CHAPTER 68
Hamstring Strain
Omar M. Bhatti, MD; Beth M. Weinman, DO; Anne Z. Hoch, DO
Definition
Hamstring strains are among the most common muscle injuries, particularly in athletes. Hamstring strains increase in incidence with age and are most common in football, soccer, and sports that require sprinting. The hamstrings consist of three muscles: the semimembranosus and semitendinosus muscles medially and the long and short heads of the biceps femoris muscle laterally.
Hamstring strains constitute a range of injuries from delayed-onset muscle soreness to partial tears to complete rupture of the muscle-tendon unit [1]. Injuries can occur from direct or indirect forces. Direct forces refer to lacerations and contusions. Complete avulsion of the proximal hamstring origin from the ischial tuberosity has been described, most commonly in water-skiers [2,3]. These injuries occur when forced hip flexion is sustained while the knee remains in complete extension.
Most hamstring injuries, however, occur from indirect forces with exertional use of the muscles, such as running, sprinting, and hurdling. Most hamstring injuries occur at the myotendinous junction during eccentric actions when the muscle lengthens while developing force, most commonly in the lateral hamstrings [4]. The biceps femoris has two heads with different origins and dual innervation and is therefore considered a “hybrid” muscle [5]. Dyssynergic contraction of the muscles is one of many proposed etiologic factors predisposing the hamstrings to strain. Other proposed etiologic factors include the hamstring’s being a two-joint muscle, insufficient hamstring flexibility (Fig. 68.1), insufficient warm-up and stretching before activity, strength imbalance between the hamstrings and quadriceps, strength imbalances between the right and left hamstrings, previous injury to the hamstring, higher running speeds, and poor strength or endurance of the hamstrings. Hamstring strains can occur in a variety of patients from young to old and in any level of athletics from the “weekend warrior” to the elite athlete.
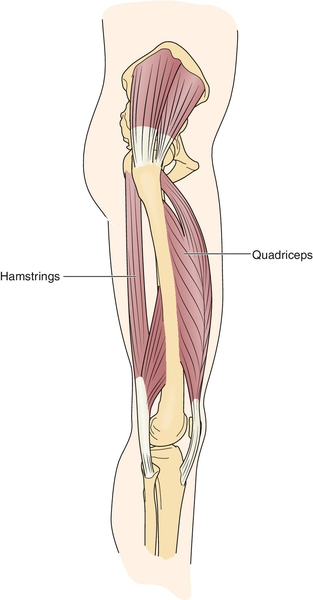
The hamstrings function over two joints. Like other biarticular muscle groups, such as the quadriceps femoris, the gastrocnemius, and the biceps brachii, the hamstrings are more susceptible to injury. The hamstrings cross the hip and knee joint (with the exception of the short head of the biceps femoris). During the latter part of the swing phase of gait, the hamstrings act eccentrically to decelerate knee extension; and at heel strike, the hamstrings act concentrically to extend the hip. During running, this rapid change in function puts the muscle at risk for injury; the higher the running speed and angular velocity, the greater the forces at heel strike [6,7]. Any large strength imbalance between the larger and stronger quadriceps and the hamstrings will put the hamstrings at a disadvantage. If the synergy of antagonists is altered, a vigorous contraction of the weaker muscle may result in injury. Any factor that adversely affects the neuromuscular coordination during running, such as lack of proper warm-up, poor training, or muscle fatigue, may result in a strain injury.
Hamstring strains can be divided into three grades according to their severity:
2. Grade II, or second-degree, strain: moderate strain with more severe partial tearing of the muscle but no complete disruption of the myotendinous unit. Pain is present with loss of knee flexion strength.
3. Grade III, or third-degree, strain: severe strain involving complete tearing of the myotendinous unit. This injury presents with severe pain and marked loss of knee flexion strength [1,8].
Avulsion of the hamstrings tendon from its origin on the ischium or distally from the tibia or fibula is not graded like the classic myotendinous strains. These injuries are usually complete or partial avulsion injuries and described as such.
Symptoms
At the time of injury, patients typically report a sudden, sharp pain in the back of the thigh. Some describe a “popping” or tearing sensation. There is generalized pain and point tenderness at the site of injury. The patient may complain of tightness, weakness, and impaired range of motion. Depending on the severity of the injury, the individual may or may not be able to continue the activity and occasionally is unable to bear weight on the affected limb. Swelling and ecchymosis are variable and may be delayed for several days. The ecchymosis may descend to the thigh and be manifested at the distal thigh or back of the knee, calf, or ankle. The injury may occur in the early or late stages of activity, and patients may give a history of inadequate warm-up or fatigue.
Rarely the patient may complain of symptoms of numbness, tingling, and distal extremity weakness. If these are present, further investigation into a sciatic nerve irritation is warranted. Complete tears and proximal hamstring avulsion injuries can cause a large hematoma or scar tissue to form around the sciatic nerve [9,10].
Alternatively, any change in training patterns and increased eccentric exercise in a previously untrained subject can lead to hamstring injury with delayed-onset muscle soreness. This is thought to be the result of microscopic damage followed by a local inflammatory response [11].
Physical Examination
The physical examination begins with assessment of gait abnormalities. Patients with hamstring injuries often have a shortened walking gait or running stride associated with a limp. Swelling and ecchymosis may not be detectable for several days after the initial injury, and the amount of bleeding depends on the severity of the strain. Unlike direct muscle contusions, in which the ecchymosis remains confined to the muscle proper, the bleeding in a hamstring strain can escape through the ruptured fascia with resultant ecchymosis into interfascial spaces, explaining the common finding of ecchymosis distal to the site of injury [12].
The posterior thigh is inspected for visible defects and deformity, asymmetry, swelling, and ecchymosis (Fig. 68.2). The entire length of the hamstrings should be palpated, including the proximal origin near the ischial tuberosity and distal insertions at the posterior knee. A palpable defect in the posterior thigh indicates a more severe injury with possible complete rupture of the muscle.

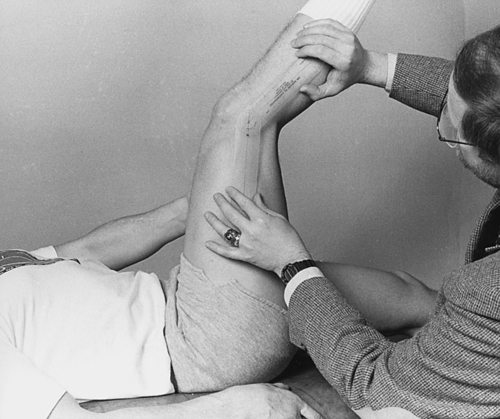
Active and passive range of motion of the hamstrings should be tested and compared with the contralateral side. Range of motion of the knee can be measured with the hip at 90 degrees in the supine position or sitting position. Deficits in knee and hip range of motion are common, and the point at which pain limits range of motion should be noted (Fig. 68.3). Concentric and eccentric muscle strength testing of the hamstrings should also be performed with the patient both sitting and prone. Weakness of knee flexion and hip extension is common. Asymmetry of the hamstrings can sometimes be accentuated with active-resisted static muscle contraction. A soft tissue defect with distal bulging of the retracted muscle belly indicates a partial or complete rupture.
Neurologic examination findings should be normal except for strength testing of the hamstring group and in rare cases when there is an associated sciatic nerve irritation. In these cases, there may be weakness, particularly notable in plantar flexion, and loss of the affected Achilles reflex.
Functional Limitations
Most patients sustaining a hamstring strain have no residual deficits and return to their previous level of function. However, others may experience difficulty with walking or running, time lost from occupation, and delayed return to sports. Hamstring strains heal slowly and are at high risk for reinjury if return to activities is too early. With severe injuries, it may take up to 1 year for patients to resume preinjury activities; in some cases of complete ruptures, patients never return to the previous level of function [13].
Diagnostic Studies
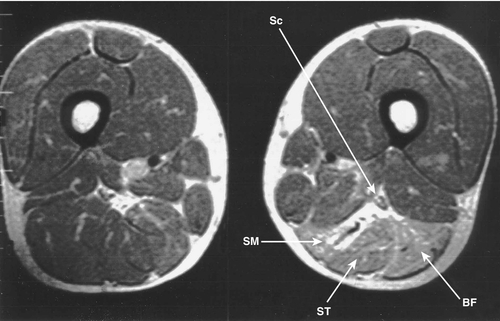
The common hamstring strain usually requires no additional testing because the diagnosis is made by history and clinical examination. However, more severe cases may warrant diagnostic imaging. If the injury localizes near the origin of the hamstrings, plain radiographs may help identify irregularities of the ischial tuberosity, such as a bone avulsion of the ischial tuberosity (especially in the adolescent). Other radiographic findings may include ectopic calcification consistent with chronic myositis ossificans [4,8]. Magnetic resonance imaging may be used to determine the degree of injury and to identify complete proximal avulsion injuries (Fig. 68.4). Ultrasound imaging, in the hands of an experienced practitioner, may also be used as a diagnostic tool.
Treatment
Initial
Initial management of a hamstring strain consists of the PRICE principle (protection, rest, ice, compression, and elevation). Relative rest and protection may involve weight bearing as tolerated or, with higher grade injuries (grade II or grade III injuries), cane or crutch walking. Ambulatory aids help prevent tissue irritation and the resulting inflammation, both of which prolong recovery. Assistive devices should be used until the patient can walk without a limp in a normal heel-toe gait. The application of ice as often as every 2 or 3 hours for 20 minutes the first few days is indicated to limit the amount of pain and swelling. Ice provides an anti- inflammatory effect and helps reduce swelling. Icing is continued through the recovery to inhibit inflammation and to allow muscle healing. Compression by taping or elastic wrapping of the thigh combined with elevation reduces hemorrhage, thereby helping control edema and pain. Nonsteroidal anti-inflammatory drugs and other analgesics are commonly used to limit the inflammatory reaction and for pain control in the first few days. Soft tissue mobilization to the site of pain should be avoided for at least 5 days because this may exacerbate the inflammatory response.
Rehabilitation
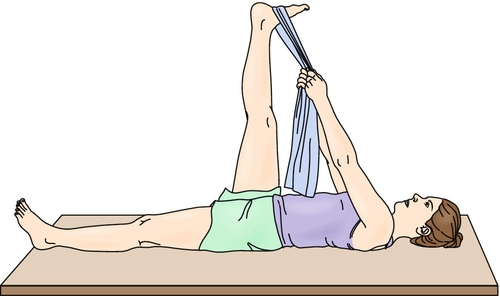
The elements of a hamstring rehabilitation program involve a pain-free progression of stretching, strengthening, and sports-specific activities. In the acute phase, pain-free range of motion should be achieved as soon as possible to prevent adhesions and scarring in the muscle tissue. Patients should start with pain-free active range of motion and progress to pain-free passive range of motion and gentle stretching. For a full stretch of the hamstring muscle to be achieved, the hip must be flexed to 90 degrees and the knee fully extended. This stretch is best achieved in the supine position; a towel can facilitate hamstring lengthening (Fig. 68.5). It is also critical to improve flexibility throughout the spine and lower extremities. Strengthening can begin when the patient achieves full active extension without pain. It is best to start with static contractions, such as multiple-angle submaximal isometric exercises [14]. Once these are performed at 100% effort without pain, the patient may progress to isotonic exercise, such as prone hamstring strengthening and isokinetic exercise. These concentric strength exercises are followed by eccentric strength exercises and sports-specific activities as tolerated. Examples of eccentric training include Nordic hamstring exercises, straight-leg windmills, straight-leg dead lift, and flywheel training [15]. Return to sport is allowed when full motion is restored, strength is at least 90% that of the uninjured side, and hamstring-quadriceps strength ratio is symmetric [6]. Hamstring flexibility must be maintained throughout the rehabilitation process to prevent reinjury. Aerobic conditioning should continue throughout the rehabilitation process. Bicycling without toe clips (toe clips increase use of hamstrings), swimming or jogging in a pool, and upper body ergometry are recommended. Rehabilitation programs incorporating progressive agility and trunk stabilization exercising have been shown to decrease reinjury rates [16].
It is critical to educate patients about how to prevent recurrent hamstring injuries. This includes a good warm-up period before engaging in sports. Full return to play must be gradual because the risk of recurrent injury is high. In addition, training errors, such as an abrupt switch to a hard surface or an increase in training intensity, should be avoided.
Procedures
Procedures are not typically performed in hamstring strain injuries. However, the use of platelet-rich plasma to aid in the recovery of high hamstring strains has been gaining popularity [17]. Given the increased use of autologous blood injections and dry needling techniques, further clinical and laboratory research is warranted.
Surgery
Routine hamstring strains do not require surgical intervention and respond well to a conservative rehabilitation program. However, in the case of complete hamstring avulsion from the ischial tuberosity, surgical repair is recommended because of the residual loss of power and function in nonoperatively treated patients [2,3,18]. Surgical neurolysis is also recommended for the rare complication of symptomatic scarring around the sciatic nerve [9,10].
Potential Disease Complications
The most common complication of hamstring strain is recurrent injury. Loss of hamstring flexibility and strength as well as neuromuscular coordination puts the patient at risk for reinjury, especially if the return to activity is before full recovery. The high injury recurrence rate is believed to be due to return to play before full strength is regained in the lengthened hamstring position [19].
Two cases of posterior thigh compartment syndrome have been reported with complete hamstring tears, one resulting from injury alone and one complicated by anticoagulation therapy [20,21]. Complete hamstring tears can also result in substantial scar formation around the sciatic nerve within the posterior thigh. Patients may present with radicular-type symptoms ranging from sensory paresthesias to footdrop.
Patients with chronic complete hamstring avulsion off the ischial tuberosity may complain of pain, weakness, and cramping as well as difficulty in running and walking and poor leg control, especially walking downhill [3].
Potential Treatment Complications
Nonsteroidal anti-inflammatory drugs are known to have gastrointestinal, renal, and liver side effects. Ultrasound therapy should be avoided in the acute treatment of high-degree strains, especially if hematoma formation is suspected, because it may extend the hematoma [21]. Potential complications of surgical repair of an avulsion fracture include sensation loss along the incision site and postoperative sciatica [22].







