CHAPTER 66
Collateral Ligament Sprain
Paul Lento, MD; Venu Akuthota, MD
Definition
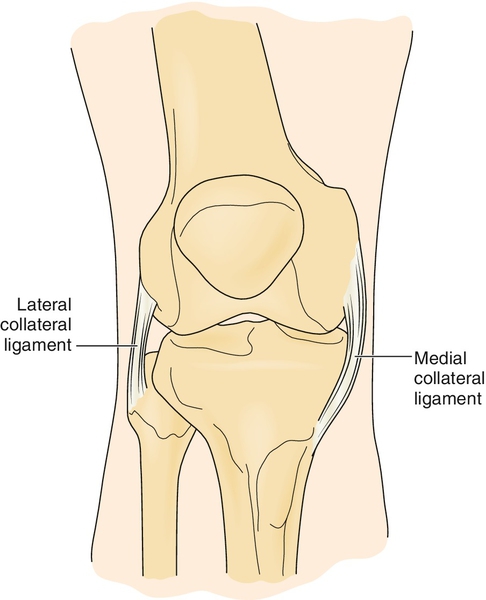
The medial collateral ligament (MCL) and lateral collateral ligament (LCL) are important structures that predominantly prevent valgus and varus forces, respectively, through the knee (Fig. 66.1). Like other ligamentous injuries, knee collateral ligament sprains can be defined by three grades of injury. With a grade I sprain, there is localized tenderness without frank laxity. Anatomically, only a minimal number of fibers are torn. On physical examination, the joint space opens less than 5 mm (i.e., 1 + laxity). With a moderate, or grade II, sprain, there is more generalized tenderness without frank laxity. Grade II sprains can cover the gamut from a few fibers torn to nearly all fibers torn [1]. The joint may gap 5 to 10 mm (i.e., 2 + laxity) when force is applied. A severe, or grade III, sprain, by definition, is a complete disruption of all ligamentous fibers with a joint space gap of more than 10 mm (i.e., 3 + laxity) on stressing of the ligament [2].
Medial Complex Injury and Resultant Instability
The MCL is the most commonly injured ligament of the knee [3]. In fact, injury to this structure has been estimated to occur in 0.24 per 1000 people in the United States in any given year and to be twice as high in males (0.36) compared with females (0.18) [4]. This ligament is usually injured when valgus forces are applied to the knee [5]. Contact injuries produce grade III MCL deficits; noncontact MCL injuries typically result in lower grade injuries. Although MCL injury can occur in isolation, valgus forces typically instigate injury to other medial structures [6]. Findings of a rotational component to medial joint instability should prompt a search for cruciate ligament, meniscal, or posterior oblique ligament involvement [7,8].
Lateral Complex Injury and Resultant Instability
The LCL is much less frequently injured than the MCL. True isolated injury to the LCL is rare. True straight lateral instability requires a large vector force. Thus, a complete knee dislocation with possible damage to neurovascular structures should be suspected if straight lateral instability is present [9]. Posterolateral rotatory instability appears to be a more frequent cause of lateral instability than of straight lateral instability. Most authors believe that posterolateral rotatory instability requires disruption of the arcuate complex, the posterior cruciate ligament, and the LCL. The usual mechanism of posterolateral rotatory instability is forcing of the knee into hyperextension and external rotation [6,9].
Symptoms
Medial or lateral knee pain is the most common symptom related to knee collateral ligament injury. Interestingly, grade I and grade II injuries cause more pain than grade III injuries do [3,10]. Pain is often accompanied by a sensation of knee locking [8]. This may be due to hamstring muscle contraction or concomitant meniscal injury. Patients may also report an audible pop, although this is more common with anterior cruciate ligament injuries [3]. A giving way sensation or a feeling of instability is often reported with high-grade injuries. Moreover, patients with high-grade injuries may also have neurovascular damage [11]. Therefore these individuals may complain of a loss of sensation or muscle strength below the level of the knee [9].
Physical Examination
Physical examination begins with the uninjured knee to obtain a baseline. Palpatory examination can be as important as ligamentous laxity testing. Palpation can reveal tenderness along the length of the collateral ligament, localized swelling, or a tissue defect [8]. Localized swelling correlates well with the area of injury to the MCL [10]. With pure joint line tenderness, an underlying meniscal injury should be suspected. A true knee joint effusion may also be present with collateral ligament injuries; however, it is more prevalent with meniscal or cruciate ligament injury [12].
Laxity of the medial joint ligaments is determined by the abduction stress test (Fig. 66.2A), performed by examination of the knee at 0 and 30 degrees of joint flexion. If the test result is negative, a firm endpoint will be reached. If the test result is grossly positive, the femur and tibia will gap with valgus stress and “clunk” back when the stress is removed [13]. Although it is controversial, increased medial joint laxity of the fully extended knee with a valgus force not only implies damage to the superficial and deep fibers of the MCL but also indicates rupture of the posterior cruciate ligament or posterior oblique ligament [14–16]. If laxity occurs at 30 degrees of flexion but not at 0 degrees, one may confidently conclude that MCL injury is present with sparing of the posterior capsule and posterior cruciate ligament [10,13]. The soft endpoint during valgus stress with the knee at 30 degrees of flexion is the intact cruciate ligament [16]. Although the anterior drawer test is classically used for chronic anterior cruciate ligament tears, it can be a useful adjunctive test for detection of MCL or posterior oblique ligament injury [10].
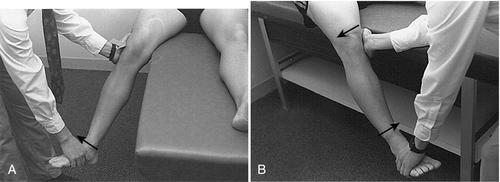
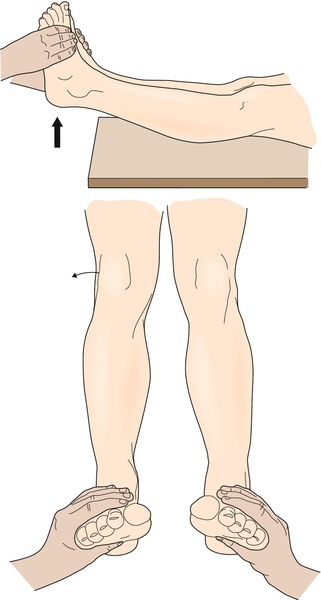
Laxity of the lateral knee joint ligaments is determined by the adduction stress test, which is also performed at 0 and 30 degrees of knee flexion and compared with the opposite “normal” knee (Fig. 66.2B). Gapping of the lateral joint line at 30 degrees of knee flexion indicates damage to the LCL and arcuate ligament complex [12,15]. However, joint opening with the knee in full extension indicates damage not only to the LCL but also to the middle third of the capsular ligament, cruciate ligaments, iliotibial band, or arcuate ligament complex [6,17]. When LCL injury is associated with rotational instability, the reverse pivot shift may be helpful [18]. This maneuver is performed by application of a varus force to an initially flexed knee. A positive test result reveals a clunk as the knee is passively extended from a flexed position. The clunk is a result of the relocation with extension of a knee subluxed in flexion [11,15]. Rotational instability may also be detected by the external rotation recurvatum test (Fig. 66.3).
Functional Limitations
The functional limitations for patients with MCL and LCL injuries result from instability. In general, sagittal plane movements are better tolerated than frontal or transverse plane motions. Most patients with grade III tears of the MCL are able to walk comfortably without an assistive device. Few, however, are able to traverse steps or to do a full knee squat [10]. Patients may also report difficulty with transfers and “cutting” sports activities. Some individuals with posterolateral ligament injuries may have pain with prolonged standing or knee hyperextension. This posterolateral laxity may eventually result in significant genu recurvatum as well as tibia vara, producing pain with even basic activities such as walking and standing [6].
Diagnostic Testing
Plain radiographs are usually normal in acute sprains of the collateral ligaments. Radiographs may be particularly useful to detect avulsion and tibial plateau fractures [7]. For example, an avulsion fracture of the proximal fibula can be detected after a varus-type injury and is associated with posterolateral corner injury, the so-called arcuate sign [19]. Stress views may be indicated in skeletally immature patients for evaluation of physeal injuries [20]. The current “gold standard” diagnostic test is magnetic resonance imaging. Magnetic resonance imaging can detect concomitant injury as well as the severity of collateral ligament damage [21]. Bone bruises not evident on plain films may be detected by magnetic resonance imaging. This can be an important finding, particularly in patients who are experiencing persistent pain. Diagnostic musculoskeletal ultrasound has been used to diagnose and prognosticate injuries of the collateral ligaments and posterolateral corner of the knee [22–24].
Treatment
Initial
After it has been determined whether concomitant injury is present, all grades of collateral ligament injuries are treated initially in the same manner. The basic principles of PRICE (protect, rest, ice, compression, elevation) apply. Immobilization can be used if pain is a significant issue but typically only for a limited time in grade II MCL and LCL injuries [25]. Alternatively, patients with grade II and grade III injuries may need crutches or a hinged knee brace locked between 20 and 60 degrees to provide additional support for an unstable knee, but there is no consensus regarding this [26]. Allowable brace range of motion is increased as tolerated to prevent arthrofibrosis [7,12,27]. Nonsteroidal anti-inflammatory medications may be prescribed to provide pain relief as well as to reduce local inflammation associated with acute injury [28].
Rehabilitation
The goals of rehabilitation for the knee with a collateral ligament injury are to restore range of motion, to increase stability, and to return pain-free activity. Rehabilitation protocols have been described even for grade III MCL injuries [25]. Within the first 24 to 48 hours after injury, static isometric quadriceps contractions and electrical stimulation can be instituted to reduce local tissue swelling and to retard muscle atrophy [13,27]. Range of motion exercises and gentle stretching activities are introduced after the first day [7]. Early weight bearing is also encouraged. Aerobic conditioning can be maintained by use of upper body ergometry, stationary bicycle, or swimming with gentle flutter kicks. Maintenance-phase rehabilitation should emphasize exercise in multiple planes. Rehabilitation should eventually progress to functional or sport-specific activity [25]. A combination of closed and open kinetic chain exercises is used [25,29]. Typically, individuals with mild collateral ligament injuries return to activity after 3 to 4 weeks; patients with grade II and grade III injuries may be able to return to activity after 8 to 12 weeks [30]. Prophylactic hinged knee brace use has been advocated, although effectiveness remains controversial [31–33]. Postsurgical rehabilitation for grade III LCL and MCL injuries with concomitant anterior cruciate ligament, posterior cruciate ligament, or meniscal repair should be at the discretion of the individual surgeon. Variability occurs with each surgeon in respect to immediate weight bearing, protected range of motion, and return to full activity [34].
Procedures
Procedures such as corticosteroid injections have not been studied in acute collateral ligament injuries and typically are not indicated [35]. Needling of symptomatic calcifications within the MCL has been reported [36].
Surgery
The treatment of grade I and grade II injuries of the MCL and LCL is nonsurgical. Grade III injuries, especially when they are associated with concomitant injuries, may be treated surgically. However, most practitioners treat isolated grade III MCL injuries nonsurgically secondary to the high healing rates [3,13,27,37]. Repair of an MCL tear without repair of an associated anterior cruciate ligament injury may lead to a high failure rate [8]. In contrast, grade III LCL injuries or posterolateral complex tears with or without associated cruciate ligament injuries have been shown to heal poorly with nonsurgical measures [7,38,39]. In this case, surgical intervention within 2 weeks, addressing deficits of the arcuate ligament complex, lateral meniscus, and cruciates, provides optimal outcomes [7].
Potential Disease Complications
The most significant disease complication is chronic knee instability. This most commonly occurs with undetected injury to the posterolateral joint complex. Another cited complication is an increased risk of osteoarthritis. Osteoarthritis occurs more frequently with combined MCL and anterior cruciate ligament ruptures than with pure MCL injury [40]. Pellegrini-Stieda disease may also be a rare complication [41]. This condition consists of focal calcium deposition in the area of the injured ligament, typically on the femoral insertion of the MCL. Massage or manipulation may worsen this condition. Instead, calcium reabsorption may be stimulated by dry needling [7,12,36].
Potential Treatment Complications
Analgesics and nonsteroidal anti-inflammatory drugs have well-known side effects that most commonly affect the gastric, hepatic, and renal systems. If the injured knee is immobilized for too long or if range of motion does not proceed in an appropriate fashion, stiffness may result with possible loss of full extension. Similarly, if a surgeon reattaches the deep or superficial components of the MCL to the femoral condyle as opposed to the epicondyle, ankylosis of the joint may result, restricting flexion as well as extension [8].







