CHAPTER 69
Iliotibial Band Syndrome
Venu Akuthota, MD; Sonja K. Stilp, MD; Paul Lento, MD; Peter Gonzalez, MD; Alison R. Putnam, DO
Definition
The iliotibial band (ITB) is a dense fascia on the lateral aspect of the knee and hip. Traditionally, the gluteus maximus and tensor fascia lata were thought to be the proximal origin of the ITB. Further anatomic dissections have demonstrated that the gluteus medius also has direct and indirect contributions to the ITB (Fig. 69.1) [1]. Proximal attachment includes the iliac tubercle or iliac crest [2,3]. In the distal thigh, the ITB attaches to the linea aspera and the upper edge of the lateral femoral epicondyle [3,4]. According to Terry [5], after passing over the lateral femoral epicondyle, it separates into two components. The iliotibial tract of the distal ITB attaches to Gerdy tubercle of the anterolateral proximal tibia. The iliopatellar band of the ITB has aponeurotic connections to the patella and the vastus lateralis [5]. Other distal attachments include the biceps femoris, the lateral patellar retinaculum, and the patellar tendon [5,6]. An anatomic pouch can be found underlying the posterior ITB at the level of the lateral femoral epicondyle [7]. Controversy exists as to whether this pouch is a bursa, a synovial extension of the knee joint, or degenerative tissue [7,8]. Others have reported that a highly innervated fat pad overlies the lateral femoral epicondyle [9].
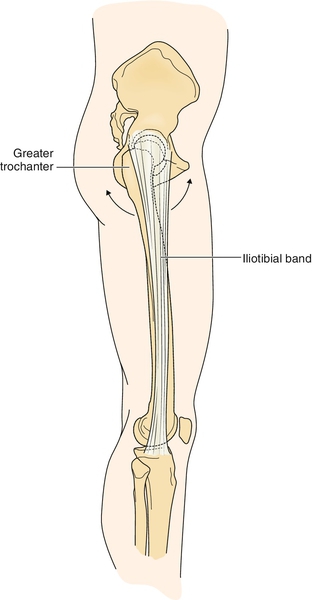
Iliotibial band syndrome (ITBS) or iliotibial band friction syndrome is an overuse injury typically referring to lateral knee pain as a result of impingement of the distal ITB over the lateral femoral epicondyle. Less commonly, ITBS may refer to hip pain associated with movement of the ITB across the greater trochanter. This chapter deals primarily with distal ITBS. The suspected pain generator in ITBS is as controversial as the anatomy around the lateral epicondyle. It has been postulated to be bursitis, synovitis, or irritation of the fat pad, posterior fibers of the ITB, or periosteum [3,6,9–12]. Although the anatomic pain generator may not be fully known, pain at the distal aspect of the ITB is thought to be caused by the fibers of the ITB passing over the lateral femoral epicondyle with knee flexion and extension [6,11].
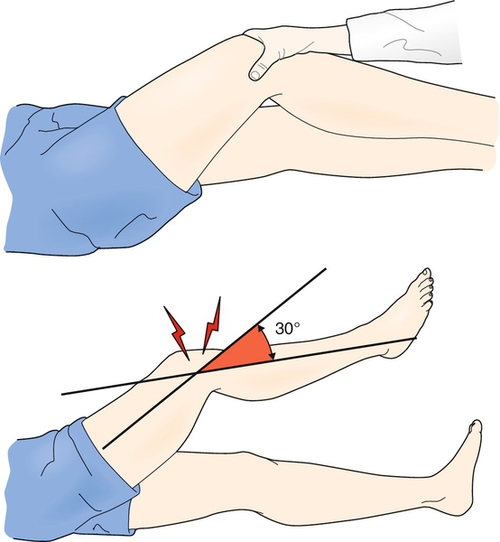
Friction has been implicated as the most important factor in ITBS [8,11]. Maximum friction occurs when the posterior fibers of the ITB pass over the lateral femoral epicondyle at 20 to 30 degrees of knee flexion, the putative “impingement zone.” [8] Repeated knee flexion and extension, particularly with increased running mileage per week, creates friction and has been shown to predispose an individual to lateral knee pain [8,11]. Friction has been shown to play a role in cycling activities as well. Cycling-induced ITBS is thought to result from the repetitive activity of cycling, as less time is spent in the impingement zone than during running activities [11]. Other authors have theorized that pain is due not only to friction but also to compression of the fat pad between the ITB and the lateral femoral epicondyle. The compression of the fat pad was found to be greatest at 30 degrees of flexion, similar to previous reports, and increased with internal rotation of the tibia during knee flexion [6,9].
Several factors may increase the risk for development of ITBS. Although it has not been extensively studied, poor neuromuscular control appears to be an important modifiable risk factor for ITBS. Weakness of hip abductors has been implicated in ITBS [6]. However, difference in strength of hip abduction was not found in a study of 10 runners with ITBS compared with controls [13]. Specifically, neuromuscular control is needed to attenuate the valgus–internal rotation vectors at the knee after heel strike. If appropriate control is not available, the ITB may have an abrupt increase in tension at its insertion site [10,14,15]. Increased hip adduction and knee internal rotation have been noted in female runners, suggesting increased ITB strain as a mechanism of injury [15]. Increased foot inversion, maximum knee flexion, and knee internal rotation were noted during an exhaustive run in recreational runners with history of ITBS [16]. Peak rearfoot eversion, knee internal rotation angle, and hip adduction angle were increased in 35 female runners with history of ITBS compared with matched controls [17]. Contradictory results were found in a study of 18 runners with ITBS compared with controls. Results indicated decreased hip adduction in those with ITBS, although they were found to have a lack of “coordination” defined as earlier hip flexion and knee flexion [18]. Hamill and colleagues [19] noted that the strain rate of the ITB during stance phase was increased in female runners who developed ITBS compared with healthy age-matched controls, and Miller and coworkers [16] noted increased ITB strain in recreational runners with history of ITBS. Strengthening of the gluteus medius and tensor fascia lata, decelerators of the valgus–internal rotation vectors at the knee, has been shown to reduce symptoms of ITBS [10,20]. Lack of dynamic flexibility, particularly of the ITB, has been implicated with ITB injury susceptibility [6,15,21,22]. No research study to date, though, has revealed a correlation between ITB tightness and ITB injury. Theoretically, however, tightness of the ITB or its constituent muscles increases impingement of the ITB on the lateral femoral epicondyle [8]. Other risk factors that may be attenuated with proper shoe wear or foot orthoses include excessive foot-ankle pronation and supination [6,16]. Training errors, such as rapid changes in training routine, hill training, striding, and excessive mileage, have also been highlighted as increasing the risk of ITBS [6,12]. Increased ground reaction force, as with running in old shoes, may also increase frictional forces at the knee and exacerbate symptoms [8]. Intrinsic or nonmodifiable factors, such as bone malalignment or a wide distal ITB, may contribute to the development of ITBS [22,23]. Finally, repeated direct trauma to the lateral knee, particularly with soccer goalies, appears to be injurious to the ITB impingement area [23].
Symptoms
Symptoms of ITBS occur typically at the lateral femoral epicondyle but may emanate from the distal attachment of the ITB at Gerdy tubercle on the tibia [6,12]. ITBS is the most common cause of lateral knee pain in runners [6]. Individuals present with sharp or burning lateral knee pain that is aggravated during repetitive activity. This pain may radiate up into the lateral thigh or down to Gerdy tubercle [24]. Runners often describe a specific, reproducible time when the symptoms commence [25]. Pain usually subsides after a run; however, in severe cases, persistent pain may cause restriction in distance [26,27]. Runners also note more pain with downhill running because of the increased time spent in the impingement zone [8]. Paradoxically, runners state that faster running and sprinting often do not produce pain. Fast running allows the athlete to spend more time in knee angles greater than 30 degrees [8]. Cyclists present with rhythmic, stabbing pain with pedaling. Specifically, they complain of pain at the end of the downstroke or the beginning of the upstroke. Bikers with improper saddle height and cleat position may experience greater symptoms [28,29].
ITBS symptoms may also occur as a lateral snapping hip. An external or lateral snapping hip occurs as the ITB rapidly passes anteriorly over the greater trochanter as the femur passes from extension to flexion [30]. Athletes, particularly dancers, sometimes experience an audible painful snap on landing in poor turnout (decreased external rotation at the hip) and with excessive anterior pelvic tilt [31].
Physical Examination
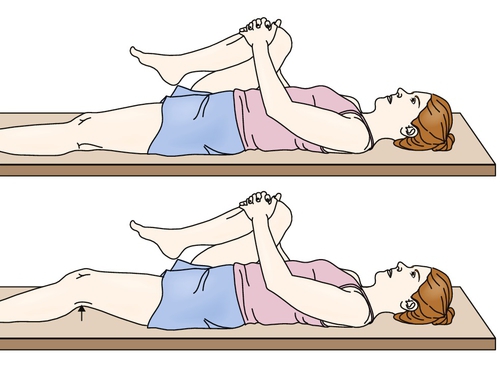
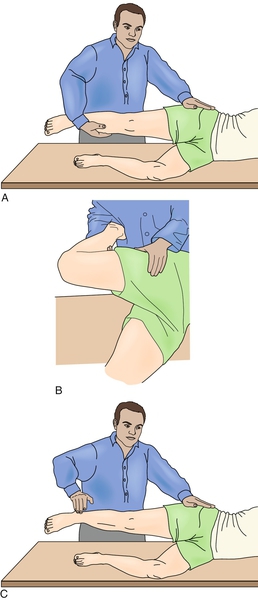
Physical examination begins with a screening examination of the joints above and below the site of injury. Hip girdle examination includes an assessment for joint range of motion, asymmetries [32], muscle strength (particularly hip abductors) [10], and lumbopelvic somatic dysfunctions [33]. The modified Thomas and Ober tests are used to assess flexibility of the ITB and related musculature at the hip and knee (Figs. 69.2 and 69.3) [6,12,34].
The knee examination includes palpation, patellar accessory motion [35], and the Noble compression test (Fig. 69.4) [8]. Knee tenderness is noted either at the lateral femoral epicondyle (above the lateral joint line) or at Gerdy tubercle. Palpatory examination should also include a thorough assessment for myofascial restrictions and trigger points along the lateral thigh musculature [25,26]. On rare occasion, ITB swelling and crepitus accompany tenderness. Pain can also be elicited by the Noble compression test [6]. Other conditions are effectively ruled out by performing a relevant physical examination.
The foot and ankle examination is particularly useful in the determination of gastrocnemius-soleus inflexibility, subtalar motion restrictions, and specific foot type (e.g., hindfoot varus). Finally, a biomechanical assessment of sports-specific activity can be done. Walkers and runners are observed for abnormalities such as excessive foot-ankle pronation, inability to attenuate shock at the knee, Trendelenburg frontal plane gait at the pelvis, and forward trunk lean [33,36]. Bicyclers are observed for proper foot placement on the pedal, saddle height, and knee angles with pedaling revolution [28,29]. Dancers can be observed performing rond de jambe or grand plié for proper turnout and pelvic stabilization [31].
The findings of the neurologic examination, including strength, sensation, and reflexes, are typically normal. Strength may be affected by disuse or guarding due to pain, particularly in the hip abductors and external rotators.
Functional Limitations
ITBS pain usually restricts athletes from their sports activity but does not typically cause limitations of daily activities. Yet, a vicious circle is set forth in which biomechanical deficits (e.g., gluteal weakness and ITB tightness) cause ITB tissue injury with resultant functional adaptations to avoid the pain of the tissue injury (e.g., external rotation of the hip) [32].
Diagnostic Studies
Imaging has a limited role in ITBS because it is usually a clinical diagnosis. Radiographs are rarely helpful [12]. Diagnostic ultrasonography has been used in some centers to confirm injuries [37]. Diagnostic ultrasound examination can measure ITB thickness for which normal values have been determined in uninjured subjects [38]. Dynamic sonography may also be helpful in identifying abnormal motion of the proximal ITB in diagnosis of external snapping hip syndrome [39]. When definitive diagnosis is needed or other diagnoses need to be excluded, magnetic resonance imaging has emerged as a potentially useful test. Magnetic resonance imaging may show a thickened ITB or high intensity on axial T2-weighted images [40].
Treatment
Initial
Acute phase treatment is akin to that of other musculoskeletal injuries. Relative rest consists of activity modification, particularly with restriction of those activities that exacerbate the pain symptoms [6,26]. In most instances, this does not mean a complete cessation of activity. The clinician needs to emphasize the positive aspects of relative rest and provide alternative training regimens. The ITB can be relatively off-loaded if an individual can keep his or her activity below the threshold of pain. Frequently, this can be achieved by simply decreasing intensity or training duration. Medications such as nonsteroidal anti-inflammatory drugs may help reduce pain and inflammation in the first few weeks of injury. If swelling is present, some authors advocate a local corticosteroid injection in the initial stages [25,26]. As well, modalities such as ice, ice massage, ultrasound, iontophoresis, and phonophoresis can be helpful in the early period to reduce early inflammation and pain [6,11,26]. It is critical early on to address the biomechanical cause of ITB injury [26].
Rehabilitation
Ultrasound, phonophoresis, iontophoresis, and electrical stimulation may also be used to reduce early inflammation and pain [26]. The subacute phase of rehabilitation addresses the biomechanical deficits found on physical examination. Typically, flexibility deficits are seen in the ITB, iliopsoas, quadriceps, and gastrocnemius-soleus [25,26]. Incorporation of flexibility and strengthening into the rehabilitation treatment is often recommended [6,13,26]. Proper stretching addresses all three planes and incorporates proximal and distal musculotendinous fibers.
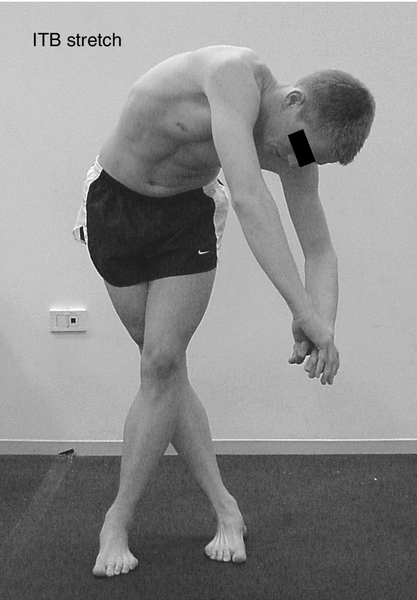
Fredericson and colleagues [21] studied the relative effectiveness of three commonly prescribed standing ITB stretches. The authors concluded that when overhead arm extension is added to the standing ITB stretch, the ITB length and average external adduction moments could be increased [21]. This stretch is performed standing with the symptomatic leg extended and adducted across the uninvolved leg. The subject laterally flexes the trunk toward the contralateral side and extends both arms overhead (Fig. 69.5). A study evaluated the effectiveness of the Ober test (see Fig. 69.3) and the modified Ober test in stretching the ITB and the most distal component, the iliotibial tract. The modified test is performed the same as the Ober test except the knee remains extended at 0 degrees. The investigators used ultrasonography to assess the soft tissue changes of the iliotibial tract and concluded that both tests are effective in the initial stages of stretching. However, the modified Ober test may afford a greater stretch of the iliotibial tract of the ITB when additional adduction of the hip is allowed [41]. In a cadaveric study, Falvey and colleagues [3] found limited ability to lengthen the ITB by the modified Ober test and by hip flexion, adduction, and external rotation with knee flexion (hip test) compared with control (straight-leg raise), although the hip test had significantly greater strain. In another limb of the same study, they found minimal change in length with isometric contraction of the tensor fascia lata, concluding that focus should be on stretching the muscle component of the ITB complex. Some muscle groups do not respond to stretch unless myofascial and joint restrictions are concomitantly addressed by experienced therapists or by self-administered techniques [25,26]. In a systematic review by Ellis and coworkers [11], one study of transverse friction massage was not found to be beneficial. Proper facilitation of hip girdle musculature can be achieved by addressing antagonistic tight structures, such as tight hip flexors or anterior hip capsule [34]. Subtalar mobilizations are often needed to prevent excessive valgus–internal rotation forces from transferring to the knee and ITB [36]. In conjunction with a flexibility and joint mobilization program, strengthening of weak or inhibited muscles can be started. Strengthening regimens ultimately need to move away from the plinth to more functional activities, such as single squats and lunges, with an emphasis on proper pelvic and core stabilization [26,33].
Finally, the maintenance phase focuses on returning patients to their respective activities with confidence in their functional abilities. In this phase, athletes are ideally observed or videotaped in their sporting environment. Frequently, runners have form deviations that lead to uncontrolled valgus–internal rotation of the knee. These abnormalities include excessive pronation, inability to shock attenuate at the knee, and Trendelenburg frontal plane gait at the pelvis [33,36]. A change to shock-absorbing or motion-control shoes can accommodate supination and overpronation, respectively [36]. Foot orthoses have also been advocated for runners with lower limb injuries. Their benefit is as yet empirical. Cyclists can often correct their ITB problems with equipment and bicycle adjustments [24,28]. Dancers performing rond de jambe or grand plié can be cued on maintaining turnout and neutral pelvic position [34]. After sports-specific adjustments have been made, athletes need to be reintroduced to activity gradually and individually.
Procedures
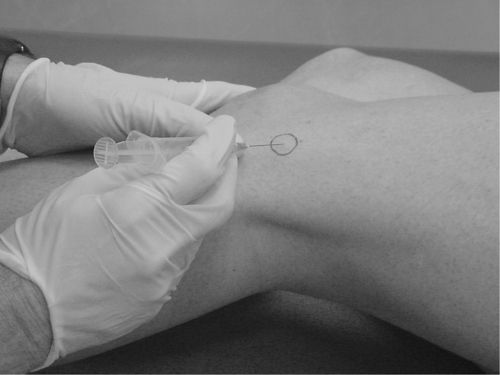
Corticosteroid injections may be performed at different locations along the ITB. Injection into the anatomic pouch at the lateral femoral epicondyle is a relatively simple procedure and is advocated for patients with persistent pain and swelling (Fig. 69.6) [25]. A mixture of anesthetic (e.g., 1 mL of 1% lidocaine) and long-acting steroid (e.g., 1 mL of betamethasone) is instilled to the affected site. A randomized controlled study evaluating the efficacy of corticosteroid injections in runners with acute symptoms of ITB-mediated pain showed that runners in the injection group experienced less pain during running activities [42]. Steroid injections should be repeated only if adequate relief is obtained after the initial injection. Patients can return to play as their pain allows.
Surgery
Surgical treatment of ITBS is rarely needed. Surgery involves excision of the posterior half of the ITB where it passes over the lateral femoral epicondyle, Z lengthening, or removal of the underlying putative bursa by open or endoscopic techniques [12,43,44]. These procedures appear to have mixed results and should be contemplated only for patients who have exhausted all other options, including a comprehensive rehabilitation program as previously outlined.
Potential Disease Complications
If ITBS is not properly addressed, biomechanical adaptations can occur [32]. Chronic pain, leading to progressive disability, is a potential complication.
Potential Treatment Complications
Rehabilitation complications are rare. Nonsteroidal anti-inflammatory drugs and analgesics have well-known side effects that may affect gastrointestinal, hepatic, or renal function. Corticosteroid injections have the potential complications of infection, depigmentation of skin, and flare of symptoms at the site of injection. Surgical procedures for ITBS carry inherent risks. Postoperative infection and other standard risks should be explained to patients before surgical interventions. Overall, interventional procedures for the ITB carry few risks or complications.







