deformity cannot be corrected unless a structural graft is used.
Examination/Imaging
Clinical Examination
 General dorsoradial edema and focal snuffbox tenderness are highly suggestive of a scaphoid fracture.
General dorsoradial edema and focal snuffbox tenderness are highly suggestive of a scaphoid fracture.
 The distal pole of the scaphoid may also be tender to palpation, and axial compression of the thumb may reproduce the pain.
The distal pole of the scaphoid may also be tender to palpation, and axial compression of the thumb may reproduce the pain.
 Decreased wrist motion and grip strength are common findings in patients with a scaphoid nonunion.
Decreased wrist motion and grip strength are common findings in patients with a scaphoid nonunion.
Imaging
 Wrist radiographs including scaphoid views should be obtained to evaluate the overall fracture pattern, carpal alignment, and degree of radiocarpal and midcarpal arthritis. Chronic scaphoid nonunions display a characteristic pattern of wrist arthritis and carpal instability—scaphoid nonunion advanced collapse (SNAC), as described by Watson and Ballet. The hallmark of AVN on radiographs is increased bone density, fragmentation, and collapse (Fig. 69-1).
Wrist radiographs including scaphoid views should be obtained to evaluate the overall fracture pattern, carpal alignment, and degree of radiocarpal and midcarpal arthritis. Chronic scaphoid nonunions display a characteristic pattern of wrist arthritis and carpal instability—scaphoid nonunion advanced collapse (SNAC), as described by Watson and Ballet. The hallmark of AVN on radiographs is increased bone density, fragmentation, and collapse (Fig. 69-1).
 A thin-cut computed tomography (CT) scan with reconstructions carefully aligned in the axis of the scaphoid is helpful to elucidate scaphoid angular deformity (as measured by intrascaphoid angles), translation, comminution, and degenerative changes. This study best quantifies the deformity and necessary reconstruction.
A thin-cut computed tomography (CT) scan with reconstructions carefully aligned in the axis of the scaphoid is helpful to elucidate scaphoid angular deformity (as measured by intrascaphoid angles), translation, comminution, and degenerative changes. This study best quantifies the deformity and necessary reconstruction.
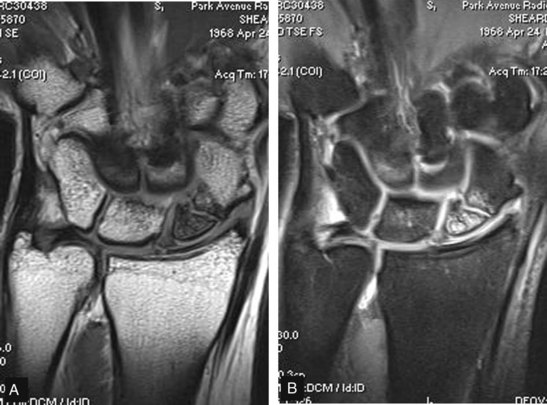
 Magnetic resonance imaging (MRI) is the only noninvasive study able to assess vascularity of the scaphoid and identify AVN (Fig. 69-2). An MRI should be obtained in every patient for whom there is a concern about the viability of the proximal pole. Contrast-enhanced imaging has a sensitivity of 66%, a specificity of 88%, and an accuracy of 83%.
Magnetic resonance imaging (MRI) is the only noninvasive study able to assess vascularity of the scaphoid and identify AVN (Fig. 69-2). An MRI should be obtained in every patient for whom there is a concern about the viability of the proximal pole. Contrast-enhanced imaging has a sensitivity of 66%, a specificity of 88%, and an accuracy of 83%.
Surgical Anatomy
 Eighty percent of the scaphoid surface is covered by articular cartilage, leaving limited space for vascular supply.
Eighty percent of the scaphoid surface is covered by articular cartilage, leaving limited space for vascular supply.
 A dorsal branch of the radial artery provides 70% to 80% of the blood supply.
A dorsal branch of the radial artery provides 70% to 80% of the blood supply.
 A second nutrient artery enters volarly and supplies only the distal pole.
A second nutrient artery enters volarly and supplies only the distal pole.
 There is no nutrient artery to the proximal pole; thus, it is susceptible to AVN when fractured.
There is no nutrient artery to the proximal pole; thus, it is susceptible to AVN when fractured.
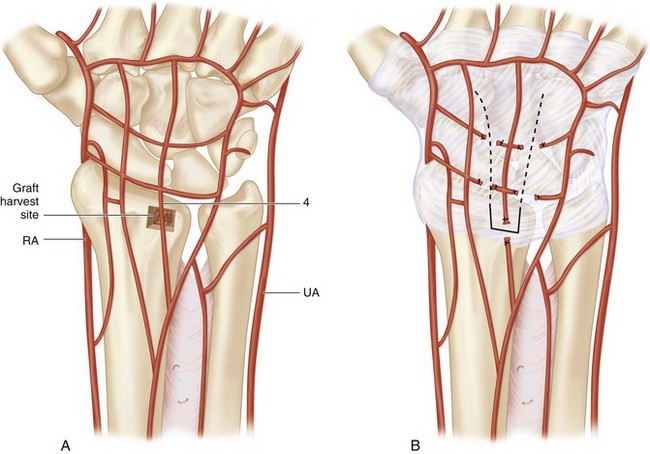
 Dorsal distal-radius vascularized bone grafts have been shown to be based on consistent vascular anatomy (Fig. 69-3A).
Dorsal distal-radius vascularized bone grafts have been shown to be based on consistent vascular anatomy (Fig. 69-3A).
 The pedicled graft described in this chapter is based on the artery of the fourth extensor compartment. The fourth extensor compartment artery is less than 1 mm in diameter and between 1 and 2 cm in length (see Fig. 69-3A and B).
The pedicled graft described in this chapter is based on the artery of the fourth extensor compartment. The fourth extensor compartment artery is less than 1 mm in diameter and between 1 and 2 cm in length (see Fig. 69-3A and B).
 Rotation of the graft on the capsular pedicle of only 10 to 30 degrees allows placement of the graft on the proximal scaphoid.
Rotation of the graft on the capsular pedicle of only 10 to 30 degrees allows placement of the graft on the proximal scaphoid.
Exposures
 Multiple vascularized grafts have been described. One of the more popular grafts is that based on the 1,2 intercompartmental supraretinacular artery (1,2 ICSRA) as described by Zaidemberg. We prefer to use a dorsal capsular distal-radius graft as described by Sotereanos and coworkers because it does not involve dissection of tiny vessels, is less technically demanding, and is more durable during flap rotation.
Multiple vascularized grafts have been described. One of the more popular grafts is that based on the 1,2 intercompartmental supraretinacular artery (1,2 ICSRA) as described by Zaidemberg. We prefer to use a dorsal capsular distal-radius graft as described by Sotereanos and coworkers because it does not involve dissection of tiny vessels, is less technically demanding, and is more durable during flap rotation.
 A 4-cm dorsal incision is made centered over the radiocarpal joint, ulnar to the Lister tubercle (Fig. 69-4).
A 4-cm dorsal incision is made centered over the radiocarpal joint, ulnar to the Lister tubercle (Fig. 69-4).
 The extensor retinaculum over the third and fourth dorsal compartments is released. The extensor pollicis longus (EPL) tendon is retracted radially and the extensor digitorum communis (EDC) tendons ulnarly, exposing the dorsal wrist capsule (Fig. 69-5).
The extensor retinaculum over the third and fourth dorsal compartments is released. The extensor pollicis longus (EPL) tendon is retracted radially and the extensor digitorum communis (EDC) tendons ulnarly, exposing the dorsal wrist capsule (Fig. 69-5).
 Carefully elevate the extensor sheaths off the capsule at the medial and lateral borders to increase exposure of the graft.
Carefully elevate the extensor sheaths off the capsule at the medial and lateral borders to increase exposure of the graft.
Procedure
Step 1: Cutting the Graft
 A capsular-based pedicle about 1.5 cm wide is outlined on the dorsal surface of the wrist capsule, narrowing down to a 1 × 1 cm distal-radius bone block (see Fig. 69-3B).
A capsular-based pedicle about 1.5 cm wide is outlined on the dorsal surface of the wrist capsule, narrowing down to a 1 × 1 cm distal-radius bone block (see Fig. 69-3B).
 The bone block is situated at the dorsal ridge of the distal radius, just ulnar to the Lister tubercle, and should be about 7 mm in depth.
The bone block is situated at the dorsal ridge of the distal radius, just ulnar to the Lister tubercle, and should be about 7 mm in depth.
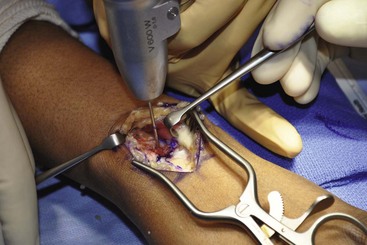
 The outline of the graft is “postage-stamped” using a 0.045-inch K-wire or similarly sized drill bit (Fig. 69-6).
The outline of the graft is “postage-stamped” using a 0.045-inch K-wire or similarly sized drill bit (Fig. 69-6).
Step 2: Elevate the Graft and Pedicle
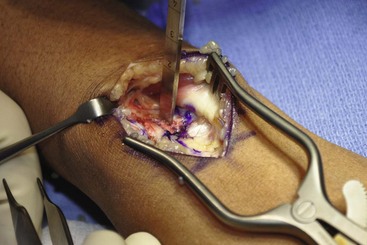
 The proximal, medial, and lateral edge osteotomies are completed with a straight osteotome (Fig. 69-7).
The proximal, medial, and lateral edge osteotomies are completed with a straight osteotome (Fig. 69-7).
 The graft is then carefully elevated with a curved osteotome, leaving 2 to 3 mm of distal radius cortex intact (Fig. 69-8).
The graft is then carefully elevated with a curved osteotome, leaving 2 to 3 mm of distal radius cortex intact (Fig. 69-8).
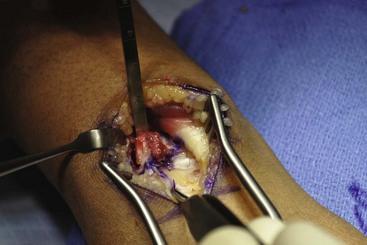
 Full-thickness dorsal capsular incisions are made, and the capsular flap is dissected away from the underlying tissues. The capsular attachment to the portion of the distal radius cortex left intact is carefully released with a scalpel. Be particularly mindful not to disturb the capsular attachment to the bone graft (Fig. 69-9).
Full-thickness dorsal capsular incisions are made, and the capsular flap is dissected away from the underlying tissues. The capsular attachment to the portion of the distal radius cortex left intact is carefully released with a scalpel. Be particularly mindful not to disturb the capsular attachment to the bone graft (Fig. 69-9).
Step 3: Scaphoid Preparation and Fixation
 After the flap has been elevated, the proximal half of scaphoid is visible.
After the flap has been elevated, the proximal half of scaphoid is visible.
 Identify the nonunion site and débride it of nonviable tissue with small curets and rongeurs, preserving bone stock and intact cartilage.
Identify the nonunion site and débride it of nonviable tissue with small curets and rongeurs, preserving bone stock and intact cartilage.
 If there is pseudoarthrosis with a cartilage shell primarily intact, it is not débrided but rather is left intact.
If there is pseudoarthrosis with a cartilage shell primarily intact, it is not débrided but rather is left intact.
 The scaphoid is then fixed using a headless screw as described in Procedure 68, although using an open technique (Fig. 69-10).
The scaphoid is then fixed using a headless screw as described in Procedure 68, although using an open technique (Fig. 69-10).
Step 4: Insetting the Graft
 The tourniquet is now deflated to check the viability of the graft. It may take several minutes to see punctate bleeding from the graft.
The tourniquet is now deflated to check the viability of the graft. It may take several minutes to see punctate bleeding from the graft.
 A trough, slightly smaller than the bone block, is created on the dorsal aspect of the scaphoid with a high-speed bur. The trough should be centered over the nonunion site and deep enough to hold the bone block securely (Fig. 69-11).
A trough, slightly smaller than the bone block, is created on the dorsal aspect of the scaphoid with a high-speed bur. The trough should be centered over the nonunion site and deep enough to hold the bone block securely (Fig. 69-11).
 The bone block, attached to its capsular pedicle, is then press-fit into the trough (Fig. 69-12).
The bone block, attached to its capsular pedicle, is then press-fit into the trough (Fig. 69-12).
 Final fluoroscopic posteroanterior and lateral images after the graft was inset are shown in Figure 69-13.
Final fluoroscopic posteroanterior and lateral images after the graft was inset are shown in Figure 69-13.
Step 5: Closure
 The wound is irrigated and closed in layers.
The wound is irrigated and closed in layers.
 The extensor retinaculum can be repaired; however, the EPL tendon should be placed radial to the Lister tubercle to minimize the risk for tendon irritation at the bone graft donor site.
The extensor retinaculum can be repaired; however, the EPL tendon should be placed radial to the Lister tubercle to minimize the risk for tendon irritation at the bone graft donor site.
 A volar and dorsal short-arm splint with a thumb component is applied in the operating room.
A volar and dorsal short-arm splint with a thumb component is applied in the operating room.
Postoperative Care and Expected Outcomes
 At the first office visit 2 weeks after surgery, the patient is fitted with a short-arm thumb spica cast to wear for an additional 4 weeks.
At the first office visit 2 weeks after surgery, the patient is fitted with a short-arm thumb spica cast to wear for an additional 4 weeks.
 When the cast is taken off, a removable Orthoplast thumb spica splint, constructed by an occupational therapist, is worn at all times until healing is confirmed by radiograph or CT scan.
When the cast is taken off, a removable Orthoplast thumb spica splint, constructed by an occupational therapist, is worn at all times until healing is confirmed by radiograph or CT scan.
Sotereanos DG, Darlis NA, Dailiana ZH, et al. A capsular-based vascularized distal radius graft for proximal pole scaphoid pseudarthrosis. J Hand Surg [Am]. 2006;31:580-587.
Sunagawa T, Bishop AT, Muramatsu K. Role of conventional and vascularized bone grafts in scaphoid nonunion with avascular necrosis: a canine experimental study. J Hand Surg [Am]. 2000;25:849-859.